Tuberculosis (TB) knows no boundaries. It is a disease not only of the patient as an individual, but also of the community itself. Its control has always transcended the conventional strategies and made it necessary to understand the individual interaction with the social and economic culture. In order to do so, the surveillance programs provide support for evaluation of the burden of TB, the effectiveness of its control and suggested hypotheses for further research.
Considering the importance of active case finding in low incidence settings, an epidemiological study was developed to assess high risk groups for Pulmonary TB cases notified and residing in Coimbra District (Portugal), between 2000 and 2011, contributing to a proper understanding for programmatic approaches.
The study was designed as a retrospective cohort. It was carried out at the Respiratory Diagnostic Centres of Coimbra and Figueira da Foz. There were 556 cases retrospectively enrolled, of which only 339 were identified with antimicrobial susceptibility testing on their clinical records.
Various parameters were analyzed, such as demographic, socioeconomic, and associated diseases data, using descriptive statistics.
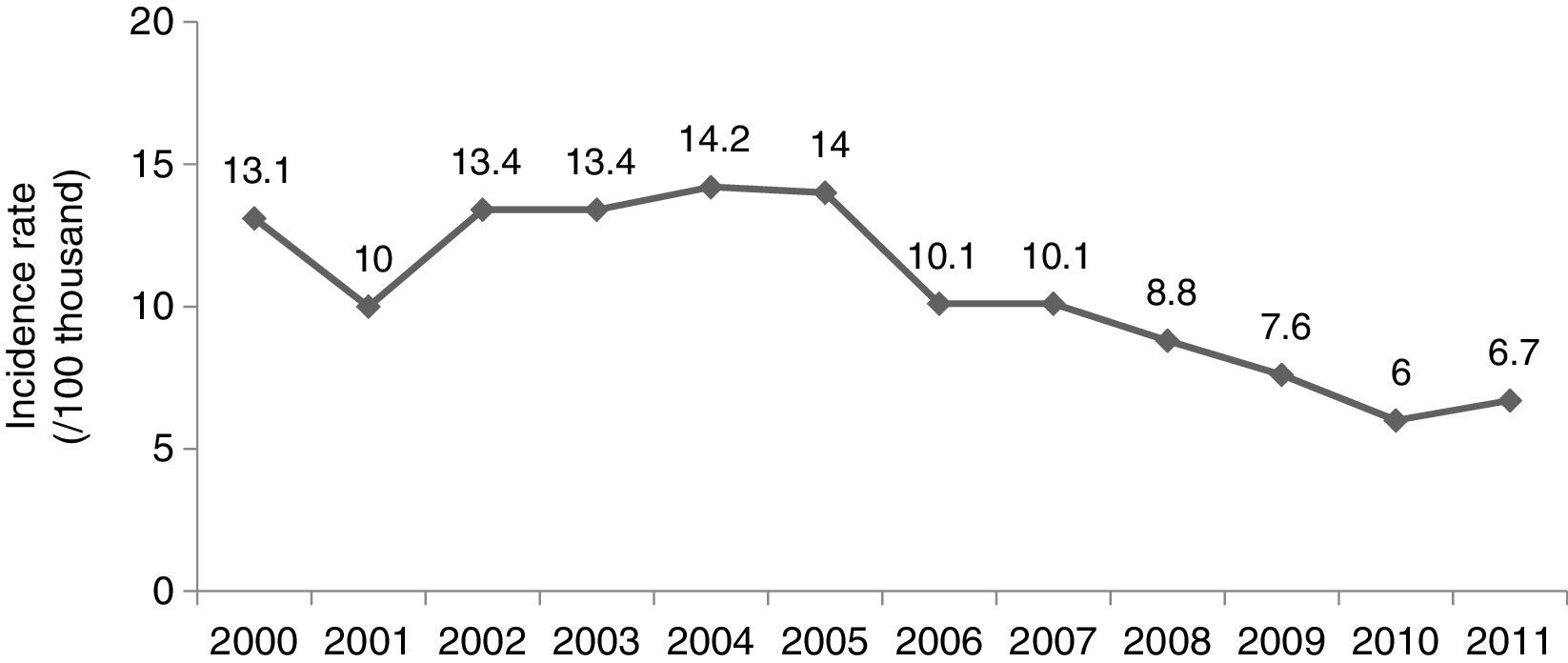
The incidence was the highest in 2004 (14.2/100 thousand). After 2005, it reverted to its previous decreasing tendency until 2010 (Fig. 1). The study population enrolled was 72.3% male (402/556). In 2000 and 2011 the median age was 40 and 47 years respectively. Only in 2000, 2005 and 2006 there were patients reported under 18 years of age (14, 6 and 5, respectively). The annual ratio between men and women peaked at 2.9:1 in 2004, and was lowest at 0.9:1 in 2011.
There were 88.1% (490/556) national and 11.9% (66/556) foreign-born patients reported. The median age was 44 years, and 35 years, respectively. Most of the foreign-born patients were from former Portuguese colonies: Angola (33.3%), Mozambique (10.6%), Cape Verde (9.1%), and Guinea-Bissau (6%).
The three most frequent co-morbidities were human immunodeficiency virus (HIV) co-infection (32/169), diabetes (38/556), hepatitis C virus infection (35/556).
HIV status was registered in only 30.4% (169/556) of the patients reported. Of the 169 patients, 39 were HIV positive, of whom 12 were foreign-born.
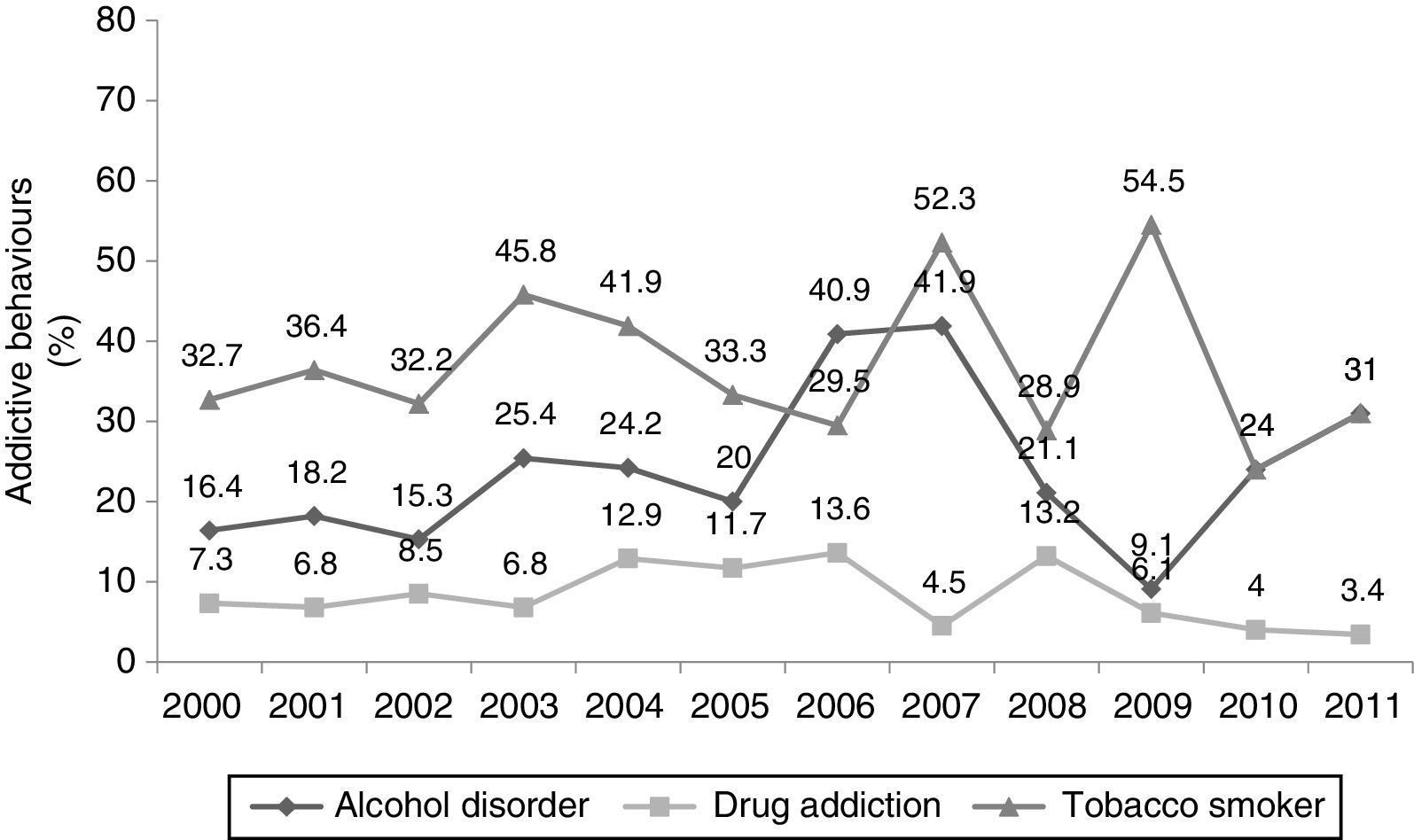
The prevalence of alcohol, tobacco smoke and drug abuse was 23.6% (130/556), 37.3% (206/556) and 8.7% (48/556) respectively. The annual prevalence of alcohol disorder peaked in 2007 (18/43). Among patients with drug addiction, their prevalence peaked in 2006 (6/44). Among tobacco smokers there was a regular trend, which peaked in 2009 (18/33) (Fig. 2).
The highest annual prevalence among residents in community shelters, homeless, and prisoners, was 13.2% (5/38) in 2008, 6.8% (3/44) in 2006 and 9.7% (6/62) in 2004, respectively.
Considering the patients occupations, 10.5% were from teaching institutions of which 86.3% (44/51) were students. Among the health care workers 45.8% (11/24) were nurses.
The incidence increase in the Coimbra District between 2001 and 2004, matches with the national one.1 In 2011 there was a slight incidence increase that the control programs should attend to. However, Coimbra District is one of the lowest incidence regions nationwide.1
There was an increased prevalence among older patients. It decreased among the 25–34 age group, which is typical in low prevalence regions.1 Many active foreign-born TB patients are attributable to the reactivation of latent infection, which is higher during the first 2–5 years following migration.2
The annual ratio between men and women is similar to that seen nationally,1 but in 2011 was at its lowest. Is this episodic or an indicator of some sort of change on the epidemiological profile of the disease?
The patients resistant to at least one first line anti-TB drug peaked at 32.3% (10/31) in 2006. Those susceptible to all first-line anti-TB drugs peaked at 88.5% (23/26) in 2009. There were six patients identified with Multidrug-Resistant TB over the study period; with the highest incidence of 6.9% (2/31) in 2006.
The HIV co-infection is the main immunosuppressive risk factor for developing active disease,3 making HIV counseling and screening for TB patients highly cost/effective.1,4,5 It was not possible to come to a conclusion about the real impact of the co-infection, however there has been a progressive increase in the proportion of patients registered with HIV screening (peaked in 2010 with 42.3%) since 2007 when the directive no. 19/DCSS/PNT of the Directorate-General of Health5 was published. Although these results may have been affected by a selection and classification bias, typical of retrospective studies, the reasons for this under registration should be addressed in order to improve our knowledge of the patient's HIV status.
The annual prevalence of diabetes among the patients was around 10%. It has been recognized as a risk factor for the development of active TB, due to its impairment of the immune responses.3
Although the third most prevalent co-morbidity, considering the eventual and positive impact of HCV treatment available, it can be expected that its prevalence will decrease in the near future among the TB patients.
Healthcare workers are at increased risk of exposure to Pulmonary TB, the nursing staff being the most affected. The infection control measures available to deal with nosocomial transmissions particularly on hospital wards should be one of the main priorities of the health institutions. Naturally, those have to include TB, for obvious reasons (airborne pathogen). Transmission in health services can be significantly reduced with implementation of preventive and control measures, including periodic screening.6
Tobacco smoking, and alcohol are the most prevalent addictions among the patients, which have already been recognized as strong risk factors for the disease.3,7 In Coimbra District among the social factors studied, particular attention is given to the residents in shelters, residence halls and therapeutic communities, with increasing prevalence between 2009 and 2011.
Coimbra District presented what is known as “Epidemiological Transition of TB”, typical features of low incidence regions with a growing proportion of patients corresponding: to immigrants, to older people and to cases resistant to at least one 1st line anti-TB drug.
Today's crisis reminds us that the conditions for TB resurgence (malnutrition, crowded living conditions, addictive behaviors, HIV infection) are still present.
Nowadays the surveillance programs have become even more important as the rates of TB decline, since it tends to be a disease of higher-risk groups. The quality of the information registered and reported to these programs is essential to responsibly adjust local programs and strategies; allowing such assessment, for example, to define risk groups for active screening.
These are reasons important enough to assure a close monitoring of the disease burden.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data, right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to extend our gratitude to Manuel Veloso dos Reis (M.D.), Carla Nunes (Ph.D.) and António Jorge Ferreira (M.D., Ph.D.) for their valuable insight and opinions. Equally, we would like to thank the professionals of the health facilities that in various ways allocated some of their valuable time to collaborate with the study.