Santos et al. have recently characterized hypersensitivity pneumonitis (HP).1 HP is diagnosed based on the patient's exposure history, physical examination (dyspnea, cough, and fever) findings, chest high-resolution computed tomography (HRCT) findings, and bronchoalveolar lavage (BAL). Santos et al. reported that most patients with HP exhibit respiratory symptoms (dyspnea and cough); and ground-glass opacification (GGO) occurred in thoracic CT of 76.7% acute and 91.7% subacute HP cases. HRCT features, including centrilobular diffuse nodules, ground-glass opacification (GGO), and mosaic attenuation, are especially useful for diagnosis.1,2 Although these typical CT patterns are often useful in clinical practice, sometimes, they may also be present in other diseases. Through our recent clinical experience, we wish to highlight a pulmonary intravascular lymphoma with diffuse centrilobular GGO mimicking HP.
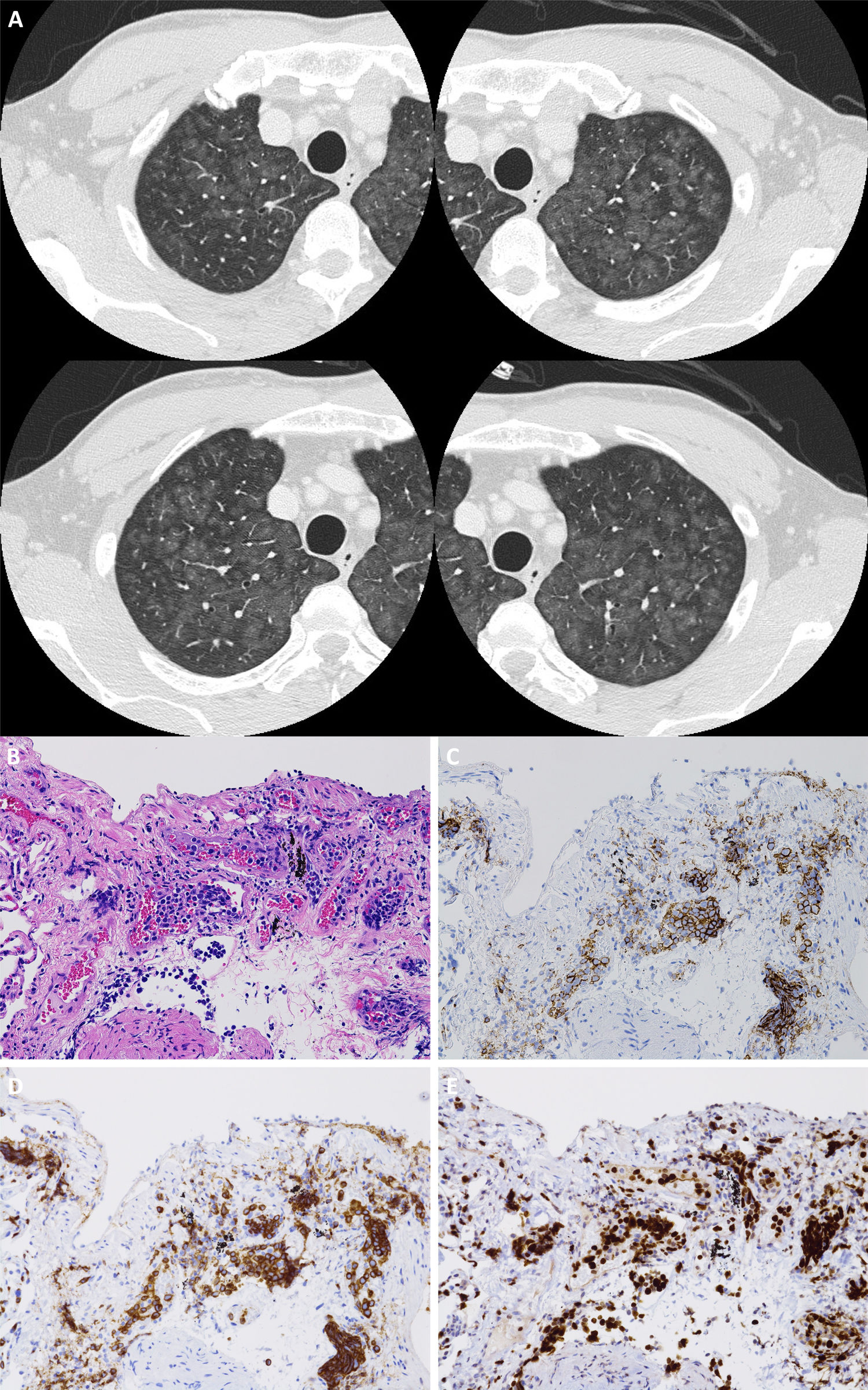
A 61-year-old man with no medical history who was a non-smoker and took no medications was admitted to our hospital with fever (38.5°C), dyspnea, and cough. He had hypoxemia (SpO2 88% at room air) but no crackles. He did not present with extrapulmonary symptoms. Blood tests revealed high C-reactive protein (4.2mg/dL), lactate dehydrogenase (LDH) (923 U/L), and soluble interleukin-2 receptor (sIL-2R) (609 U/mL) levels. Serological tests for anti-neutrophil cytoplasmic antibody and other known autoantibodies against specific antigens were all negative. Chest HRCT revealed diffuse centrilobular GGO and nodules in the bilateral lungs (Fig. 1A). We initially suspected HP based on the respiratory symptoms, CT findings, and history of a dusty air conditioner at the patient's workplace. Although he was observed carefully without receiving steroid therapy to avoid antigens, his symptoms worsened; his LDH and sIL-2R levels increased. We could not perform BAL because of hypoxemia. Histological examination of a transbronchial lung biopsy (TBLB) specimen showed abnormal lymphocytes in the intravascular space of the capillaries (Fig. 1B). Immunohistochemical staining revealed that the tumor cells were positive for vascular antigens, including CD20, CD79α, and Ki-67 (Fig. 1C–E). Based on these findings, we diagnosed pulmonary intravascular large B-cell lymphoma (IVLBCL). Thereafter, he received chemotherapy consisting of rituximab, cyclophosphamide, doxorubicin hydrochloride, vincristine, and prednisolone. His symptoms improved, and the diffuse opacities mostly disappeared.
(A) Chest high-resolution computed tomography revealing diffuse ground glass opacities and nodules with centrilobular augmentation in the bilateral lungs. (B) Microphotographs of the transbronchial lung biopsy specimen. Atypical lymphocytes are seen in the intravascular space of capillary blood vessels. Immunochemical staining revealing that these cells were positive for CD20 (C), CD79α (D), and Ki-67 (E).
IVLBCL is a rare extranodal subtype of non-Hodgkins lymphoma characterized by the selective growth of malignant lymphocytes within the blood vessels, especially in the capillaries, small arteries, and veins.3 The clinical manifestation of pulmonary IVLBCL is nonspecific, and symptoms include fever, cough, and dyspnea.4 The appearance on chest HRCT is varied and can include centrilobular nodules, GGO, and interlobular septal thickening.5 Centrilobular nodules reflect lesions in the bronchioles located at the center of the pulmonary lobules, bronchial arterioles, broad interstitium, and lung parenchyma. In the present case, abnormal lymphocytes had infiltrated the capillary vessels and surrounding space, suggesting that small blood vessels in centrilobular structures can be significantly damaged by intravascular lymphoma. Consequently, we considered that HRCT revealed HP-like pale GGO and nodules with a centrilobular distribution pattern. It is probable that the resulting occlusive proliferation of tumor cells in the vascular lumens led to multiple minor infarctions, which manifested as coughing, dyspnea, and fever.
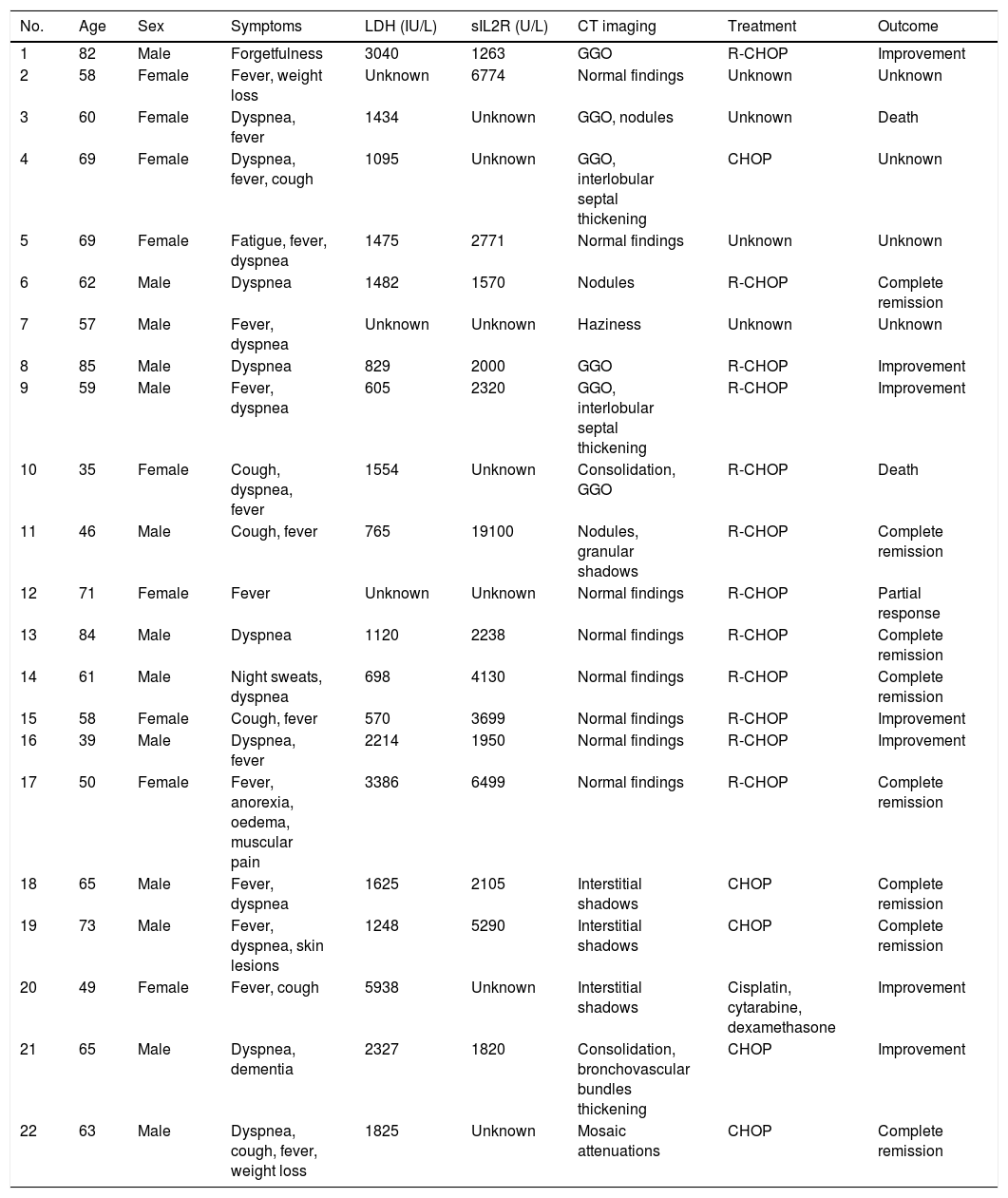
IVLBCL is often not identified during the lifetime, is only diagnosed at autopsy. To the best of our knowledge, only 22 cases, diagnosed by TBLB, have been reported during the past 20 years (Table 1). Respiratory symptoms including dyspnea and cough were present in 18 of those 22 cases, and both LDH and sIL2-R were elevated. Thoracic CT revealed GGO and nodules in some cases but was normal in others, and the response to treatment was mostly good. Based on these findings, TBLB may assist with diagnosis in patients complaining chiefly of respiratory symptoms, and early diagnosis may contribute to improved prognosis. TBLB may also be valuable in the differential diagnosis of other diseases, including HP (particularly acute/subacute HP).
Previous case reports of pulmonary intravascular large B cell lymphoma diagnosed by transbronchial lung biopsy.
| No. | Age | Sex | Symptoms | LDH (IU/L) | sIL2R (U/L) | CT imaging | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| 1 | 82 | Male | Forgetfulness | 3040 | 1263 | GGO | R-CHOP | Improvement |
| 2 | 58 | Female | Fever, weight loss | Unknown | 6774 | Normal findings | Unknown | Unknown |
| 3 | 60 | Female | Dyspnea, fever | 1434 | Unknown | GGO, nodules | Unknown | Death |
| 4 | 69 | Female | Dyspnea, fever, cough | 1095 | Unknown | GGO, interlobular septal thickening | CHOP | Unknown |
| 5 | 69 | Female | Fatigue, fever, dyspnea | 1475 | 2771 | Normal findings | Unknown | Unknown |
| 6 | 62 | Male | Dyspnea | 1482 | 1570 | Nodules | R-CHOP | Complete remission |
| 7 | 57 | Male | Fever, dyspnea | Unknown | Unknown | Haziness | Unknown | Unknown |
| 8 | 85 | Male | Dyspnea | 829 | 2000 | GGO | R-CHOP | Improvement |
| 9 | 59 | Male | Fever, dyspnea | 605 | 2320 | GGO, interlobular septal thickening | R-CHOP | Improvement |
| 10 | 35 | Female | Cough, dyspnea, fever | 1554 | Unknown | Consolidation, GGO | R-CHOP | Death |
| 11 | 46 | Male | Cough, fever | 765 | 19100 | Nodules, granular shadows | R-CHOP | Complete remission |
| 12 | 71 | Female | Fever | Unknown | Unknown | Normal findings | R-CHOP | Partial response |
| 13 | 84 | Male | Dyspnea | 1120 | 2238 | Normal findings | R-CHOP | Complete remission |
| 14 | 61 | Male | Night sweats, dyspnea | 698 | 4130 | Normal findings | R-CHOP | Complete remission |
| 15 | 58 | Female | Cough, fever | 570 | 3699 | Normal findings | R-CHOP | Improvement |
| 16 | 39 | Male | Dyspnea, fever | 2214 | 1950 | Normal findings | R-CHOP | Improvement |
| 17 | 50 | Female | Fever, anorexia, oedema, muscular pain | 3386 | 6499 | Normal findings | R-CHOP | Complete remission |
| 18 | 65 | Male | Fever, dyspnea | 1625 | 2105 | Interstitial shadows | CHOP | Complete remission |
| 19 | 73 | Male | Fever, dyspnea, skin lesions | 1248 | 5290 | Interstitial shadows | CHOP | Complete remission |
| 20 | 49 | Female | Fever, cough | 5938 | Unknown | Interstitial shadows | Cisplatin, cytarabine, dexamethasone | Improvement |
| 21 | 65 | Male | Dyspnea, dementia | 2327 | 1820 | Consolidation, bronchovascular bundles thickening | CHOP | Improvement |
| 22 | 63 | Male | Dyspnea, cough, fever, weight loss | 1825 | Unknown | Mosaic attenuations | CHOP | Complete remission |
References:
1. Kaito S et al. Am J Case Rep. 2019, 2. Yamasaki M et al. Intern Med. 2018, 3. Zhang Y et al. Oncol Lett. 2018, 4. Zhang Y et al. Oncol Lett. 2018, 5. Nada T et al. J Gen Fam Med. 2017, 6. Takeshige T et al. Intern Med. 2017, 7. Wu F et al. Clin Nucl Med. 2016, 8. Yamakawa H et al. Intern Med. 2015, 9. Nishizawa T et al. BMJ Case Rep. 2014, 10. Chen Y et al. J Thorac Dis. 2014, 11. Sekiguchi Y et al. Int J Clin Exp Pathol. 2014, 12. Wagner T et al. Cancer Imaging. 2012, 13. Nakazato T et al. Ann Hematol. 2012, 14. Niida T et al. J Med Case Rep. 2011, 15. Kaku N et al. Intern Med. 2010, 16. Kotake T et al. Intern Med. 2010, 17. Kitanaka A et al. Hematol Oncol. 2009, 18. Asada N et al. Mayo Clin Proc. 2007, 19. Asada N et al. Mayo Clin Proc. 2007, 20. Goh SG et al. Pathology. 2002, 21. Kawamura T et al. Jpn J Clin Oncol. 2001, 22. Walls JG et al. Chest. 1999.
Although the diagnosis of pulmonary IVLBCL is difficult due to its nonspecific clinical manifestation, in cases of diffuse centrilobular GGO and nodules on chest HRCT, it is necessary to consider not only HP but also pulmonary IVLBCL. Moreover, increased serum LDH and sIL-2R levels should suggest a diagnosis of IVLBCL, and TBLB be performed to make a definitive diagnosis.