It is known that patients with heart failure (HF) have an increased risk of developing central sleep apnoea (CSA), with Cheyne-Stokes respiration. The development of servo-ventilation aimed to treat CSA and improve the quality of life (QoL) of these patients. A large randomized clinical study, SERVE-HF, was conducted in order to test this theory in patients with HF and reduced ejection fraction (HFrEF). The results from this trial seemed to indicate that, in these patients, there was no beneficial effect of the assisted ventilation in CSA treatment. More surprisingly, an increased rate of all-cause or cardiovascular mortality was observed. This has led to dramatic changes in clinical practice, with decreased frequency of servo-ventilation prescription across Europe, including Portugal, due to changes in the guidelines. However, SERVE-HF was conducted only in severe systolic HF patients with CSA, and caution must be taken when extrapolating these results to HF patients with preserved ejection fraction or CSA patients without HF.
The study also showed poor adherence, methodological and statistical gaps, including study design, patient selection, data collection and analysis, treatment adherence, and group crossovers, which have not been discussed in the trial as potential confounding factors and raise several concerns. Moreover, the adaptive servo-ventilation (ASV) device used in SERVE-HF was unable to lower the minimum support pressure below 3 mm H20, and this has been suggested as one of the probable contributing reasons to the excess mortality observed in this study. This limitation has since been solved, and this ASV device is no longer used.
This paper describes the results of a Portuguese Task Force on the treatment of central sleep apnoea in patients with chronic HF.
Central sleep apnoea (CSA) is a co-morbidity of chronic heart failure (CHF).1 Servo-ventilation (SV) is a method of ventilatory support designed for Cheyne-Stokes respiration (CSR) in heart failure (HF).2
The effects of servo-ventilation in patients with HF with reduced ejection fraction (HFrEF) and CSA were investigated in a large randomised trial – SERVE-HF.3 Although analysis of the pre-determined primary endpoints – time to first event of death from any cause, life-saving cardiovascular intervention, or unplanned hospital admission due to worsening of HF – was neutral, results showed increased all-cause and cardiovascular mortality.3 These results cannot be extrapolated to HFrEF with other forms of sleep-disordered breathing such as Obstructive Sleep Apnoea (OSA).3,4
The SERVE-HF trial showed poor adherence, methodological and statistical evidence gaps, and further research was needed to better understand its definitions, screening methods and whether and how to treat sleep-disordered breathing (SDB) in patients with HF.5-8 A very interesting commentary explored the methodological issues of the SERVE-HF trial, including study design, patient selection, data collection and analysis, treatment adherence and group crossovers, which have not been discussed in the trial, as potential confounding factors, and raised several concerns.9 Results from a multistate modelling analysis showed that SV was associated with an increased risk of cardiovascular death in patients with HF and Left Ventricular Ejection Fraction (LVEF) ≤ 45% treated for predominant CSA. This risk of cardiovascular death was found to be increased in patients not previously admitted to the Hospital, presumably cases of sudden death, and markedly increased in patients with LVEF<30%.10 However, results from two real world studies showed that most patients treated with SV do not fall into the group of patients at risk, in whom SV is contraindicated.11,12 Moreover, it has been recently shown that the increased cardiovascular mortality reported in the SERVE-HF trial may not be related to worsening of HF.13
A Task Force of the European Respiratory Society (ERS) addressing existing diagnostic and therapeutic standards describes the current practice of CSA treatment in HF.14 Some of the statements were supported by a previous study, which compared the effect of SV with nasal oxygen and CPAP during polysomnography. Results showed large increases in slow-wave and rapid eye movement (REM) sleep with SV but not with oxygen or CPAP.2 In patients with heart disease and preserved left ventricular ejection fraction (pEF), whose treatment of CSA was ASV, a significant reduction of the apnoea-hypopnea index (AHI) was observed. Based on the information available at the time, members of the ERS task force stopped prescribing SV to treat CSA in patients with HFrEF with LVEF≤45% until the publication of results from new studies.14
Novel clinical studies to better understand the real implications of the SERVE-HF trial have been completed or are currently ongoing.
The CAT-HF trial aimed to investigate whether minute ventilation (MV) ASV improved cardiovascular outcomes in hospitalized HF patients with moderate-to-severe sleep apnoea. In these patients, adding SV to optimized medical therapy (OMT) did not improve 6-month cardiovascular outcomes. Detection of the safety signals and identification of the differential SV effects in HF patients with pEF were limitations of this study, which was terminated in 2015.15 Nevertheless, it allowed to conclude that significant reverse left ventricular (LV) remodelling was observed among HFrEF patients with SDB, regardless of treatment allocation. Substantial reductions in left atrial volume among HFrEF and HFpEF patients receiving SV suggests that SV treatment may also improve diastolic function and warrant further investigation.16 A proof-of-concept study showed that treatment of sleep apnoea with SV leads to reduction in atrial fibrillation burden compared with OMT alone, without an increase in ventricular tachycardia/ventricular fibrillation (VT/VF) events. However, this hypothesis should be tested in larger trials.17
The ADVENT-HF (NCT01128816) is an open-label multicentre, randomized study, with blinded assessment of endpoints of standard medical therapy for HFrEF alone versus HFrEF, with the addition of SV in patients with HFrEF and SDB, in both non-sleepy OSA and CSA. Patients with LVEF≤45% are eligible for inclusion.18 The trial is currently under recruitment (the last recruited patient is expected for 2021).
It is the authors’ opinion that the SERVE-HF study was flawed due to the inclusion of HF patients that were too severe, which biased the results since only a small percentage of HF patients fall within this severity group.11,12 The ADVENT-HF is including patients more similar to the ones found in real clinical practice, with less severe HF, and the results, when available, will be of great relevance.7 This paper describes the main conclusions of a Portuguese Task Force for the use of SV in HF patients following the modification of guidelines due to the results of the SERVE-HF trial in 2015.
MethodsA Portuguese Task Force of nine Pulmonologists and Cardiologists, specialized in servo-ventilation in heart failure patients, convened twice to discuss the role of adaptive servo-ventilation as a therapeutic approach of central sleep apnea in heart failure. Based on current clinical guidelines and on relevant scientific papers in the field, the conclusions of this Task Force were agreed upon in 2021.
Problems regarding the prescription of ASVCurrently there are two main problems regarding the prescription of ASV, both directly associated with the results from SERVE-HF: 1) physicians are afraid of prescribing it due to safety issues and 2) after the release of the SERVE-HF trial, in 2015, the Portuguese National Health Authority immediately issued a document recommending withdrawal of SV from patients with the same characteristics as the SERVE-HF population and not prescribing it to new patients.19 These two reasons explain why, although prescription levels of SV have been slowly increasing in recent years, they are far from achieving the prescribing levels before 2015.
Since there are different kinds of SV, being able to analyse the Cheyne-Stokes curve and identify in advance the most suitable type of SV for each patient is crucial, and one of the issues in this identification is the value of the minimum support pressure of the devices. When patients hyperventilate, CO2 levels decrease, which leads to a compensatory decrease in HCO3− to maintain the pH. This alkalosis is associated with hypokalaemia, which may lead to arrhythmia and even cardiac arrest.7 Therefore, when the patient is in a hyperventilation phase, the support pressure should be zero because any pressure above zero will worsen the already existing hypocapnia, with the consequent cardiac alterations. On the other hand, when the patient is in apnoea, the maximum programmed pressure should be used. In fact, the ASV device used in SERVE-HF was unable to lower the minimum support pressure below 3 mm H2O, and this has been suggested as one of the reasons that may have contributed to the excess mortality observed in this study.7,9 This problem has since been solved, and this previous-generation ASV device is no longer used.9
How to overcome the results of the SERVE-HF trial?There is currently a generalized fear of prescribing SV in patients with HFrEF≤45%. Prescription of SV in patients with HFrEF<30% is not an issue since existing data clearly indicates that ASV is contraindicated in this group.10,12 However, the question remains regarding EF values between 30–45%. The fact is that patients were doing well before the results of the SERVE-HF trial and SV is considered to be, overall, a very good treatment, better than CPAP20-22 and with a better adherence to therapy.23 Indeed, a meta-analysis from 2012 that included studies of stable HF patients with LVEF between 20% and 55% concluded that SV was more effective than control conditions in reducing SDB severity and improving cardiac function and exercise capacity in patients with SDB and HF.24
An overall prescription improvement can be observed, but there are still patients who could benefit from SV and are being refused treatment. One of the main reasons is the lack of clarity in the treatment algorithm definition. This might be related to the insufficient level of resources available, which hampers diagnosis and consequently SV treatment.
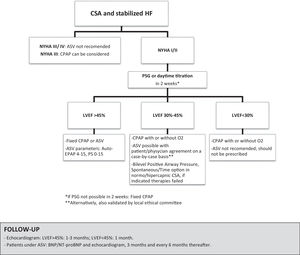
Proposed algorithmIn an attempt to obtain a diagnostic and therapeutic approach for the treatment of CSA in patients with HF, the authors firstly agreed that each patient constitutes a specific case and must always be evaluated individually. In fact, the latest guidelines on SV state that the ultimate judgment regarding any specific care must be made by the clinician.25 The Task Force could not reach a full consensus regarding the proposed approach for the treatment of CSA, mainly due to the different resources of each therapeutic centre, and taking into account that real-world conditions should be adapted to current guidelines. Following these considerations, the available treatment options were discussed, and a diagnosis and treatment algorithm was designed – Fig. 1. The starting point is the referral of patients with controlled and stabilized HF. If the diagnosis of central sleep apnea was performed with a level III sleep study, it is advisable to confirm it with a level I or II PSG as soon as possible. However, it is important to mention that although PSG I/II is considered the gold standard, it is not always easy to achieve, due to practical constraints, and results can take a long time to be obtained. If this is the case, CPAP can be used during the waiting period to PSG. Complementary diagnostic exams must include arterial blood gas analysis, brain natriuretic peptide (BNP), electrocardiogram, and echocardiogram with LVEF evaluation. If the results show an LVEF<45%, the patient evaluation by the Cardiology Department is mandatory. In this case, a new echocardiogram in stable conditions, myocardial scintigraphy, or myocardial magnetic resonance should be performed in selected cases, and the type of HF determined as ischemic or non-ischemic. If NYHA classes III or IV are identified, ASV is not recommended, and medical treatment should be optimized, with CPAP being a possibility for NYHA class III. In case the patient is in NYHA classes I or II, then the recommendations are indicated below.
Pressure adjustmentTitration should be performed during a full-night PSG titration or during daytime ventilatory adaptation. When positive pressure titration is not available within 2 weeks, and if the perceived risk of the continuing sleep apnoeas appears to inflict possible harm to the patient, we recommend a modified protocol of the CANPAP study.26 In this case, fixed CPAP with a low pressure is applied and the pressure is increased in steps of 1-2, up to a maximum of 12 cm H2O. Higher pressures can be considered individually but not higher than 13 cm H2O due to hemodynamic changes. If CPAP is not effective, then other options have to be considered according to LVEF. We do not recommend a split-night study because of the limited titration period.
LVEF- •
LVEF>45%: ASV is recommended, with an auto-EPAP pressure that should be set to the one that corrected the obstructive events. The respiratory rate should be automatic or 2 values below the rest value. The minimum support pressure should be zero, and the maximum should be 15 cm H2O. If EPAP is titrated manually, it is important to mention that one must wait 10-20 minutes before increasing the EPAP pressure (1-2 cm H2O), depending on the respiratory cycle time of the patient.
- •
LVEF between 30-45%: CPAP, with or without O2, is recommended. ASV can be a possibility, considered on a case-by-case basis, in patients without CSR, who sign an informed consent and with medical agreement, as done in several studies.8,12,14,27 Some members of the Task Force recommend that these cases should also be approved by the local ethical committee. If there is no consent, CPAP must be maintained, with pressures adjusted up to a maximum of 12 cm H2O. Higher pressures can be considered in special situations, depending on the case. The Bilevel Positive Airway Pressure, Spontaneous/Timed might be an option only in normo/hypercapnic CSA related to HFrEF, if adequate trials of recommended therapies fail.
- •
LVEF<30%: For CPAP, Bilevel Positive Airway Pressure, Spontaneous/Timed, and oxygen therapy, the same treatment approach as for LVEF between 30-45% should be used. ASV is not recommended in these cases and should not be prescribed. Low flow oxygen therapy can also be an option. Low flow oxygen therapy has been used for decades in the treatment of central sleep apnea and CSR. It has been shown to decrease central sleep apnea and Cheyne-stokes respiration and is recommended by the American academy of sleep medicine. However, the long term effect of low-flow oxygen therapy on morbidity and mortality of HF patients with CSA/CSR is only currently under investigation in a prospective randomized controlled study.28 Therefore, at present, it is not possible to give a conclusive recommendation towards this therapy.
Although new therapy modalities, such as the unilateral phrenic nerve stimulation, have shown promising results in recent publications,29 the task force cannot at present make any recommendations regarding its use.
Follow-upIn cases of LVEF between 30-45% and <30%, there should be a tight control of the patient with frequent monitoring. After treatment initiation, follow-up should be performed in all patients (including those with LFEV>45%) with a cardiac ultrasound, between 1-3 months if LVEF>45% and 1 month if LVEF<45%. If the patient is treated with ASV, BNP levels and an echocardiogram should be performed after 3 months and every 6 months after that.
Final remarksIn conclusion, it is important to remember that in 2013-2014 ASV prescription was the rule, there was no treatment personalization, the methodology lacked importance. Currently, the opposite happens, with the prescription being too rigid due to the results of the SERVE-HF trial, regardless of its numerous flaws. In the future, a more unbiased culture must be adopted when some new treatment is released. Finally, a national registry of patients already exists, but it is not accessible, since the National Health Ministry does not release the data due to data protection. Also, the ADVENT-HF trial is being monitored every 6 months and it has not been stopped, suggesting there are no safety concerns. It is the authors’ opinion that the implementation of the consensual algorithm hereby presented will aid in the clarification of treatment options and therefore help an increased number of patients who would benefit from ASV in Portugal.
FundingThis work was supported by Philips. Funding was used to access all necessary scientific bibliography and cover meeting expenses. Philips had no role in the collection, analysis and interpretation of data, in the writing of the paper or in the decision to submit the paper for publication.