Asthma is the commonest and most important chronic non-infectious disease in childhood and it has become more prevalent in recent years. There is a shortage of studies in relation to early childhood and so, as part of the INAIRCHILD project, this cross-sectional study aimed to assess the prevalence of asthma and its associated risk factors, namely demographic, environmental, psychosocial and clinical factors for infants and preschoolers living in Northern Portugal. Data concerning asthma prevalence were collected through questionnaires based on those from the International Study of Asthma and Allergies in Childhood (ISAAC-derived), the questionnaires were distributed to 1042 children attending the 17 nurseries involved in the INAIRCHILD project (10 in urban and suburban context, and 7 in rural context). The response rate was 48%. Prevalence of asthma based on symptomatology and odds ratio was calculated. Around 52% of the studied children presented at least one of the respiratory symptoms investigated (wheeze, dyspnea and cough) in the absence of upper respiratory infections. The prevalence of asthma was 10.7%, comparable to the figures for Portuguese schoolchildren (6–7 years old) reported by the national Directorate-General of Health, thus showing that an early diagnosis might be possible and helpful for the mitigation of childhood asthma. Environmental context (urban, suburban or rural), gender and family asthma history showed clear associations with asthma prevalence, namely non-rural location, male gender, and having an asthmatic parent were found to be risk factors.
Asthma is the commonest and most important chronic non-infectious disease of childhood and it is estimated that at present time more than 300 million people are affected worldwide.1,2 The prevalence of asthma has increased over the past few decades (it is currently approximately 10% globally) and today is a serious public health issue with a considerable impact on health economics,2–4 being its incidence higher during childhood.2,5 Traditionally, asthma prevalence surveys were based on the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire and mainly focused on children aged 6–7 and 13–14 years old.1,6,7 However, more than half of all cases of persistent asthma start before 3 years old.8 Although in preschool age it is difficult to make a definite diagnosis of asthma, it is worth determining the prevalence and analyzing risk factors for this phenomenon among preschool aged children.9–11 Many risk factors for childhood asthma have been identified, including allergic sensitization, family history of asthma, severe respiratory tract infections, low birth weight, and pollutants such as parental tobacco smoke.1,5,12–14 However, their impact on prevalence trends in infancy and preschool age has rarely been studied.1,9
Thus, as part of the INAIRCHILD project,15 this cross-sectional study aimed to assess asthma prevalence and associated risk factors, namely demographic, environmental, psychosocial and clinical risk factors for infants and preschoolers living in Northern Portugal.
Materials and methodsStudy population consisted of 1042 children attending the 17 nursery schools involved in the INAIRCHILD project (approved by the Ethics Commission of Universidade do Porto and by the Ethics Commission of Hospital de S. João, Porto). These nursery schools were located in urban and suburban contexts in Porto district and in rural context in Bragança district (both in northern region of Portugal). In Porto district 3 and 7 nursery schools were considered, for infants (children aged under 3) and pre-schoolers (3–5 years old) respectively; in Bragança district, there were 2 and 5 nursery schools considered, for infants and pre-schoolers respectively.
Data concerning asthma prevalence were collected through ISAAC-derived questionnaires, distributed in 2013/2014 academic year to all the children attending the nurseries involved. The questionnaire included questions concerning sex, age, height, weight, distance from home to school, socioeconomic status, tobacco smoke exposure habits, family asthma history and health symptoms related to asthma prevalence: asthma previously diagnosed, wheezing, dyspnea and their severity through asthma attacks (number in the previous year, speech-limiting attacks, during night and induced by exercise). Parents or guardians signed participation consent according to the Helsinki Declaration developed by the World Medical Association, and completed the questionnaire. Uncompleted questionnaires were excluded. Questionnaires and their evaluation were validated by medical doctors.
Logistic regression models were used to calculate odds ratios (OR). The level of statistical significance was set at 0.05. Statistical analyses were performed using epicalc package in R software, version 3.1.2.16
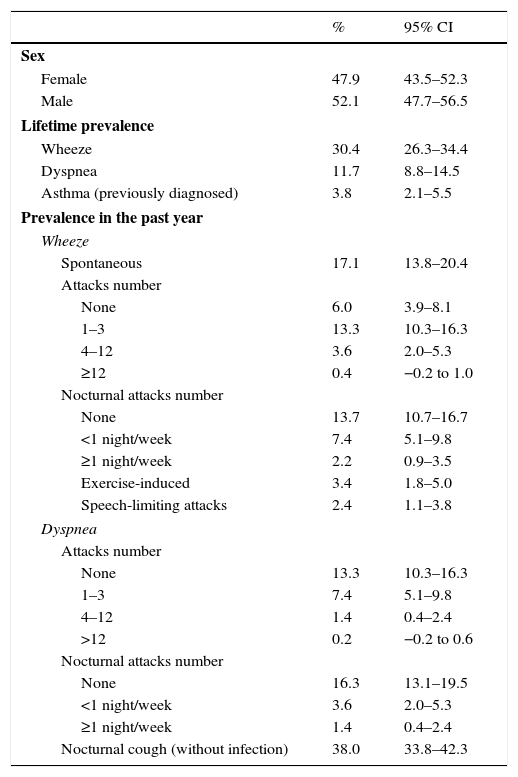
Results and discussionFrom the 1042 ISAAC-derived questionnaires distributed, a total of 497 questionnaires were considered complete for this study (response rate of 48%). Out of those, 197 questionnaires were from children attending nursery schools in Bragança district – rural context, and 160 and 140 questionnaires were from children attending nursery schools in Porto district – urban and suburban context, respectively. The studied population (mean age 3.6 years old) is characterized in Table 1. Around 52% of the studied children presented at least one of the respiratory symptoms investigated (wheeze, dyspnea and cough) in the absence of upper respiratory infections. The prevalence of wheezing for lifetime period and for the past year was 30.4% and 17.1%, respectively.
Characterization of the studied children and prevalence of asthma symptoms (with confidence intervals).
| % | 95% CI | |
|---|---|---|
| Sex | ||
| Female | 47.9 | 43.5–52.3 |
| Male | 52.1 | 47.7–56.5 |
| Lifetime prevalence | ||
| Wheeze | 30.4 | 26.3–34.4 |
| Dyspnea | 11.7 | 8.8–14.5 |
| Asthma (previously diagnosed) | 3.8 | 2.1–5.5 |
| Prevalence in the past year | ||
| Wheeze | ||
| Spontaneous | 17.1 | 13.8–20.4 |
| Attacks number | ||
| None | 6.0 | 3.9–8.1 |
| 1–3 | 13.3 | 10.3–16.3 |
| 4–12 | 3.6 | 2.0–5.3 |
| ≥12 | 0.4 | −0.2 to 1.0 |
| Nocturnal attacks number | ||
| None | 13.7 | 10.7–16.7 |
| <1 night/week | 7.4 | 5.1–9.8 |
| ≥1 night/week | 2.2 | 0.9–3.5 |
| Exercise-induced | 3.4 | 1.8–5.0 |
| Speech-limiting attacks | 2.4 | 1.1–3.8 |
| Dyspnea | ||
| Attacks number | ||
| None | 13.3 | 10.3–16.3 |
| 1–3 | 7.4 | 5.1–9.8 |
| 4–12 | 1.4 | 0.4–2.4 |
| >12 | 0.2 | −0.2 to 0.6 |
| Nocturnal attacks number | ||
| None | 16.3 | 13.1–19.5 |
| <1 night/week | 3.6 | 2.0–5.3 |
| ≥1 night/week | 1.4 | 0.4–2.4 |
| Nocturnal cough (without infection) | 38.0 | 33.8–42.3 |
Based on the answers from the questionnaires, children were considered asthmatic if wheezing and dyspnea were reported simultaneously, or if previously diagnosed asthma was self-reported.17,18 The studied population registered a global asthma prevalence of 10.7%, which is similar to the estimated prevalence (11.0%) for Portuguese children population aged 6–7 years old,19 showing that an early diagnosis might be possible and would surely be beneficial for the mitigation of childhood asthma.
In Chicago, United States of America (USA), Grant et al.20 obtained from ISAAC-derived questionnaires a prevalence of asthma of 10.8% among inner-city kindergarten children (mean age 5.7 years), which was similar to that found in the present study for the same age group (preschoolers). Also in USA, and using a different methodology to obtain data on asthma prevalence (3 national surveys), Akinbami et al.21 reported asthma prevalence in children aged 0–4 years old, lower than in the present study (6.2%) in the period of 2004–2005. In Los Angeles (USA), from new born to 5 years old, asthma prevalence was estimated to be 5.9%,22 lower than that found in the present study; this age group had the lowest asthma prevalence in comparison with the other groups studied (6–11 and 12–17 years old), however having the highest number of emergency room or urgent care visits. In New York State (USA)23 asthma prevalence for the age group 0–4 years old (7.3%) was also the lowest estimated (compared with 5–9, 10–14 and 15–17 years old groups).
Zhao et al.24 studied children in the 3 major cities of China applying also ISAAC-based questionnaires, and registered lower asthma prevalence (3.15% in Beijing, 7.45% in Chongqing, and 2.09% Guangzhou). In a Portuguese study based on a similar methodology, de Sousa et al.25 reported an asthma prevalence of 9.56% for children aged 0–7 years old from Matosinhos (a suburban area in Porto district), slightly lower than the prevalence estimated for the suburban area studied in the present study (also in Porto district).
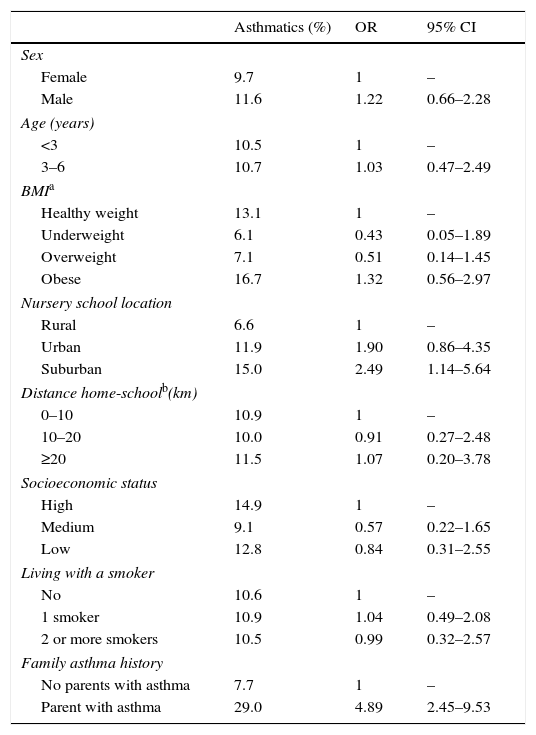
Table 2 shows the distribution of asthma risk factors for the studied children, determined using univariate logistic regression analysis. Odds ratio (OR) and respective 95% confidence interval (CI) are also presented. In the studied population, asthma prevalence was higher for boys than for girls and body mass index (BMI) seemed to be a risk factor for asthma prevalence, with higher risk for obese children (OR=1.32), all results consistent with the literature.21,23 Children attending nursery schools located in non-rural areas (urban and suburban areas) were found to have greater risk (OR=1.90 and 2.49) than in rural areas. Zhu et al.26 also registered lower asthma prevalence in Chinese children aged 5 years old or younger from rural areas (1.33%) than in those from urban areas (2.83%) of Beijing, although both lower than in the present study. In Tennessee (USA), Valet et al.27 studied asthma prevalence in children under 6 years old between 1995 and 2000, and found it higher in rural context (13%) than in suburban (12%) or in urban (11%), which is the opposite to the findings in the present study (6.6%, 11.9% and 15.0%, respectively). However, these comparisons should be made with caution, not only because the methodology for obtaining prevalence in data in that study was different (asthma diagnosis was based on hospital databases and pharmacy claims), but also because the classification of rural context could be different. On the other hand and contrary to what was found in previous studies,24 an increase in asthma prevalence with the age was not found. Additionally, asthma prevalence did not seem to be dependent on distance from home to nursery school. Although socioeconomic status (SES) is a measure of the family's economic and social position in relation to others, based on income, education and occupation,28 the questionnaires did not provide information about income. So, in the present study, SES was estimated merely based on education and parents’ occupation which constitutes a limitation. Results showed higher prevalence for children with high SES, but literature findings suggested the opposite.12 However, the limitations in the results make them uncertain and their interpretation tricky. Although asthma is one of the diseases showing the largest burdens due to environmental tobacco smoke,12 results globally showed that living with smokers did not constitute a risk factor for asthma prevalence, which might have been due to the tendency of adults to avoid smoking in the presence of young children. In fact, Yeh et al.10 concluded that parental smoking was not related to asthma development in early childhood.
Distribution of asthma risk factors for the children studied.
| Asthmatics (%) | OR | 95% CI | |
|---|---|---|---|
| Sex | |||
| Female | 9.7 | 1 | – |
| Male | 11.6 | 1.22 | 0.66–2.28 |
| Age (years) | |||
| <3 | 10.5 | 1 | – |
| 3–6 | 10.7 | 1.03 | 0.47–2.49 |
| BMIa | |||
| Healthy weight | 13.1 | 1 | – |
| Underweight | 6.1 | 0.43 | 0.05–1.89 |
| Overweight | 7.1 | 0.51 | 0.14–1.45 |
| Obese | 16.7 | 1.32 | 0.56–2.97 |
| Nursery school location | |||
| Rural | 6.6 | 1 | – |
| Urban | 11.9 | 1.90 | 0.86–4.35 |
| Suburban | 15.0 | 2.49 | 1.14–5.64 |
| Distance home-schoolb(km) | |||
| 0–10 | 10.9 | 1 | – |
| 10–20 | 10.0 | 0.91 | 0.27–2.48 |
| ≥20 | 11.5 | 1.07 | 0.20–3.78 |
| Socioeconomic status | |||
| High | 14.9 | 1 | – |
| Medium | 9.1 | 0.57 | 0.22–1.65 |
| Low | 12.8 | 0.84 | 0.31–2.55 |
| Living with a smoker | |||
| No | 10.6 | 1 | – |
| 1 smoker | 10.9 | 1.04 | 0.49–2.08 |
| 2 or more smokers | 10.5 | 0.99 | 0.32–2.57 |
| Family asthma history | |||
| No parents with asthma | 7.7 | 1 | – |
| Parent with asthma | 29.0 | 4.89 | 2.45–9.53 |
The factor with highest risk (OR=4.89) was having at least one parent with asthma, confirming asthma family history as an evident risk factor for infants and pre-schoolers.1
ConclusionsResults showed high asthma prevalence in early childhood in Northern Portugal, comparable to that of Portuguese schoolchildren (6–7 years old) reported by the national Directorate-General of Health, thus showing that an early diagnosis might be possible and helpful for the mitigation of childhood asthma. Environmental context (urban, suburban or rural), gender and family asthma history showed clear associations with asthma prevalence, namely non-rural location, male gender, and being the child of an asthmatic parent were found to be risk factors. In the future it could be important to confirm prevalence results through medical exams (e.g. spirometry), and to compare them with asthma prevalence in school children in the same regions which will allow validation of asthma prevalence diagnosis at an early age (infancy and preschool age). It could be also important to extend this to other risk factors.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Authors’ contributionsPTBSB collected field data, structured and drafted the manuscript, performed the statistical analysis and interpreted the results. RAON collected field data and contributed to the background and results sections. MCMAF and FGM contributed to the design of the study and critically revised the manuscript. CF and LGV validated the questionnaires and the results and critically revised the manuscript. SIVS conceived the study, led the study design and coordination, contributed to the interpretation of the results, and critically revised the manuscript. All authors read and approved the final manuscript.
The authors are grateful to the Project UID/EQU/00511/2013-LEPABE, funded by the FCT/MEC with national funds and when applicable co-funded by FEDER in the scope of the P2020 Partnership Agreement; Project NORTE-07-0124-FEDER-000025 - RL2_ Environment&Health, by FEDER funds through Programa Operacional Factores de Competitividade – COMPETE, by the Programa Operacional do Norte (ON2) program and by national funds through Fundac¿a¿o para a Cie¿ncia e a Tecnologia (FCT). The authors are also grateful to project PTDC/SAU-SAP/121827/2010 funded by FCT, COMPETE, QREN and EU; grants SFRH/BD/97104/2013 and SFRD/BPD/91918/2012, for PTBS Branco and SIV Sousa, respectively, funded by FCT, POPH/QREN and European Social Fund (ESF).