Angiomyolipomas are benign mesenchymal tumours that commonly arise in the kidney.1,2,5,7,9 However, they can also occur in extrarenal sites, including the skin, oropharynx, abdominal wall, gastrointestinal tract, heart, lung, liver, uterus, penis, and spinal cord.1,2,5,9 The occurrence of angiomyolipoma in the mediastinum is extremely rare,1-4 with only a few documented cases in the medical literature. This article presents a case of angiomyolipoma detected in the prevascular mediastinum, which was accompanied by recurrent pleural effusion.
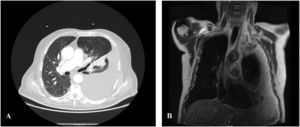
A 78-year-old male presented to our hospital with a large-volume and recurrent left pleural effusion. Cytologic examination of the effusion was negative for malignant cells. Routine haematologic, blood chemical and enzyme tests were within normal limits. Computed tomography (CT) (Fig. 1A) of the thorax revealed a mediastinal pleural mass associated with extensive pleural effusion on the left. Magnetic resonance imaging (MRI) (Fig. 1B) showed a solid, heterogeneous lesion in the mediastinal pleura, with well-defined limits and regular contours, measuring approximately 36 × 23 mm with the longest perpendicular axes. The lesion was mostly isointense on T1 and moderately hyperintense on T2, with central hypointense areas. Additionally, a lesion was identified at the level of the pectoralis major muscle sheath, measuring about 73 × 41 mm in the longest perpendicular axes. The two lesions, although undetermined by imaging, suggested the possibility of schwannomas. A biopsy of the lesion in the pectoralis major muscle sheath was performed, and the morphological and immunohistochemical findings were consistent with a diagnosis of schwannoma.
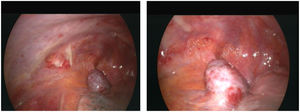
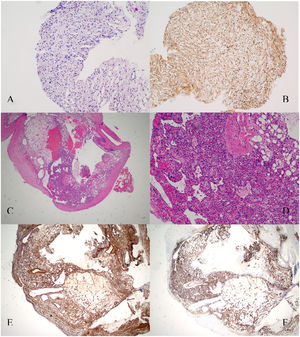
To confirm the cause of the mediastinal lesion, the patient underwent medical thoracoscopy. A hypervascular, sessile mass was observed in the prevascular mediastinum and subsequently biopsied (Fig. 2). The tumour was not separated from the aorta during the procedure. Histological examination of pleural fragments showed vascular congestion, alveoli filled with macrophages, and compression of the alveoli by a fibroadipose tissue 'mass' (MDM2-) and smooth muscle (actin+), accompanied by capillary proliferation (CD34+). Thrombi were frequently present. No necrosis or mitoses were detected. Histochemical investigation for microorganisms, including PAS, Ziehl-Neelsen, and Grocott staining, yielded negative results. Immunohistochemical analysis was performed to explore other neoplasms, and results for calretinin, BER-EP4, S100, CD1a, Melan-A, HMB45, and p53 were negative (Fig. 3)
Histopathology sections. A. Lesion in the pectoralis major muscle sheath. Hematoxylin and eosin staining. B. Lesion in the pectoralis major muscle sheath. Schwann cells are strongly positive for S-100 protein (×10). C. Hematoxylin and eosin staining revealing features of the excised pleural mass with mature adipose tissue, thick-walled blood vessels and smooth muscle cells. Pathological findings of angiomyolipoma. D. 10× magnification. E. Pleural lesion. Smooth muscle actin immunohistochemical showed diffuse positivity smooth muscle cells (×10). F. Pleural lesion. Immunostaining for CD34 antigen revealed many CD34-reactive capillaries combined with mature adipocytes (×10).
Angiomyolipoma of the mediastinum is an exceptionally rare mesenchymal tumour consisting of fat, smooth muscle cells, and abnormal, tortuous, thick-walled blood vessels.1,2,3,6 Although angiomyolipomas are usually found in renal tissue and may be linked to tuberous sclerosis and lymphangioleiomyomatosis (LAM),1,3,6,7 our patient had no prior history of either condition.
Angiomyolipomas are characterised by the expression of melanoma markers (HMB45 and melan-A) in tumour cells, as well as smooth muscle component positivity for muscle actin-specific marker (HHF35) and desmin.2,8 Although the immunohistochemical study did not fully support the diagnosis, the observed morphological features strongly suggest that angiomyolipoma is likely the correct diagnosis, considering its rarity in the mediastinum and the limited number of reported cases in the literature. The histology was reviewed by three different pathologists.
While renal angiomyolipomas typically exhibit a benign behaviour, there have been rare reported cases where they display more aggressive characteristics, including invasion into the renal vein and inferior vena cava.11 Angiomyolipoma of the mediastinum is a recognised variant with malignant potential, as seen in renal angiomyolipomas.3 However, due to the limited availability of long-term follow-up data for mediastinal angiomyolipomas, it remains challenging to fully understand their prognosis and potential for malignant behaviour.
The histology did not show evidence of pleural invasion. The pleural effusion was identified as an exudate and tested negative for malignant cells. The lungs exhibited no signs of lymphangioleiomyomatosis (LAM), and it was considered that the pleural effusion might be reactive.
The management of angiomyolipoma is controversial, and there is limited literature supporting the optimal treatment for pleural angiomyolipoma. However, available literature suggests that small, asymptomatic tumours can be managed conservatively with regular follow-up. For larger tumours with a high risk of spontaneous rupture and bleeding, surgical intervention or selective arterial embolization may be considered as treatment options.3,4,10
In conclusion, while angiomyolipoma in the mediastinum is extremely rare, with only a few reported cases in the literature, it should be considered in the differential diagnosis of mediastinal tumours. Unfortunately, further investigation was not possible as the patient passed away due to a complication of the procedure.
Ethical considerationsWritten informed consent was obtained from the family for publication of the article.