Non invasive ventilation (NIV) is currently employed for weaning from invasive ventilation (IMV) in the acute setting but its use for weaning from prolonged ventilation is still occasional and not standardized. We wanted to evaluate whether a combined protocol of NIV and decannulation in tracheostomized patients needing prolonged mechanical ventilation was feasible and what would be the one-year outcome.
MethodsWe studied patients still dependent from invasive mechanical ventilation with the following inclusion criteria: a) tolerance of at least 8h of unsupported breathing, b) progressive hypercapnia/acidosis after invasive ventilation discontinuation, c) good adaptation to NIV, d) favorable criteria for decannulation. These patients were switched from IMV to NIV and decannulated; then they were discharged on home NIV and followed-up for one year in order to evaluate survival and complications rate.
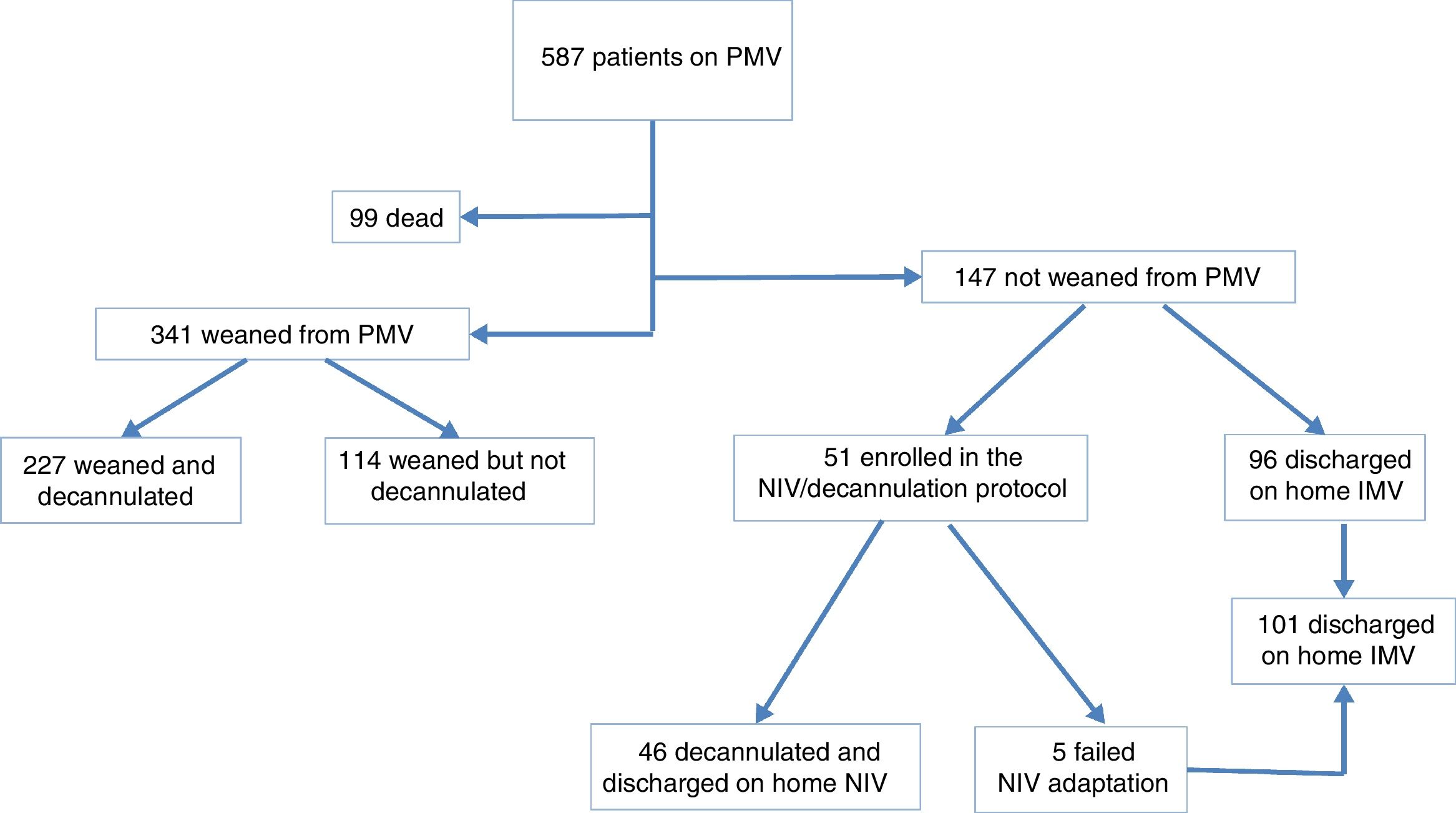
ResultsData from patients consecutively admitted to a weaning unit were prospectively collected between 2005 and 2018. Out of 587 patients admitted over that period, 341 were liberated from prolonged mechanical ventilation. Fifty-one out of 147 unweaned patients (35%) were eligible for the protocol but only 46 were enrolled. After a mean length of stay of 35 days they were decannulated and discharged on domiciliary NIV. After one year, 38 patients were still alive (survival rate 82%) and 37 were using NIV with good adherence (only one patient was switched again to invasive ventilation).
ConclusionsNIV applied to patients with failed weaning from prolonged IMV is feasible and can facilitate the decannulation process. Patients successfully completing this process show good survival rates and few complications.
About 40% of all patients admitted to Intensive Care Units (ICU) require mechanical ventilation, mostly through translaryngeal intubation.1,2 Most patients can be liberated from mechanical ventilation within one week, a smaller proportion requiring tracheostomy and long periods of weaning from mechanical ventilation. According to different definitions,3–5 these patients may represent up to 14% of those admitted to ICU for mechanical ventilation, accounting for 37% of all ICU costs with a hospital mortality up to 38%, significantly higher compared with simple and difficult weaning.6–8
Difficult-to-wean patients may be transferred from acute care hospitals to specialized weaning units, often located within rehabilitation hospitals9 where patients also receive intensive physiotherapy programs,10 in an attempt to regain a satisfactory quality of life.11
A recent systematic review of patients needing prolonged mechanical ventilation reported a 29% and 59–62% hospital discharge and one year mortality, respectively. However, only 19% of patients were discharged home and only 50% were successfully liberated from mechanical ventilation.12
Since non invasive ventilation (NIV) has been shown to shorten the duration of invasive mechanical ventilation (IMV) in patients with chronic obstructive pulmonary disease (COPD), and physiologically to “mimic” IMV,13 there is a rationale for applying it in order to remove the tracheotomy in those patients with incomplete liberation from mechanical ventilation and showing a progressive deterioration in arterial blood gases during spontaneous ventilation. In this study we reviewed data collected prospectively on patients unable to tolerate total unsupported breathing and switched from IMV to NIV and then decannulated, with the aim of assessing the feasibility and effectiveness of this approach and their one year outcome.
MethodsData from subjects consecutively admitted to the weaning unit of the Istituti Clinici Scientifici Maugeri IRCCS, Pavia, Italy, were prospectively collected between May 2005 and January 2018 and retrospectively analysed. Subjects gave written informed consent to the anonymous use of their data for scientific purposes, and the study was approved by the Institutional Ethics Committee (Number 359 CEC on May 2nd 2005).
Setting and study participantsOur weaning unit consists of seven fully monitored beds equipped for mechanical ventilation, located inside the respiratory unit of a multidisciplinary rehabilitation hospital. A 24-h on-duty doctor is available, the nurse-to-patient ratio is 1:4, and the physiotherapist-to-patient ratio is 1:7. Patients can be treated with both NIV and IMV together with a comprehensive rehabilitation program.10 The Italian National Health System refunds a hospital length of stay (LoS) up to 5 weeks.
For the purpose of the study prolonged mechanical ventilation was defined as the need of IMV for more than 6 daily hours for more than 21 consecutive days.4 Patients suffering from end-stage diseases or severe brain damage were not included into the study.
Weaning strategyAt admission patients underwent IMV through tracheostomy by means of an ICU-type ventilator (Nellcor Puritan Bennet 840, Pleasanton, CA, USA or Extend Taema Air Liquide, Antony Cedex, France), with the same setting as prescribed by the sending ICU. Within two hours, arterial blood gases were assessed in order to evaluate the need (if any) of changes in ventilator setting. Within 48h of admission, all patients underwent chemical laboratory tests, collection of urine and tracheal aspirate samples for microbiological analysis, chest X ray, bronchoscopy through the tracheal cannula, another arterial blood gas evaluation and assessment of maximal inspiratory and expiratory pressures (MIP, MEP respectively) (Pony spirometer, Cosmed, Rome–Italy).14
During the following days, when patients were considered stable, (without fever, pain, anxiety, haemodynamic instability or respiratory distress), spontaneous breathing trials were attempted15 with the tracheal cuff deflated, a heat and moisture exchanger filter on the 15mm tracheal cannula connector and oxygen supplementation able to maintain an oxygen saturation as assessed by pulse oximetry (SpO2) monitoring of at least 90%. The spontaneous breathing trial was interrupted in cases of signs or symptoms of distress such as oxygen desaturation (SpO2 less than 90% despite an inspiratory oxygen fraction (FiO2) above 0.40), tachypnea (respiratory rate (RR) higher than 35 bpm), diaphoresis, tachycardia (heart rate above 130 bpm), haemodynamic instability (systolic arterial pressure higher than 180 o lower than 80mmHg). Where any of these conditions were present the patient was connected again to the ventilator and a new spontaneous breathing trial had to be carried out on the following day, if possible.
In absence of the above conditions, patients started increasing periods of spontaneous breathing, until they were able to sustain round-the-clock unsupported breathing.
For data analysis, the patients were categorized in 3 groups (Fig. 1):
Group 1. Patients weaned from IMV: when able to maintain spontaneous breathing over a seven-day period without developing moderate hypercapnia (arterial carbon dioxide tension (PaCO2) above 50mmHg) and/or pH less than 7.33 or any of the above conditions associated to failure.15 When liberated from the ventilator they were considered for tracheostomy removal according to our decannulation protocol based on criteria already described in a previous study.16 According to the absence or presence of these criteria, patients weaned from the ventilator were discharged, in spontaneous breathing, with or without the tracheostomy cannula (Fig. 1).
Group 2. Patients discharged on home IMV through tracheostomy (i.e. whose that after 5 weeks of hospital stay still completely or partially needed invasive mechanical ventilation).
Group 3. Patients switched from IMV to NIV and then decannulated: individuals able to maintain unsupported breathing without signs of respiratory distress but showing:
- •
moderate hypercapnia (PaCO2 higher than 50mmHg), and/or a greater than 5mmHg increase in PaCO2 from the time of suspension of invasive ventilation or
- •
respiratory acidosis (pH less than 7.33) within seven days of spontaneous breathing,
- •
all favorable criteria for decannulation.
These patients underwent the following protocol:
- 1)
fitting a proper NIV mask;
- 2)
downsizing by 1mm the cannula internal diameter without fenestration to leave more pericannular space, in order to facilitate airflow from upper airways during NIV;
- 3)
daytime check of patient tolerance and adherence to NIV with the capped cannula;
- 4)
night-time increasing periods of NIV with the capped cannula, with the aim of at least 4 consecutive hours of NIV. After two nights of good NIV adherence, patients were switched to a domiciliary bilevel ventilator (Astral 100 Resmed, San Diego, CA or Vivo 50 Breas, Mölnlycke, Sweden)
- 5)
daily arterial blood gas assessments, recording of NIV time, checks for air leaks and asynchronies through ventilator microchip analysis (using the dedicated software: ResScan for Resmed and Vivo PC software for Breas).
When all these above steps were successfully completed, decannulation was performed after upper airway endoscopy check and the patient was admitted to a domiciliary NIV program.
In cases of failure of adaptation to NIV, defined as intolerance to interfaces or inability to maintain NIV for at least two consecutive hours, or in cases of persistence of hypercapnia or respiratory acidosis (PaCO2 above 50mmHg and or pH less than 7.33), the protocol was stopped and the patient remained in Group 2 (see above) and was discharged on home IMV.
MeasurementsUpon enrollment into the NIV protocol, the following data were recorded: demographics and anthropometrics; cause of acute respiratory failure; simplified acute physiology score (SAPS) II17; previous ICU LoS; number of comorbidities.
Based on our previous experience,18 patients enrolled into the NIV protocol, underwent re-evaluation of MIP and MEP and respiratory mechanics as described elsewhere,19 in order to acquire more data about the load-force capacity balance of the respiratory system.
Briefly, total cycle duration (TTOT), inspiratory (TI), expiratory time (TE) and duty cycle (TI/TTOT) were calculated from the flow signal, as average values of 5-min periods of continuous recording of flow and volume. Intrinsic dynamic positive end-expiratory pressure (PEEPi,dyn) was recorded and measured as the negative deflection in transdiaphragmatic pressure (Pdi) swings from the onset of inspiratory effort to the onset of inspiratory flow, as described elsewhere.20 Maximal Pdi (Pdimax) was calculated by means of the maximal inspiratory effort generated with a maximal sniff maneuver with verbal encouragement to breathe with the maximal strength.21 The magnitude of the inspiratory muscle effort was estimated from the pressure time product for the diaphragm (PTPdi) and for the inspiratory muscle in toto (pleural pressure time product, or PTPpl). The pressure time integrals were calculated per breath and per minute. The tension-time index of the diaphragm (TTdi) was computed according to the method of Bellemare and Grassino22: TTdi=Pdi/Pdi,max×Ti/Ttot. A value of TTdi higher than 0.15 was considered as an index of respiratory muscle fatigue. All the signals recorded during the measurement of respiratory mechanics were digitized by means of an analog-to-digital converter with a 12-bit resolution (Data Translation 2801/A) and fed into a Pentium processor personal computer at a sampling frequency of 100Hz.
Upon discharge from the weaning unit, the following data were recorded:
1) Weaning unit LoS; 2) number of daily hours spent on NIV.
Follow-upTwelve months after discharge, patients enrolled into the NIV protocol were contacted for a control visit or, in case of inability/unavailability of access to the hospital, for a telephone interview to assess: i-survival; ii-present and time of use of NIV (if any) as self-reported by patients contacted by phone, while in patients visiting our unit it was gathered by the analysis of the ventilator card; iii-adverse events (and causes of) such as hospital admissions or need to switch again to invasive mechanical ventilation.
Statistical analysisStatistical analysis was performed by a dedicated software (STATA 11.2). Anthropometric and clinical characteristics of the patients are described as mean (standard deviation: SD) for continuous variables and as numbers (percentage) for binary or categorical ones. Survival analysis by Kaplan-Maier curve was performed to describe mortality rate over time, and Log-rank test was used to test differences between groups as necessary. Predictive analysis by Hazard Ratio (HR) was used to define the relation between mortality over time and baseline measures (age, gender, SAPS II, ICU LoS, comorbidities, respiratory disease).
ResultsDuring the observation period, out of 587 admitted patients on prolonged mechanical ventilation, 341 were liberated from the ventilator and 227 also decannulated. Fig. 1 shows the flow chart of the study. Fifty-one patients were enrolled in the NIV/decannulation protocol but only 46 were successfully switched from IMV to NIV and decannulated, since five patients failed NIV adaptation (3 patients for claustrophobia despite the use of a nasal mask and two patients for poor adherence and motivation to NIV use).
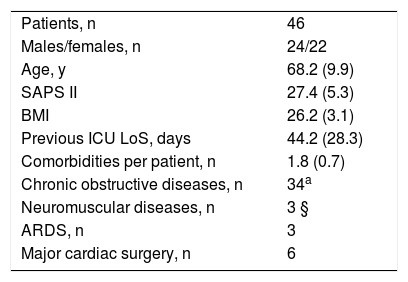
Demographic, anthropometric, physiological and clinical characteristics of patients enrolled in the combined protocol are shown in Table 1. One year survival rate was 82.6% and the only statistically significant HR of one-year mortality was the age (HR=1.089 [1.003–1.183], p=0.041). The 8 deceased patients needed a total of 13 hospital admissions over the follow up period, and the causes of death were sepsis (2 patients), cancer (1), heart failure (3), post-surgical respiratory failure (2). In addition to hospital admissions required for the 8 deceased patients, 6 surviving patients had one hospital admission for acute respiratory failure (4 acute exacerbation of COPD, 2 pneumonias) and were discharged after a mean LoS of 14 (6) days. One patient underwent a new tracheostomy for acute respiratory failure and was discharged home on nocturnal IMV, whereas all the other 37 patients, alive after twelve months were still using NIV for a mean 6.5 (2.2) hours/day.
Demographics, Anthropometric and clinical characteristics of patients. Data are shown as numbers or mean (SD). ARDS, acute respiratory distress syndrome; ICU, intensive care unit; LoS, length of stay.
| Patients, n | 46 |
| Males/females, n | 24/22 |
| Age, y | 68.2 (9.9) |
| SAPS II | 27.4 (5.3) |
| BMI | 26.2 (3.1) |
| Previous ICU LoS, days | 44.2 (28.3) |
| Comorbidities per patient, n | 1.8 (0.7) |
| Chronic obstructive diseases, n | 34a |
| Neuromuscular diseases, n | 3 § |
| ARDS, n | 3 |
| Major cardiac surgery, n | 6 |
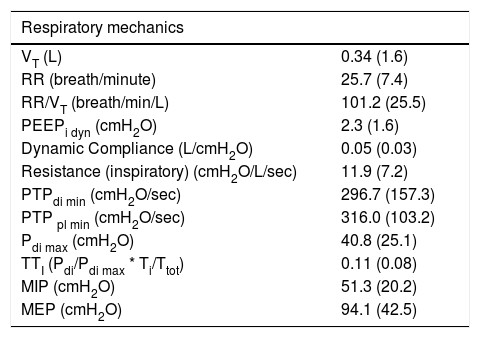
The respiratory mechanics values, shown in Table 2, were recorded for only 30 patients, since 6 patients did not give consent and in 10 patients it was not possible to place the gastric and/or oesophageal balloons. Not surprisingly, most of the patients had a high PTPdi, indicating a considerable burden for breathing, while MIP or Pdimax were quite preserved.
Respiratory mechanics values measured in 30 out of 46 patients. MIP, maximal inspiratory pressure; MEP, maximal expiratory pressure; PEEPidyn, dynamic intrinsic positive expiratory pressure; PTPdi min=pressure/time product /minute of diaphragm; Pdimax=maximal transdiaphragmatic pressure; PTPpl min, pressure/time product/minute of inspiratory muscles; TTDI=tension time index of the diaphragm. Data as mean (SD).
| Respiratory mechanics | |
|---|---|
| VT (L) | 0.34 (1.6) |
| RR (breath/minute) | 25.7 (7.4) |
| RR/VT (breath/min/L) | 101.2 (25.5) |
| PEEPi dyn (cmH2O) | 2.3 (1.6) |
| Dynamic Compliance (L/cmH2O) | 0.05 (0.03) |
| Resistance (inspiratory) (cmH2O/L/sec) | 11.9 (7.2) |
| PTPdi min (cmH2O/sec) | 296.7 (157.3) |
| PTP pl min (cmH2O/sec) | 316.0 (103.2) |
| Pdi max (cmH2O) | 40.8 (25.1) |
| TTI (Pdi/Pdi max * Ti/Ttot) | 0.11 (0.08) |
| MIP (cmH2O) | 51.3 (20.2) |
| MEP (cmH2O) | 94.1 (42.5) |
Mean weaning unit LoS was 35.3 (6.4) days. The mean time needed to complete the NIV protocol (from first day of NIV to decannulation) was 7.2 (2.3) days. None of the 46 patients needed surgical closure of the stoma. Upper airways endoscopy revealed preserved respiratory space in all patients; a rather common finding (almost 30% of cases) was a moderate mucosal introflection on the tracheal cannula convexity in the upper part of the stoma but without tracheal narrowing and, in a few cases (less than 10% of cases), an exaggerated mobility of the pars membranacea towards the anterior tracheal cartilagineous pars with tendency to tracheal narrowing during cough but without the criteria of tracheomalacia. Before discharge, 33 out of 46 (71.7%) patients used NIV only during night-time for a mean of 7.8 (1.6) hours whereas 13 patients (28.3%) were on NIV support also for 2 daytime hours. Nasal masks were used by the majority of patients (n=38), while 8 patients used oral-nasal masks. None of the 46 patients needed cough assist machine during hospital stay or after discharge.
Home bi-level ventilators were set in spontaneous/timed mode with a back-up respiratory rate of 10 bpm and mean inspiratory and expiratory positive airway pressures of 17.1 (2.8) and 4.2 (2.4) cmH2O, respectively. No patient developed face pressure sores due to the interfaces. Arterial blood gases did not differ between the application of IMV or NIV (respectively PaO2/FiO2 245 (83) vs 293 (67), PaCO2 50.4 (11.2) vs 48.2 (8.5), pH 7.40 (0.05) vs 7.40 (0.04)).
DiscussionOur study shows that tracheotomised patients requiring prolonged mechanical ventilation and showing a progressive deterioration in arterial blood gases during periods of spontaneous breathing due to partial dependence on mechanical ventilation, can be switched to NIV and decannulated, showing a one-year survival rate greater than 80%, thus supporting the role of NIV in difficult-to-wean patients. Similar results were reported in a prospective study on patients admitted to Spanish respiratory care units.23 Patients were switched to NIV when it proved unfeasible to increase the duration of spontaneous breathing beyond 18h. Eighty-six % of patients were successfully weaned, out of whom 21% needed NIV during the weaning process. However, this study did not describe the potential use of NIV in the process of weaning from tracheostomy.
The practice of decannulation is very often considered a “risky” procedure by the clinicians, especially those not involved in critical care practice, who therefore are very reluctant to perform it, especially in patients being ventilated for a long period of time, where the occurence of progressive arterial blood gases deterioration is real. This concern is perfectly understandable for safety reasons, but it may worsen the patients quality of life.24
Ours is the first systematic study in a heterogeneous population to assess the feasibility and safety of tracheotomy removal in patients at high risk of procedure failure, since not fully weaned from mechanical ventilation. Decannulation is generally considered the final step of the whole process of liberation from prolonged IMV. Despite the existence of some individualized, non-comparative and non-validated decannulation protocols, universally accepted guidelines are lacking, as well as randomised controlled trials on this critical issue. An Italian survey showed absence of agreement about indications and practical performance of decannulation, so that a substantial proportion of patients were discharged home with the cannula still in place although not requiring IMV any more.25 The presence of a tracheal cannula outside a specialized care context can carry significant risks of morbidity and mortality,26 together with a worsening in quality of life,24 hence every effort must be pursued in order to discharge the patient from the weaning units without the cannula.
The data of respiratory mechanics of our patients show that they were not able to sustain completely unsupported breathing, since their load/capacity balance was impaired. Our data show that these patients have a high respiratory load, as indicated by their PTPdi and PTPpl. The comparison with an historical group of patients18 shows in fact lower PTPpl and PTPdi values in patients successfuly weaned from prolonged mechanical ventilation compared to these patients with incomplete weaning. Previous report indicated the RR/Tidal Volume (VT) ratio as a good predictor of weaning success or failure; 27,28 in our patients the mean RR/VT ratio was higher than 100 breaths/min/L, suggestive of a rapid and shallow breathing pattern, thus indicating the tendency to develop alveolar hypoventilation.
Age was the only predictive factor of one-year mortality in our patients, while no association with survival was found with other variables. Age was also found to be a predictor of survival in a recent systematic review conducted in critically ill patients treated with prolonged mechanical ventilation.29
Limitations of the studyOur study has some limitations. This study was not a randomised controlled trial, and, as such, it cannot assess whether our protocol promotes better weaning rates from mechanical ventilation as compared to other strategies. This study reports data from a single institution, therefore, our findings may not be fully representative of similar trends from other weaning units. Furthermore, our small cohort was predominantly composed by COPD patients (74%) and this might suggest that the technique may be suitable for a selected population. On the other side, our analysis provides information on a real life condition. Since the observation period was rather long (almost 13 years) it could be argued that procedures, staff or expertise have changed over the period thus making the results not homogeneous.
ConclusionIn a selected population of patients under prolonged mechanical ventilation and not fully liberated from the invasive ventilatory support, the combined NIV/decannulation protocol was feasible and safe with a good mid-term outcome. Future randomised controlled trials are needed to confirm these results.
Conflicts of interestThe authors have no conflicts of interest to declare.