Increase in cases of tuberculosis have been reported in recent years in several countries, particularly in urban centers and regions with high prevalence of HIV infection.1 With this worldwide resurgence of M. tuberculosis infection, the recognition of complications and sequelae is very important. Patients with pulmonary tuberculosis present a wide range of CT findings, including airspace or interstitial nodules, the tree-in-bud pattern, consolidations, cavitation, fibrosis, bronchial wall thickening, lymph node enlargement, and pleural effusion.2 However, cystic changes associated with pulmonary tuberculosis have rarely been reported, and are among the rarest presentations of this common disease.3–8
The aim of this report was to describe a case of cystic tuberculosis and to perform a review of the previous reports of this uncommon finding. The MEDLINE database was searched for articles that were published between January 1994 and October 2019. All searches were performed using medical subject heading (MeSH) or free text word. We combined search terms for the primary disease (tuberculosis), the diagnostic test (computed tomography) and pattern (cystic disease). We also manually searched the reference lists of the eligible studies.
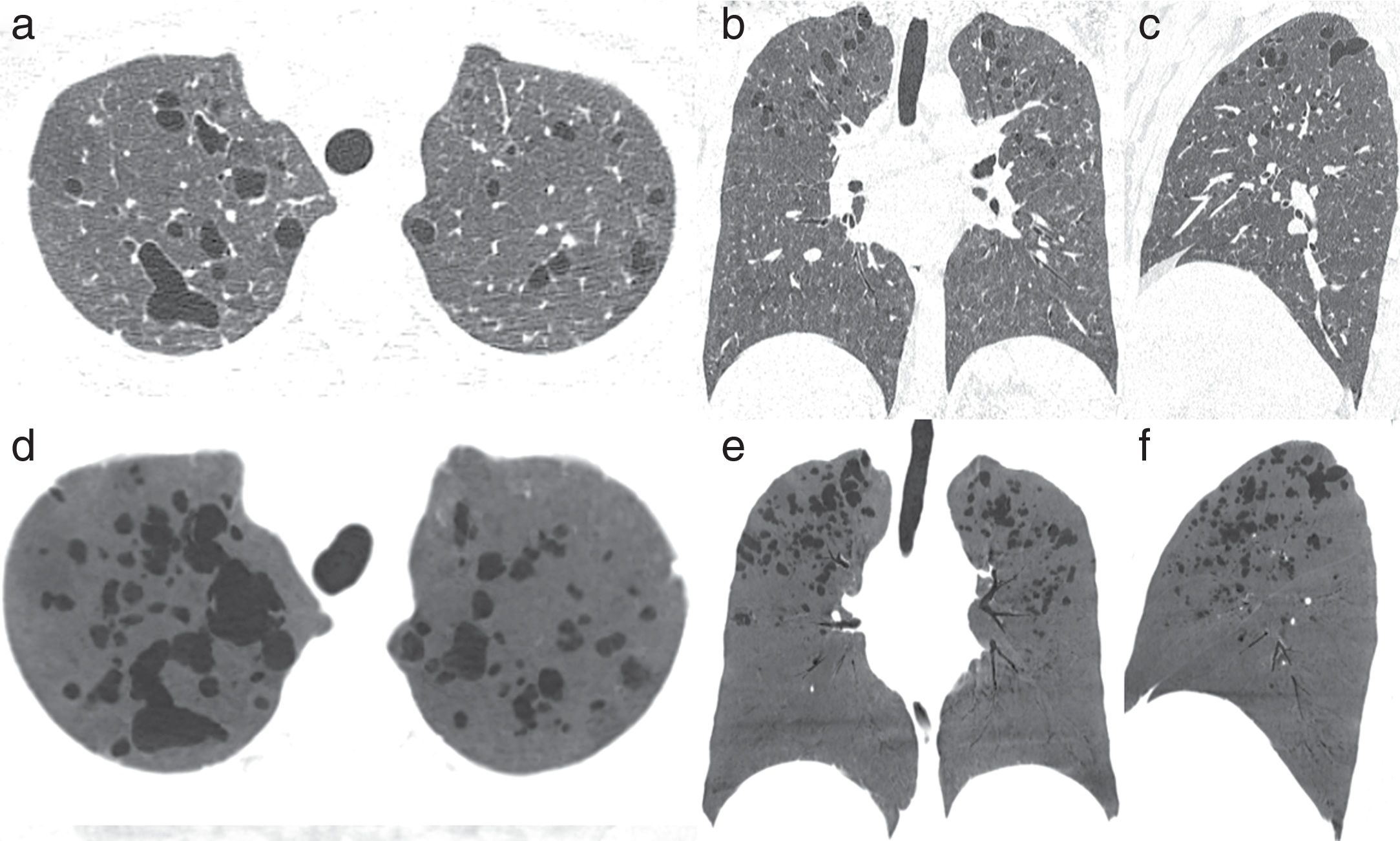
Case reportA 28-year-old homeless woman, a drug-user was admitted to the Emergency Department in an inebriated state under the influence of alcohol. On physical examination, she was found to be disoriented and to have a persistent cough. Her laboratory test results were unremarkable. Chest computed tomography (CT) showed bizarre, irregular cystic formations in the upper regions of the lungs associated with ill-defined centrilobular nodules (Fig. 1). Based on this tomographic pattern, the initial diagnostic suspicion was Langerhans cell histiocytosis.
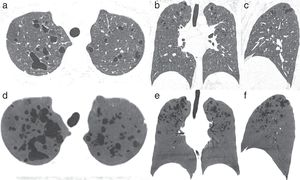
Axial (A), coronal (B), and sagittal (C) reformatted CT images showing multiple thin-walled cysts and ill-defined centrilobular nodules, mainly in the upper lung zones. The cysts have bizarre shapes and a branching appearance. (D–F) Minimum intensity projection reformatted images in the same planes as A–C better demonstrate the thin-walled bizarre cysts.
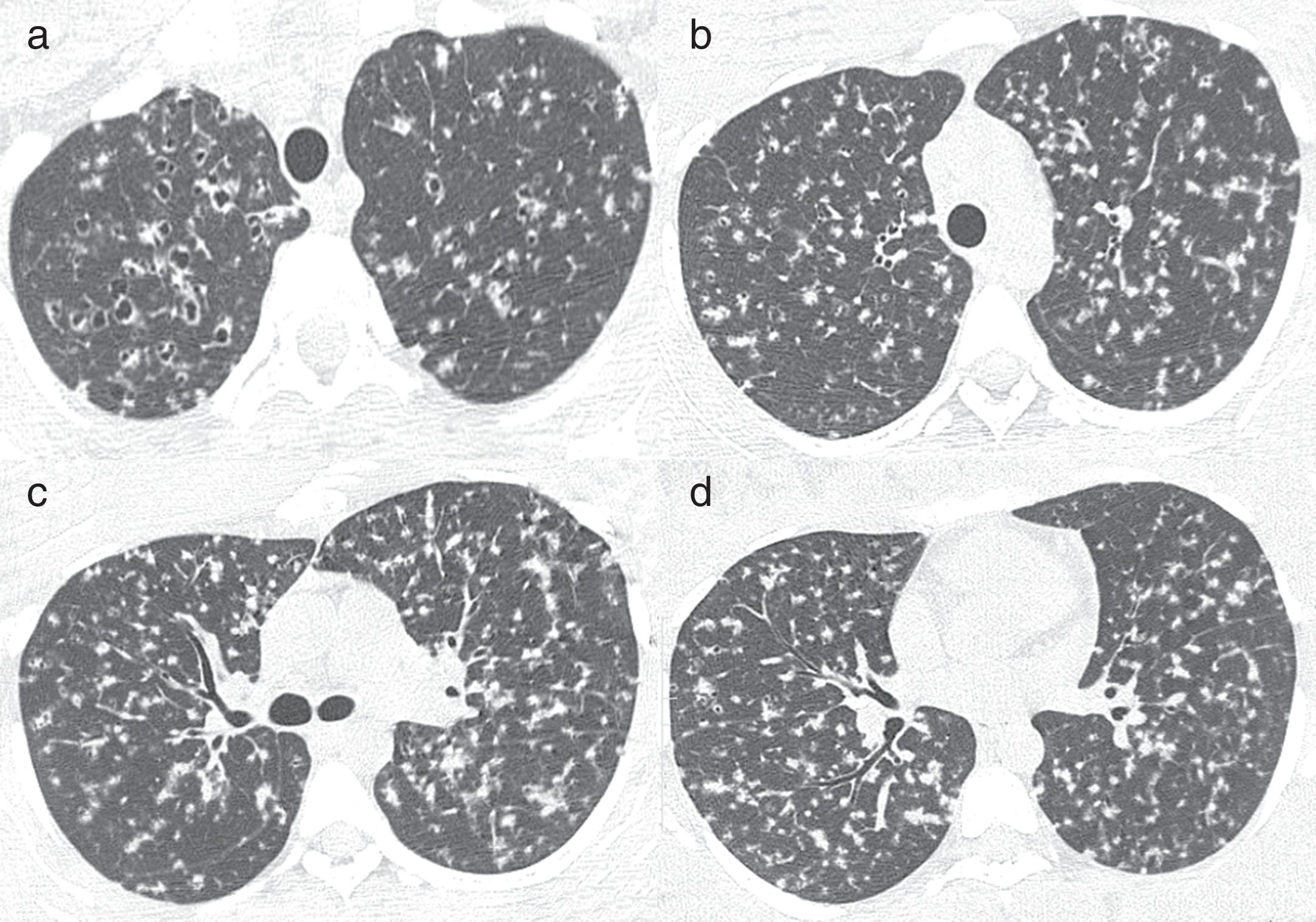
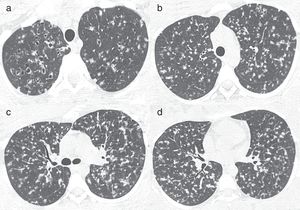
After clinical improvement, when the patient was lucid and oriented, she reported that she had been admitted to a hospital in a nearby city and diagnosed with pulmonary tuberculosis 9 months previously. We contacted the hospital and obtained the following information: the patient presented with complaints of fever for 2 months, productive cough, shortness of breath, asthenia, and 12kg weight loss. The patient’s sputum was positive for acid-fast bacilli, and a culture was positive for Mycobacterium tuberculosis. A human immunodeficiency virus (HIV) test also yielded positive findings. The patient was treated with antituberculous drugs for 6 months. A CT examination performed at that time (9 months before the current examination) showed diffuse multiple small nodules, some of which were cavitated, in the upper lobes (Fig. 2). Thus, the final diagnosis was pulmonary tuberculosis evolving into cystic formations.
Axial CT images obtained 9 months before those presented in Fig.1 show diffuse multiple small nodules, some of which are cavitated, in the upper lobes.
Our patient initially presented with disseminated tuberculosis, which evolved to cystic lesions, predominantly in the upper lung zones. Cystic lesions may develop before or during antituberculous treatment in patients with pulmonary tuberculosis.5 Tuberculosis cysts may evolve with varied outcomes and severity during the course of the disease.4 In some cases, the cysts are reversible and disappear almost completely after antituberculous therapy; in others, the cysts persist after treatment.3,4,6 The rupture of these cystic lesions may cause pneumothorax7 or pneumomediastinum.6
Several mechanisms have been suggested for the pathogenesis of cystic lung lesions due to tuberculosis: a) a check-valve mechanism due to the granulomatous involvement of bronchioles and the excavation of caseous necrotic material by bronchial drainage;3,4–7 b) the communication of tuberculous lesions containing caseous necrosis with the bronchi, resulting in the excavation of necrotic material and cystic changes;7 and c) the cystic lesions representation of areas of dilated bronchioles. Immunohistochemical studies and electron microscopic examinations have revealed that the proteinases secreted from the inflammatory cells of peribronchiolar granulomas are partly responsible for the degradation of elastic fibers along the bronchioles, alveolar ducts, and alveolar walls.5,7
On CT, these cysts appear predominantly in the upper and middle lung zones. The cystic lesions are associated with centrilobular nodules and branching opacities in surrounding areas.2,7 The lesions are irregular in shape, increase in size, and have a tendency to coalesce. The upper zone predominance may be related to the fact that tuberculous lesions are more common in this region.6
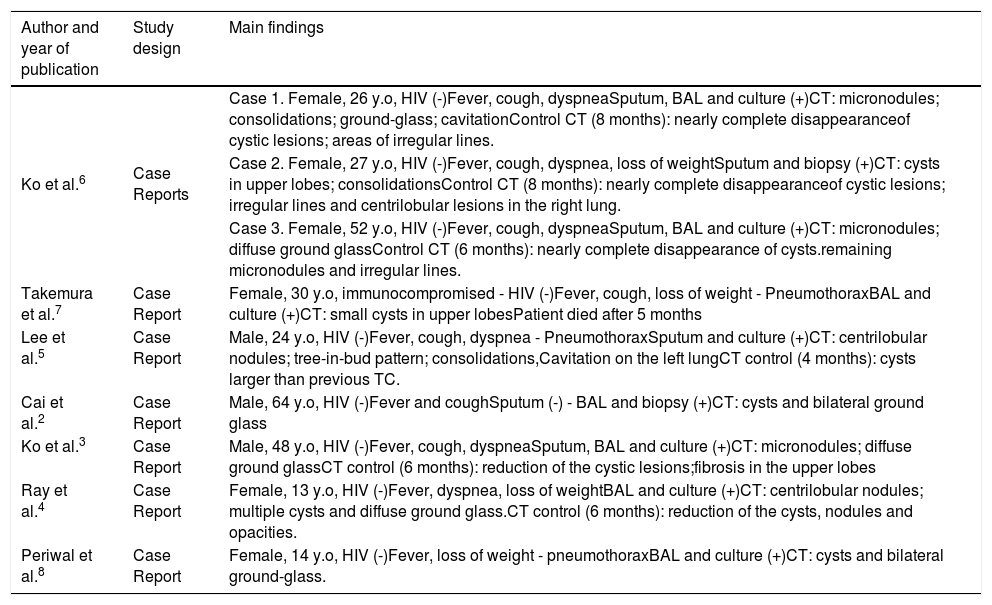
Pulmonary tuberculosis with multiple cysts should be differentiated from various cystic lung diseases, particularly Langerhans cell histiocytosis, lymphangioleiomyomatosis, lymphocytic interstitial pneumonia, and Pneumocystis jiroveci pneumonia,2,6 and from diseases that mimic cysts, such as bullous emphysema and pneumatoceles.4 In the proper clinical context, cystic changes in pulmonary tuberculosis can be easily diagnosed.3 In our patient, the main differential diagnosis was Langerhans cell histiocytosis, particularly because of the upper lobe predominance of the cysts. In summary, pulmonary tuberculosis may on rare occasions present as cystic lung disease and should be recognized as a possible cause of acquired cystic lung disease in appropriate clinical settings (Table 1).
Cases of cystic tuberculosis previously described in the literature.
| Author and year of publication | Study design | Main findings |
|---|---|---|
| Ko et al.6 | Case Reports | Case 1. Female, 26 y.o, HIV (-)Fever, cough, dyspneaSputum, BAL and culture (+)CT: micronodules; consolidations; ground-glass; cavitationControl CT (8 months): nearly complete disappearanceof cystic lesions; areas of irregular lines. |
| Case 2. Female, 27 y.o, HIV (-)Fever, cough, dyspnea, loss of weightSputum and biopsy (+)CT: cysts in upper lobes; consolidationsControl CT (8 months): nearly complete disappearanceof cystic lesions; irregular lines and centrilobular lesions in the right lung. | ||
| Case 3. Female, 52 y.o, HIV (-)Fever, cough, dyspneaSputum, BAL and culture (+)CT: micronodules; diffuse ground glassControl CT (6 months): nearly complete disappearance of cysts.remaining micronodules and irregular lines. | ||
| Takemura et al.7 | Case Report | Female, 30 y.o, immunocompromised - HIV (-)Fever, cough, loss of weight - PneumothoraxBAL and culture (+)CT: small cysts in upper lobesPatient died after 5 months |
| Lee et al.5 | Case Report | Male, 24 y.o, HIV (-)Fever, cough, dyspnea - PneumothoraxSputum and culture (+)CT: centrilobular nodules; tree-in-bud pattern; consolidations,Cavitation on the left lungCT control (4 months): cysts larger than previous TC. |
| Cai et al.2 | Case Report | Male, 64 y.o, HIV (-)Fever and coughSputum (-) - BAL and biopsy (+)CT: cysts and bilateral ground glass |
| Ko et al.3 | Case Report | Male, 48 y.o, HIV (-)Fever, cough, dyspneaSputum, BAL and culture (+)CT: micronodules; diffuse ground glassCT control (6 months): reduction of the cystic lesions;fibrosis in the upper lobes |
| Ray et al.4 | Case Report | Female, 13 y.o, HIV (-)Fever, dyspnea, loss of weightBAL and culture (+)CT: centrilobular nodules; multiple cysts and diffuse ground glass.CT control (6 months): reduction of the cysts, nodules and opacities. |
| Periwal et al.8 | Case Report | Female, 14 y.o, HIV (-)Fever, loss of weight - pneumothoraxBAL and culture (+)CT: cysts and bilateral ground-glass. |
JP, ESP, EM were responsible for the conception and design of the study, and wrote and edited the manuscript. EM contributed to the drafting and revision of the manuscript. All authors read and approved the final manuscript.
Conflicts of interestThe author has no conflicts of interest to declare.
On behalf of all authors, the corresponding author states that there is no conflict of interest.
FundingThis study was undertaken without funding.