Obesity has been associated with respiratory complications, and the majority of these complications occur in the Post-Anesthesia Care Unit (PACU). The aim of this study was to evaluate the outcome and incidence of adverse respiratory events (AREs) in obese patients during their stay in the PACU.
MethodsWe conducted a prospective control study that included 27 obese patients matched with an equal number of patients with body mass index (BMI) <30 (non-obese control group); the 2 groups of patients were similar in respect to gender distribution, age, and type of surgery and had been admitted into the PACU after elective surgery (May 2011). The AREs were identified during PACU stay. Descriptive analysis of variables was performed, and the Mann–Whitney U test, Chi-square test, or Fisher's exact test were used for comparisons. Associations with AREs were studied using univariate and multivariate logistic regression models.
ResultsThere was a higher frequency of STOP-BANG ≥3 (89% vs. 11%, p<.001) among obese patients and they were less frequently scheduled to undergo high-risk surgery (7% vs. 41%, p=.005) and major surgery (4% vs. 15%, p=.008). Obese patients had more frequent AREs in the PACU (33% vs. 7%, p<.018). Multivariate analysis identified obesity and residual neuromuscular blockade as independent risk factors for the occurrence of AREs. Stay in the PACU was longer for obese patients (120min vs. 84min, p<.01).
ConclusionsObesity was considered an independent risk factor for AREs in the PACU. Obese patients stayed longer in the PACU, but they did not stay longer in the hospital.
A obesidade tem sido associada a eventos respiratórios e a maioria destes ocorrem no pós-operatório imediato na unidade pós-anestésica (UPA). O objetivo deste estudo foi avaliar o «outcome» e a incidência de eventos adversos respiratórios (ARE) pós-operatórios em doentes com obesidade durante a sua permanência na UPA.
MétodosEstudo prospetivo caso-controlo com emparelhamento de 27 pares de adultos com obesidade e doentes com IMC <30,0 (não-obesos; grupo de controlo) semelhantes quanto à distribuição do sexo, idade e tipo de cirurgia, admitidos após cirurgia eletiva na UPA (em maio de 2011). Os doentes foram classificados como tendo alto risco de síndrome de apneia obstrutiva do sono (HR-OSA) quando tinham um score de STOP-BANG ≥3. Os ARE foram definidos como obstrução das vias aéreas superiores, hipoxémia (ligeira, moderada e grave), falência respiratória, incapacidade de respirar profundamente, fraqueza dos músculos respiratórios, reintubação e aspiração pulmonar após extubação traqueal. Foi utilizada a análise descritiva das variáveis e os testes de Mann–Whitney U, Qui-quadrado e teste de Fisher foram utilizados para efetuar comparações.
ResultadosO grupo de doentes obesos apresentou uma frequência superior de doentes com um score de STOP-BANG ≥3 (89 vs 11%, p<0,001); foi submetido menos frequentemente a cirurgias consideradas de alto risco (59 vs 0%, p=0,002) e a cirurgias major (4 vs 15%, p=0,008). Apresentou mais frequentemente eventos pulmonares adversos na UPA (33 vs 7%, p<0,018). O evento adverso pulmonar mais frequente foi a incapacidade de respirar profundamente, que ocorreu mais frequentemente nos doentes obesos (26 vs 4%, p>0,025). A análise multivariada identificou a obesidade e o bloqueio neuromuscular residual como fatores de risco independentes para a ocorrência de eventos respiratórios. A duração da estadia na UPA foi superior nos doentes obesos (120min vs 84min, p>0,01).
ConclusõesA incapacidade de respirar profundamente foi o ARE mais frequente no período pós-operatório imediato nos doentes obesos. A obesidade foi considerada um fator de risco independente para ocorrência de ARE na UPA. Os doentes obesos tiveram maior tempo de estadia na UPA mas não tiveram maior tempo de internamento hospitalar.
Obesity is a medical condition that may have several adverse effects on health, leading to reduced life expectancy and/or increased health problems.1 Obesity increases the likelihood of various diseases, particularly heart disease, type II diabetes, and obstructive sleep apnea.1 Obesity is a relatively common condition that can have a profound impact on anesthesia-related morbidity and mortality.
Recent estimates suggest that 60% of the adult population in industrialized countries is overweight (body mass index [BMI] ≥25kg/m2) and at least 30% is obese (BMI ≥30kg/m2).2
The definition of obesity and its clinical significance is well established and is accepted worldwide. Obesity is defined as BMI ≥30kg/m2. This condition is further classified by the World Health Organization (WHO) into classes I, II and III according to the BMI of the patients. Patients are defined as overweight (pre-obese) if their BMI is between 25 and 29.9kg/m2, and obese when it is greater than 30kg/m2.
An increasing number of obese patients undergo surgical procedures. As morbid obesity affects most of the vital organs, the anesthesiologist must be prepared to deal with several challenges.3 Obesity has several pathophysiological consequences, including alterations in respiratory function, and therefore, the perioperative management of these subjects may affect surgical outcomes.
Obesity is associated with excess metabolically active adipose tissue and the consequent increased workload on supportive muscles, which leads to higher oxygen consumption and carbon dioxide production. Other important effects are decreased myocardial compliance, increased work of breathing, and decreased efficiency as more work is spent on lung inflation. Respiratory system compliance and lung volumes, especially the resting functional residual capacity (FRC), tend to be lower in obese patients.4–6 Hence, obese patients tend to have higher respiratory rates in order to compensate for the lower tidal volumes. FRC may decline to less than the closing volume and oxygenation may be affected; patients may be hypoxemic post-induction, possibly due to ventilation-perfusion mismatching at the base of the lungs, where microatelectasis is likely to occur. Postoperatively, decreased lung capacities are expected for at least 5 days and acute airway obstruction is more likely.
Mild hypoxia and adverse respiratory events (AREs) in the postoperative period may be related with postoperative pulmonary atelectasis in morbidly obese patients. In morbidly obese patients, atelectasis may persist for at least 24h whereas it disappears more quickly in non-obese patients.7
Overweight and obesity have been identified as risk factors for postoperative respiratory complications.7–9 Healy et al.10 found that obesity was associated with an increased risk of postoperative respiratory complications in patients undergoing esophagectomy. On the other hand, other studies have found no increased risk attributable to obesity, even in patients with morbid obesity.11,12
The aim of this study was to evaluate the outcome and the incidence of AREs in obese patients during their admission to the PACU.
Subjects and methodsThe Centro Hospitalar São João Ethics Committee approved this study, and written informed consent was obtained from all participants.
This prospective study was conducted in a 12-bed PACU over a 3-week period (from May 9 to May 27, 2011).
Inclusion criteria were the ability of patients to provide written informed consent on admission. Exclusion criteria were patient refusal, inability to provide informed consent, a score of <25 in the mini-mental state examination (MMSE), age under 18 years, foreign nationality, known neuromuscular disease, urgent/emergent surgery and cardiac surgery, or neurosurgery or other procedures that required therapeutic hypothermia.
A case-control design with prospectively defined cases was employed for the study. All obese patients with BMI ≥30 during the study period were identified and matched with selected control patients for comparison. Cases and controls were identified by collecting data on all consecutive patients arriving in the PACU during the study period. The cases consisted of obese patients and were matched with similar subjects in respect to gender, age, and type of surgery, which was defined as intra-abdominal, musculoskeletal, or head and neck. The non-obese patients with BMI <30 were selected on the basis of a one-to-one match with the obese patients and were selected consecutively according to the matching characteristics.
Variables registered on admission in the PACU were as follows: age, sex, type of surgery (intra-abdominal, skeletal muscle, bariatric, head and neck), BMI, American Society of Anesthesiologists (ASA) physical status, and pre-hospitalization comorbidities (specifically obstructive sleep apnea, ischemic cardiac disease, congestive heart failure, cerebrovascular disease, hypertension, renal failure, insulin-dependent diabetes, dyslipidemia, and chronic obstructive pulmonary disease).
Clinical risk factors (history of ischemic heart disease, history of compensated or prior heart failure, history of cerebrovascular disease, diabetes mellitus, and renal insufficiency) were evaluated according to the Cardiac Risk Stratification for Noncardiac Surgical Procedures of the 2007 guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery of the American College of Cardiology/American Heart Association Task Force on Practice Guideline.13
Before surgery, a short interview was conducted to obtain consent, collect the medical history, and to perform an MMSE test. During this interview, the STOP-Bang questionnaire (STOP-Bang)14 was applied. Patients had high-risk obstructive sleep apnea syndrome (HR-OSA) if they had a score equal to or higher than 3.
During surgery, the anesthesiologist in charge was blinded to patient involvement in the study. Conduct of anesthesia and monitoring was done as per the criteria proposed by the anesthesiologist in charge, but followed minimum departmental standards. Neuromuscular blocking drugs were used for tracheal intubation, and additional boluses were given as needed. The use of neuromuscular monitoring was at the discretion of the anesthesiologist, and no written policy existed concerning its use. To ensure that the anesthesiologists remained blinded to their participation in the study, we did not attempt to observe the use or interpretation of Train-of-Four (TOF) intraoperatively. At the conclusion of the surgical procedure, the anesthesiologist was free to take the decision to reverse the neuromuscular blockade (NMB) with neostigmine. According to our practice, this drug is usually administered early before tracheal extubation and at a shallower depth of block.
The patient is usually extubated in the operating room and transferred to the PACU. Criteria for extubation included sustained head lift or hand grip for more than 5s, the ability to follow simple commands, a stable ventilatory pattern with an acceptable arterial oxygen saturation (SpO2 >95%), and a TOF ratio greater than 0.80. All subjects were administered 100% oxygen by a face mask after tracheal extubation. The anesthesiologist was free to decide if oxygen should be administered during the time between transfer to the cart and admission to the PACU.
Upon arrival in the PACU, all subjects received oxygen by either nasal cannula or face mask.
The neuromuscular block was defined as TOF <0.9, and it was quantified at admission to the PACU by using acceleromyography of the adductor pollicis muscle (TOF-Watch®).
The postoperative data registered included information on mortality and the length of hospital and PACU stay.
Postoperative respiratory complicationsEach postoperative ARE was defined on the data collection sheet using the following criteria specified by Murphy et al.15:
- 1.
Upper airway obstruction requiring an intervention (jaw thrust, oral airway, or nasal airway).
- 2.
Mild-moderate hypoxemia (O2 saturation [SpO2] of 90–93%) on oxygen at 3L/min with nasal cannula that did not improve after active interventions (increasing O2 flow to >3L/min, application of high-flow face mask O2, verbal requests to breathe deeply, tactile stimulation).
- 3.
Severe hypoxemia (SpO2 <90%) on oxygen at 3L/min with nasal cannula that did not improve after active interventions (increasing O2 flow to >3L/min, application of high-flow facemask O2, verbal requests to breathe deeply, tactile stimulation);
- 4.
Signs of respiratory distress or impending ventilatory failure (respiratory rate >20 breaths per minute, accessory muscle use, tracheal tug).
- 5.
Inability to breathe deeply when requested to by the PACU nurse.
- 6.
Patient complaining of symptoms of respiratory or upper airway muscle weakness (difficulty breathing, swallowing, or speaking).
- 7.
Patient requiring re-intubation in the PACU.
- 8.
Clinical evidence or suspicion of pulmonary aspiration after tracheal extubation (gastric contents observed in the oropharynx and hypoxemia).
PACU nurses were instructed to review this checklist on each patient after PACU admission and to contact the investigator if any of the described AREs was observed. In such situations, the investigator examined the patient to confirm that the patient met at least one of the criteria for an ARE.
Statistical analysisVariable descriptive analysis was used to summarize the data and Mann–Whitney U test was used for comparison of continuous variables between groups of individuals; Chi square test and Fisher's exact test were used for comparison of proportions between groups of individuals. All variables were considered significant when p<0.05.
To evaluate the determinants of postoperative respiratory complications, a univariate logistic regression analysis was performed and the following independent variables: type of surgery, age, BMI, BMI >35, duration of anesthesia, ASA-PS, high-risk surgery, and diabetes treated with insulin (from RCRI score), type of anesthesia, length of anesthesia, PACU and hospital LOS, and residual neuromuscular block. Multiple regression binary logistics with forward conditional elimination were used to examine covariate effects for each factor in order to identify independent predictors of ARE. In this model, covariates with p values ≤0.05 in the respective univariate analysis were entered.
The statistical software package SPSS for Windows version 16.0 (SPSS, Chicago, IL) was used to analyze the data.
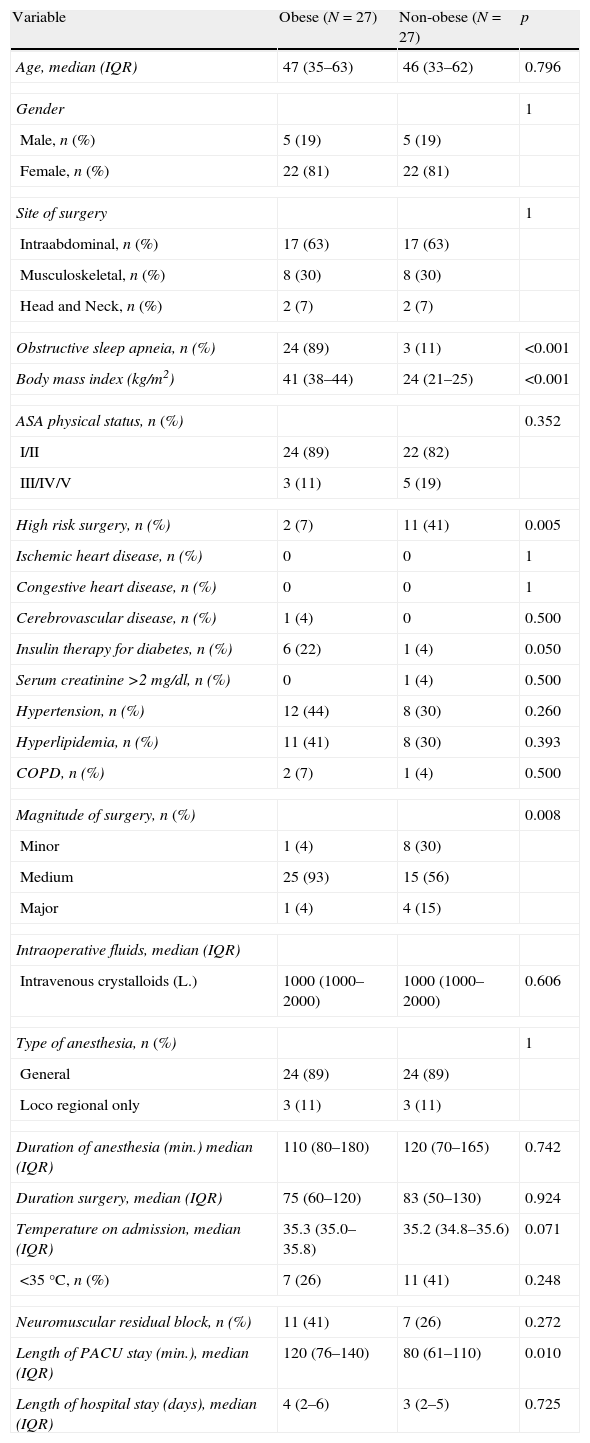
ResultsA total of 27 pairs of study subjects were admitted into the PACU during the study period. Table 1 presents the characteristics of patients admitted to the PACU and a comparison between the obese and non-obese patients.
Patient characteristics (n=54).
| Variable | Obese (N=27) | Non-obese (N=27) | p |
| Age, median (IQR) | 47 (35–63) | 46 (33–62) | 0.796 |
| Gender | 1 | ||
| Male, n (%) | 5 (19) | 5 (19) | |
| Female, n (%) | 22 (81) | 22 (81) | |
| Site of surgery | 1 | ||
| Intraabdominal, n (%) | 17 (63) | 17 (63) | |
| Musculoskeletal, n (%) | 8 (30) | 8 (30) | |
| Head and Neck, n (%) | 2 (7) | 2 (7) | |
| Obstructive sleep apneia, n (%) | 24 (89) | 3 (11) | <0.001 |
| Body mass index (kg/m2) | 41 (38–44) | 24 (21–25) | <0.001 |
| ASA physical status, n (%) | 0.352 | ||
| I/II | 24 (89) | 22 (82) | |
| III/IV/V | 3 (11) | 5 (19) | |
| High risk surgery, n (%) | 2 (7) | 11 (41) | 0.005 |
| Ischemic heart disease, n (%) | 0 | 0 | 1 |
| Congestive heart disease, n (%) | 0 | 0 | 1 |
| Cerebrovascular disease, n (%) | 1 (4) | 0 | 0.500 |
| Insulin therapy for diabetes, n (%) | 6 (22) | 1 (4) | 0.050 |
| Serum creatinine >2mg/dl, n (%) | 0 | 1 (4) | 0.500 |
| Hypertension, n (%) | 12 (44) | 8 (30) | 0.260 |
| Hyperlipidemia, n (%) | 11 (41) | 8 (30) | 0.393 |
| COPD, n (%) | 2 (7) | 1 (4) | 0.500 |
| Magnitude of surgery, n (%) | 0.008 | ||
| Minor | 1 (4) | 8 (30) | |
| Medium | 25 (93) | 15 (56) | |
| Major | 1 (4) | 4 (15) | |
| Intraoperative fluids, median (IQR) | |||
| Intravenous crystalloids (L.) | 1000 (1000–2000) | 1000 (1000–2000) | 0.606 |
| Type of anesthesia, n (%) | 1 | ||
| General | 24 (89) | 24 (89) | |
| Loco regional only | 3 (11) | 3 (11) | |
| Duration of anesthesia (min.) median (IQR) | 110 (80–180) | 120 (70–165) | 0.742 |
| Duration surgery, median (IQR) | 75 (60–120) | 83 (50–130) | 0.924 |
| Temperature on admission, median (IQR) | 35.3 (35.0–35.8) | 35.2 (34.8–35.6) | 0.071 |
| <35°C, n (%) | 7 (26) | 11 (41) | 0.248 |
| Neuromuscular residual block, n (%) | 11 (41) | 7 (26) | 0.272 |
| Length of PACU stay (min.), median (IQR) | 120 (76–140) | 80 (61–110) | 0.010 |
| Length of hospital stay (days), median (IQR) | 4 (2–6) | 3 (2–5) | 0.725 |
SD: standard deviation; IQR: interquartile range; ASA: American Society of Anesthesiologists; COPD: chronic pulmonary obstructive disease; PACU: post anesthesia care unit.
Age was similar between the groups; obese patients had a median age of 47 years and an interquartile range (IQR) value between 35 and 63 years, in comparison with non-obese patients who had a median of 46 years and IQR values between 33 and 61 years.
Obese patients had a higher BMI (median, 41 vs. 24, p<0.001), were more frequently HR-OSA patients (89% vs. 11%, p<0.001) were less frequently scheduled to high-risk surgery (7% vs. 41%, p=0.005) and major surgery (4% vs. 15%, p=0.008). Obese patients more frequently had AREs in PACU (33% vs. 7%, p<0.018).
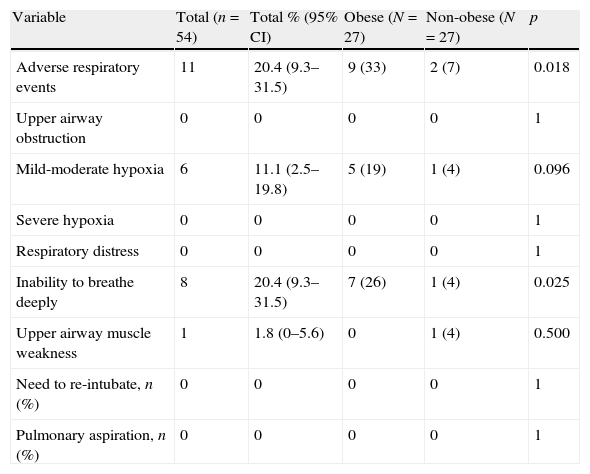
Table 2 summarizes the occurrence of postoperative respiratory complications in obese and non-obese patients. There was a greater overall incidence of postoperative respiratory complications in the obese group in comparison with the non-obese group (33% vs. 7%, p=0.018). Inability to breathe deeply was the most common complication (26% in obese patients vs. 4% in non-obese patients, p=0.025).
Adverse respiratory events (n=54).
| Variable | Total (n=54) | Total % (95% CI) | Obese (N=27) | Non-obese (N=27) | p |
| Adverse respiratory events | 11 | 20.4 (9.3–31.5) | 9 (33) | 2 (7) | 0.018 |
| Upper airway obstruction | 0 | 0 | 0 | 0 | 1 |
| Mild-moderate hypoxia | 6 | 11.1 (2.5–19.8) | 5 (19) | 1 (4) | 0.096 |
| Severe hypoxia | 0 | 0 | 0 | 0 | 1 |
| Respiratory distress | 0 | 0 | 0 | 0 | 1 |
| Inability to breathe deeply | 8 | 20.4 (9.3–31.5) | 7 (26) | 1 (4) | 0.025 |
| Upper airway muscle weakness | 1 | 1.8 (0–5.6) | 0 | 1 (4) | 0.500 |
| Need to re-intubate, n (%) | 0 | 0 | 0 | 0 | 1 |
| Pulmonary aspiration, n (%) | 0 | 0 | 0 | 0 | 1 |
The length of stay in the PACU was greater for obese patients (120min vs. 84min, p<0.01).
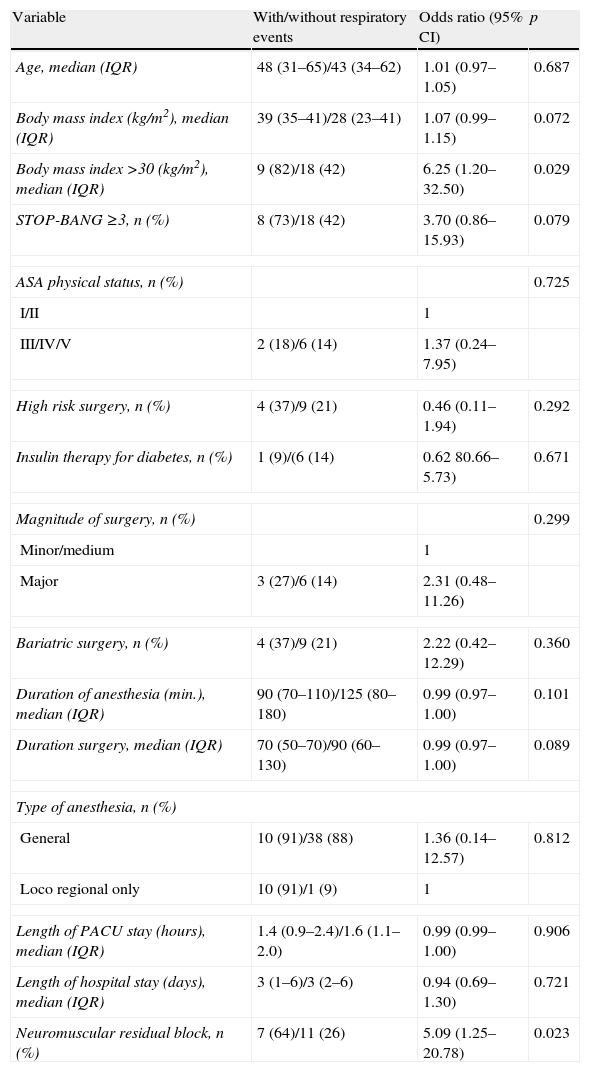
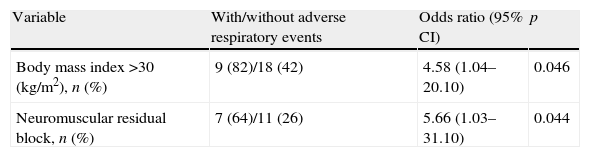
In the univariate analyses, only obesity and neuromuscular residual block after surgery were considered significant risk factors for AREs (Table 3). As shown by the multiple regression logistic analysis, these 2 variables were considered independent risk factors for the occurrence of AREs in the PACU (Table 4).
Risk factors for postoperative respiratory complications in the PACU.
| Variable | With/without respiratory events | Odds ratio (95% CI) | p |
| Age, median (IQR) | 48 (31–65)/43 (34–62) | 1.01 (0.97–1.05) | 0.687 |
| Body mass index (kg/m2), median (IQR) | 39 (35–41)/28 (23–41) | 1.07 (0.99–1.15) | 0.072 |
| Body mass index >30 (kg/m2), median (IQR) | 9 (82)/18 (42) | 6.25 (1.20–32.50) | 0.029 |
| STOP-BANG ≥3, n (%) | 8 (73)/18 (42) | 3.70 (0.86–15.93) | 0.079 |
| ASA physical status, n (%) | 0.725 | ||
| I/II | 1 | ||
| III/IV/V | 2 (18)/6 (14) | 1.37 (0.24–7.95) | |
| High risk surgery, n (%) | 4 (37)/9 (21) | 0.46 (0.11–1.94) | 0.292 |
| Insulin therapy for diabetes, n (%) | 1 (9)/(6 (14) | 0.62 80.66–5.73) | 0.671 |
| Magnitude of surgery, n (%) | 0.299 | ||
| Minor/medium | 1 | ||
| Major | 3 (27)/6 (14) | 2.31 (0.48–11.26) | |
| Bariatric surgery, n (%) | 4 (37)/9 (21) | 2.22 (0.42–12.29) | 0.360 |
| Duration of anesthesia (min.), median (IQR) | 90 (70–110)/125 (80–180) | 0.99 (0.97–1.00) | 0.101 |
| Duration surgery, median (IQR) | 70 (50–70)/90 (60–130) | 0.99 (0.97–1.00) | 0.089 |
| Type of anesthesia, n (%) | |||
| General | 10 (91)/38 (88) | 1.36 (0.14–12.57) | 0.812 |
| Loco regional only | 10 (91)/1 (9) | 1 | |
| Length of PACU stay (hours), median (IQR) | 1.4 (0.9–2.4)/1.6 (1.1–2.0) | 0.99 (0.99–1.00) | 0.906 |
| Length of hospital stay (days), median (IQR) | 3 (1–6)/3 (2–6) | 0.94 (0.69–1.30) | 0.721 |
| Neuromuscular residual block, n (%) | 7 (64)/11 (26) | 5.09 (1.25–20.78) | 0.023 |
SD: standard deviation; IQR: interquartile range; ASA: American Society of Anesthesiologists; PACU: post anesthesia care unit.
The principal findings of this study were the following. One, obese patients have a higher incidence of AREs than matched non-obese surgical patients. Second, the inability to breathe deeply and mild/moderate hypoxia were the most frequent AREs in the immediate postoperative period, and they were more frequent in obese patients (class II and III). Third, obesity and residual neuromuscular block were independent risk factors for AREs in the PACU. Even though the patients stayed longer in the PACU, the length of hospital stay had no impact on the incidence of AREs.
Obesity is known to be associated with sleep apnea, atelectasis, and hypoventilation syndrome. It is also associated with decreased vital capacity, functional residual capacity, forced expiratory volume in 1 second, and arterial oxygen tension. In our patient population, we found that obese patients had a greater incidence of adverse respiratory events.
Our study shows that obesity may be associated with AREs after surgery, and obese patients showed a nearly 4.6-fold increase in respiratory events in the PACU in comparison with non-obese patients. Previous studies have also shown a correlation between obesity and respiratory complications: in a retrospective analysis by Kuduvalli et al.16 with data from coronary artery bypass surgery patients, a BMI greater than 35 was associated with prolonged mechanical ventilation, and Merkow et al.8 found obesity to be associated with pulmonary embolus after surgery.
It is not surprising that residual neuromuscular block was an independent risk factor for respiratory events. Indeed, residual neuromuscular blockade has been commonly observed in the PACU when neuromuscular blocking drugs (NMBDs) are administered during surgery.17,18 Postoperative respiratory events are the most commonly reported adverse outcomes associated with residual paralysis in both observational and randomized clinical studies.19 Murphy et al.15 performed a case-control prospective study examining the association between residual neuromuscular blockade and critical respiratory events in the PACU and concluded that incomplete neuromuscular recovery is an important contributing factor in the development of adverse respiratory events in the PACU. Studies in volunteers have demonstrated that TOF fade ratios less than 0.70–0.90 are associated with upper airway obstruction,20 inadequate recovery of pulmonary function,20 reduced pharyngeal muscle coordination, an increased risk for aspiration,21 and an impaired hypoxic ventilatory response.22
Considering the fact that the prevalence of complications in the surgical population with OSA is higher than that in the general population and varies with different surgical populations, we relied on a concise and easy-to-use questionnaire with a high sensitivity and negative predictive value (NPV) for OSA screening in surgical patients. In fact, the sensitivities at the apnea–hypopnea index obtained from polysomnography cutoffs of greater than 5, greater than 15, and greater than 30 were, as described by Chung et al.,14,23 of 83.6%, 92.9%, and 100%, respectively and the corresponding NPVs were 60.8%, 90.2%, and 100%.
Obese patients were more frequently patients with HR-OSA and had higher BMI, as was expected by the process of matching. Obesity is associated with a 12–30-fold higher risk of OSA relative to the normal population.24 It is well known that OSA also has a significant impact on both acute and chronic cardiorespiratory function.25 Obstructive sleep apnea (OSA), the most prevalent breathing disturbance in sleep,26 has a high incidence among surgical patients and affects 2–26% of the general population, depending on sex, age, and the criteria of diagnosis.25 A growing body of literature suggests that OSA has been implicated in the development of cardiorespiratory diseases.27,28 Despite this evidence, in our study HR-OSA was not considered an independent risk for postoperative respiratory events, which agrees with the results of other studies.24
We recognize that this study has a number of important limitations. First, the results must be considered as merely associations, and causality cannot be implied. Second, our matching process was constructed in such a way that age, gender, type of surgery, and surgery date were matched. However, this process did not match for individual patient characteristics, and our results show that obese patients more frequently underwent bariatric surgery and less frequently had major surgery or high-risk surgery. Thus we can exclude the possibility that the associated risk linked to high-risk surgery, rather than the diagnosis of obesity by itself, may account for the higher complication rates. Third, we relied on the STOP-BANG questionnaire to classify patients as HR-OSA and did not carry out polysomnographic studies, which are the gold standard for diagnosing OSA. Fourth, our ARE definitions involved subjective criteria, and this may have influenced the diagnosis. The AREs were registered only during PACU stay, and complications that could have occurred after discharge were not considered, which might be viewed as a major limitation.
Despite the above limitations, this study indicates that obese patients had an increased incidence of postoperative AREs.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Mendonça J, Pereira H, Xará D, Santos A, Abelha FJ. Doentes obesos: complicações respiratórias na unidade pós-anestésica. Rev Port Pneumol 2014;20:12–19.