Pleural effusion is common in Pulmonology but primary pleural neoplastic causes are rare and sometimes difficult to diagnose.1
Case 1: A 50-year-old ex-smoker man with dyspnea, right chest pain and constitutional symptoms for 1 month was hospitalized for pleural effusion. The pleural fluid was an exudate containing predominantly mononuclear leukocytes, normal adenosine deaminase (ADA) level, without microorganisms or neoplastic cells. A thoracic–abdominal–pelvic computerized tomography (CT) demonstrated right pleural effusion with focal pleural thickening (Fig. 1A). Bronchofibroscopy did not show relevant changes and the blind pleural biopsy revealed nonspecific pleuritis. Medical pleuroscopy showed pleural lesions, of which biopsies were inconclusive. Video-assisted thoracoscopic surgical pleuropulmonary biopsy evidenced a mesenchymal neoplasm occupant of pleura and lung parenchyma, with fusocellular pattern, at the expense of cells with nuclear atypia and positive immunostaining for vimentin and smooth muscle actin, with a mitotic index less than 5 mitoses per 10 HPF (high-power field) under fasciculated pattern with heterogeneous deposition of a hyaline matrix and slit like small vascular paths, corresponding to pleuropulmonary leiomyosarcoma (Fig. 1C). Extra-thoracic lesions were not identified. The rapid clinical deterioration prevented the start of antineoplastic therapy and the patient died 11 weeks after admission.
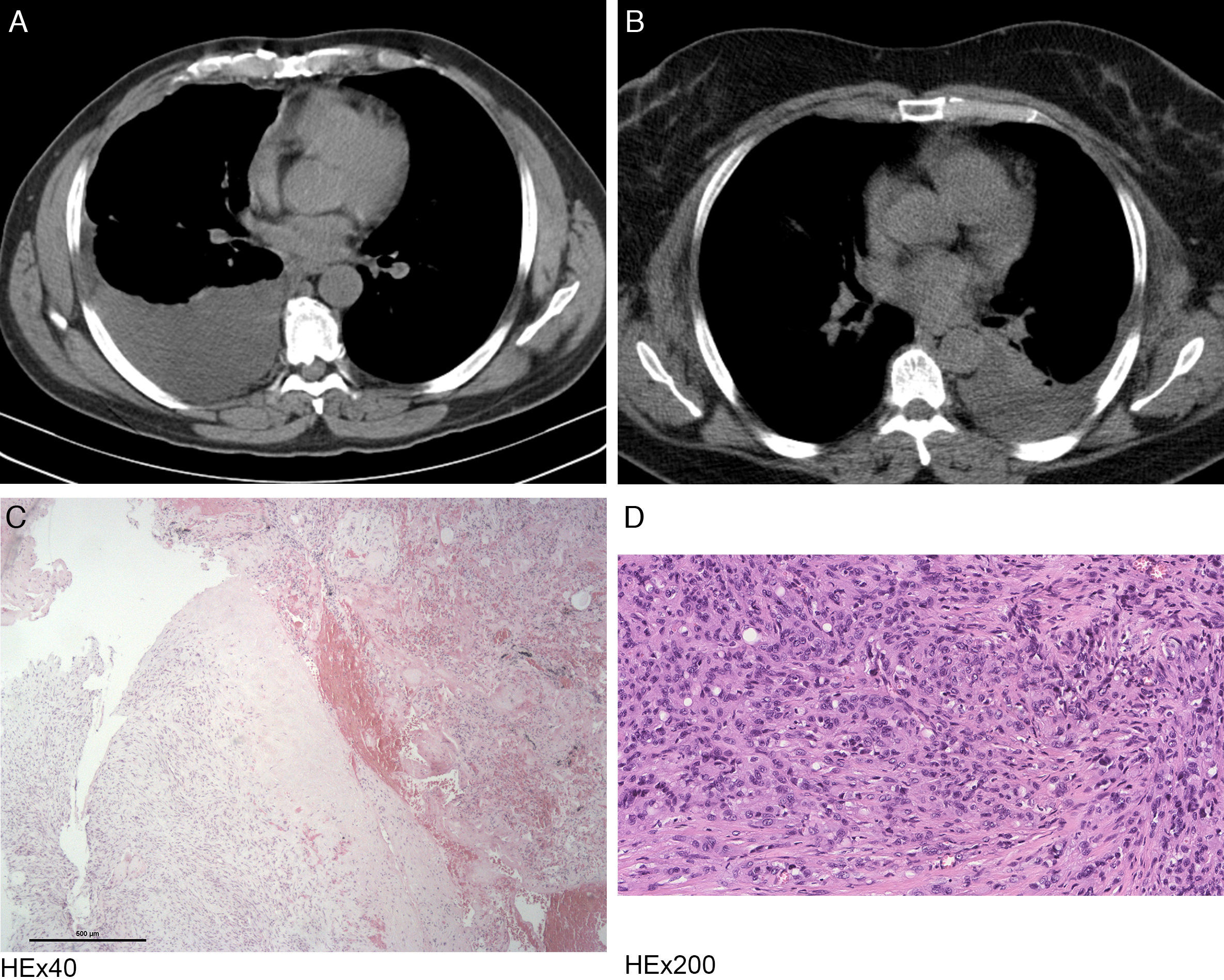
Radiological and histological features observed in the described clinical cases (Case 1: A and C, Case 2: B and D).
(A) Chest CT image demonstrating a right pleural effusion with atelectasis of the adjacent lung parenchyma and areas with pleural thickening.
(B) Chest CT image revealing a left pleural effusion with associated pulmonary atelectasis.
(C) Photomicrograph illustrating the presence of lung parenchyma with mesenchymal neoplasm in continuity, with expansive margin and heterogeneously deposition of hyaline matrix with foci of hemorrhage. Stain: hematoxylin and eosin (HE); magnification: 40×.
(D) Photomicrograph showing the presence of pleura involved by neoplasia, composed of epithelioid cells of irregular ovoid nuclei and eosinophilic cytoplasm, often with vacuoles and some erythrocytes inside. Stain: hematoxylin and eosin (HE); magnification: 200×.
Case 2: A 47-year-old non-smoker woman with recent history of chest trauma was admitted due to left chest pain and dyspnea with 3 months of evolution. The chest CT showed left pleural effusion (Fig. 1B). The hematic pleural fluid was a lymphocytic exudate with normal ADA, without criteria for hemothorax and negative cytology for malignancy. Bronchofibroscopy did not show relevant alterations and the blind pleural biopsy revealed nonspecific pleuritis. Due to symptomatic persistence and pleural thickening causing pulmonary restriction, she underwent pulmonary decortication and parietal pleurectomy. Pleural histological examination revealed epithelioid cells proliferation with atypia and positive for the CD34 marker, favoring the diagnosis of epithelioid hemangioendothelioma (Fig. 1D). The thoraco–abdominal–pelvic CT did not show other alterations. Chemotherapy was initiated with Doxorubicin but the patient died after the first cycle, 6 months after admission.
Primary thoracic sarcomas are tumors derived from mesenchymal cells, they represent 5% of all thoracic neoplasms and may involve lung, pleura and mediastinum.2 The leiomyosarcoma and epithelioid hemangioendothelioma with pleuropulmonary origin are two extremely rare types of these tumors that, due to the clinical and histological similarity to other pleural neoplasms, are often difficult to diagnose, with most of the cases diagnosed by surgical biopsy.3,4 The pleuropulmonary leiomyosarcoma usually presents as a nonspecific pleural mass and/or effusion with pulmonary involvement as a well defined nodule with smooth margins, necrotic mass or endobronchial lesions.2,3 Some risk factors have been identified, namely previous chemotherapy or radiation therapy and environmental or occupational exposure.2 It is characterized by malignant spindle cells with immunohistochemical staining for smooth muscle actin, vimentin and desmin.2,3 The treatment of choice in the limited disease is surgical resection associated with chemotherapy and/or radiation assessed on a case-by-case basis, depending on the histological grade and the clinical stage.2,3 In the advanced disease only chemotherapy is recommended.3 The median survival for patients with extensive disease is about 12 months.3 The pleural epithelioid hemangioendothelioma has vascular origin and usually is manifested by unilateral pleural effusion and nodular pleural thickening.4,5 The clinical presentation is variable, however, chest pain, dyspnea and cough are consistent symptoms.4 Although risk factors are unclear, cases have been described that follow exposure to occupational contaminants, such as roofing material, industrial exposures, cheese making, and asbestos.6 It is characterized by cords and nests of epithelioid cells similar to endothelial cells, associated with a myxohyaline matrix and immunoreactive for CD34, CD31, vimentin and factor VIII.2,4 Surgical resection is recommended but, when impracticable, chemotherapy has been used, although not uniformly.4 Compared to the pulmonary form, the pleural epithelioid hemangioendothelioma usually has an aggressive clinical course and a poor prognosis.5,7 The authors describe two patients with rare causes of pleural effusion, illustrative of the diagnostic difficulty and aggressiveness of these tumors.
Conflicts of interestThe authors have no conflicts of interest to declare.