Uterine leiomyomas are common benign neoplasms, however there are some variants characterized by histologic features which are identical to benign uterine leiomyomas but have a quasi-malignant ability to metastasize.1 Benign metastasizing leiomyoma (BML) is a rare condition characterized by leiomyomas at places distant from the uterus.2 The lungs are the most common organs for BML metastases, however extra-pulmonary lesions have also been reported.1
We present a symptomatic case of pulmonary BLM with an uncommon radiographic manifestation. We also announce the benefit of the gonadotropin releasing hormone (GnRH) agonists in the treatment of this condition.
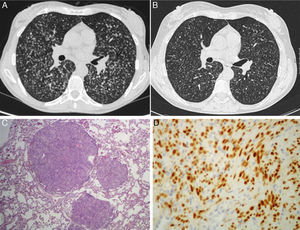
A 49-year-old white woman presented with a 2-year history of progressive dyspnea on exertion without any other symptoms. She was a current smoker (35 pack-years) and her medical history included deep venous thrombosis, hysterectomy and left-sided oophorectomy for uterine leiomyomas performed 4 years ago. She appeared to be healthy but had 80% peripheral arterial oxygen saturation, breathing room air, without other relevant alterations. Chest radiographs and computed tomography (CT) scan showed multiple diffuse bilateral small and well-defined noncalcified lung nodules (Fig. 1A). Laboratory studies did not show relevant modifications. The arterial blood gas analysis revealed hypoxemic respiratory failure (PaO2=50mmHg, breathing room air) and the pulmonary function studies presented a reduction in diffusing capacity of the lung for carbon monoxide (DLCO=58% predicted value) with preserved lung volumes and flows. Bronchoalveolar lavage had less than 5% of Langerhans’ cell (2.46%), bacterial, fungal and mycobacterial cultures were negative and pulmonary transbronchial biopsies were inconclusive. A surgical lung biopsy demonstrated pulmonary parenchyma with small nodules (1 to 3mm) composed of spindle-shaped cells without atypia, necrosis or mitotic activity (Fig. 1C). The immunohistochemistry study revealed positivity in the cells for smooth muscle actin, estrogen (Fig. 1D) and progesterone receptors and negative for HMB-45 and S-100. The diagnosis of pulmonary BML was made. She started goserelin acetate, GnRH agonist, and one year later we documented shrinkage of lung nodules (Fig. 1B) and respiratory insufficiency improvement (PaO2=65mmHg, breathing room air). Previous chest radiographs and CT scans were reviewed and 4 years earlier, simultaneous to the diagnosis of large uterus with multiple nodules, the chest CT scan had already identified multiple diffuse bilateral small noncalcified lung nodules that had not been fully investigated.
(A) Initial computed tomography (CT) scan of the thorax showed multiple diffuse bilateral small and well-defined noncalcified lung nodules. (B) CT scan of thorax one year after GnRH treatment documented shrinkage of lung nodules. (C) Low-power photomicrograph (hematoxylin-eosin stain) of a lung wedge resection by mini-thoracotomy; (D) immunohistochemistry of the lung nodule: diffusely positive for estrogen receptors, 200×.
BML was first described by Steiner in 1939 to report the presence of extra- uterine benign-appearing smooth muscle tumors.2 Although lung metastases are often asymptomatic and discovered accidentally,3 they can induce cough, dyspnea, haemoptysis and chest pain.1 Fatal events have also been reported.2 In our case, we have documented incapacity symptoms and change of the lung function with severe hypoxemic respiratory failure that are uncommon manifestations.1
The radiological findings are wide and nonspecific, mimicking other entities.3 They include well-circumscribed solitary or multiple pulmonary smooth muscle nodules, ranging in size, scattered among normal interstitium.1,3 The miliary pattern, presented in this case report, is a rare feature.4
Bearing in mind that the pathogenesis of BML is controversial, various mechanisms have been proposed. Haematogenous spreading is the most generally accepted,5 but it is unclear if the spreading is an endogenous process characteristic of the primary disease or if it is facilitated by procedures. In most of the reported cases women present a prior history of uterine surgery,3,4 however, there are some cases in which the uterine tumor is discovered whether simultaneously or after the metastasis.3,4 In this case report, we admit that lung nodules identified 4 years before were already BML, having an indolent evolution during this time.
Since there is no standardized treatment, several approaches have been described. The reported methods include vigilance, surgical resection and various hormonal manipulation – the latter bearing in mind that the primary tumor and its metastases tend to be hormone sensitive.4,6 We report the beneficial effects of reversible medical castration with GnRH analogs, which suppress the endogenous gonadotropin secretion necessary for gonadal steroids production.
In conclusion, BML should be considered in the differential diagnosis of pulmonary nodules and precise estrogen receptor/actin immunohistochemical assessment in pulmonary fusiforme celled nodules may evidence its diagnosis, particularly in women with a history of uterine leiomyomas. Although, it is a rare disease without standard treatment, hormonal therapy may be considered an option.
Conflicts of interestThe authors have no conflicts of interest to declare.