Invasive mechanical ventilation (IMV) is associated with several complications. Placement of a long-term airway (tracheostomy) is also associated with short and long-term risks for patients. Nevertheless, tracheostomies are placed to help reduce the duration of IMV, facilitate weaning and eventually undergo successful decannulation.
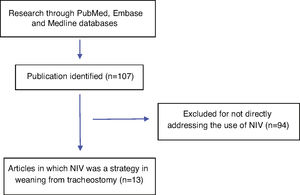
MethodsWe performed a narrative review by searching PubMed, Embase and Medline databases to identify relevant citations using the search terms (with synonyms and closely related words) “non-invasive ventilation”, “tracheostomy” and “weaning”. We identified 13 publications comprising retrospective or prospective studies in which non-invasive ventilation (NIV) was one of the strategies used during weaning from IMV and/or tracheostomy decannulation.
ResultsIn some studies, patients with tracheostomies represented a subgroup of patients on IMV. Most of the studies involved patients with underlying cardiopulmonary comorbidities and conditions, and primarily involved specialized weaning centres. Not all studies provided data on decannulation, although those which did, report high success rates for weaning and decannulation when using NIV as an adjunct to weaning patient off ventilatory support. However, a significant percentage of patients still needed home NIV after discharge.
ConclusionsThe review supports a potential role for NIV in weaning patients with a tracheostomy either off the ventilator and/or with its decannulation. Additional research is needed to develop weaning protocols and better characterize the role of NIV during weaning.
Invasive mechanical ventilation (IMV) with an endotracheal tube may lead to ventilator associated pneumonia and development of other ventilator-related complications including ventilator-induced lung injury, muscular atrophy, diaphragmatic dysfunction,1 tracheal stenosis2 and high sedation requirements. Factors associated with prolonged IMV include chronic cardiopulmonary diseases, sepsis, critical illness myoneuropathy, the use of prolonged and excessive sedation, neuromuscular blocking agents, diaphragmatic weakness, tracheo-bronchial obstruction, ineffective cough, retained secretion, nutritional and metabolic deficits.3
Tracheostomy is often placed in patients needing extended duration of endotracheal intubation. The most common indications for tracheostomy are acute respiratory failure with demonstrated or expected prolonged duration of mechanical ventilation, failure to wean from IMV, upper airway obstruction and copious secretions.4 It may diminish risks associated with prolonged endotracheal tube use such as ventilator-associated pneumonia, sinusitis and laryngeal and tracheal damage. In addition, it also improves patient comfort, reducing the need for sedation, and lowers airway resistance.4 Tracheostomy may also facilitate patient recovery as it allows more effective airway access and secretion clearance, reduces work of breathing, improves patient comfort, and promotes progression of care in and outside the intensive care unit (ICU).5
However, tracheostomy or placement of an artificial airway in the neck also has a host of short and long-term risks and complications that mirror those associated with IMV. The tracheostomy tube is a foreign body and can lead to infectious and respiratory complications, along with impaired swallowing. Moreover, patients with a tracheostomy are unable to engage in pursed-lips breathing and lose the contribution of the vocal cords in maintaining subglottic pressure.6 In most cases, the use of tracheostomy also leads to aphonia and loss of spoken communication. Early tracheostomy complications include haemorrhage, structural damage to trachea, aspiration, pneumothorax, pneumomediastinum, subcutaneous emphysema, stoma infection and stoma ulceration. Late complications include tracheal stenosis, granulation tissue formation, tracheomalacia, pneumonia, trachea-arterial fistula and tracheoesophageal fistula. Accidental decannulation and dysphagia are both early and/or late complications.4 Also, mechanical ventilation through a tracheostomy tube is associated with more demanding out-hospital management and potential respiratory incidents. In a study by Stieglitz et al. on out-of-hospital IMV patients, almost half presented with respiratory incidents, the most common being oxygen desaturation and dyspnea, requiring other interventions such as bag valve mask ventilation, need for pulmonologist consultation and replacement of the tracheostomy tube.7
As more patients with multiple co-morbidities undergo tracheostomy and develop difficulty with weaning, new innovative concepts are urgently needed for their management. Chronic ventilator dependent patients with tracheostomies are at risk of aforementioned infections and tracheal complications which further prolong duration of mechanical ventilation as well as increased mortality, so weaning from these artificial airways should start as soon as possible.8 Surprisingly, there is very little data dealing with tracheostomy patients in weaning from mechanical ventilation and subsequent tracheostomy tube decannulation. The former requires the unassisted respiratory muscles to function well enough to manage the work of breathing, the latter is feasible only if airways patency, glottic function and cough efficiency are preserved. It is not surprising that many of these patients are unable to overcome these obstacles and remain ventilator dependent. There is growing support for the use of non-invasive ventilation (NIV) to facilitate this transition off ventilatory support.
NIV has been used extensively to manage patients with acute and chronic respiratory failure,9 as well as in patients not capable of totally independent breathing after extubation.10 NIV does not usually require sedation, allowing patients to communicate, eat and drink. In a Cochrane review11 of 16 trials that compared NIV with IMV weaning, NIV significantly reduced mortality, weaning failures, ventilator associated pneumonia, ICU and hospital length of stay, total duration of IMV and rates of tracheostomy. In subgroup analysis, the authors found that the mortality benefit was greater in COPD versus non-COPD patients. The European Respiratory Society (ERS)/American Thoracic Society (ATS) guidelines suggest that in hypercapnic respiratory failure NIV may be used to facilitate weaning from IMV. It can also be used to prevent post-extubation acute respiratory failure (ARF) in high-risk patients. However, NIV is not recommended for use in the treatment of patients with established post-extubation acute respiratory failure.12
The role of NIV in mechanically ventilated patients with tracheostomy tubes to facilitate both weaning off from the ventilator and removal of the tracheostomy tube has a solid physiological rationale, but most clinical evidence is derived from limited observational studies. Therefore, to better outline the role of NIV in management in these patients with tracheostomies and chronic ventilatory failure, we conducted the following literature search and provide a narrative review on this topic.
MethodsWe searched PubMed, Embase and Medline databases for relevant citations using the search terms (with synonyms and closely related words) “non-invasive ventilation”, “tracheostomy” and “weaning” from January 1992 to February 2020. We have reviewed the bibliographies of selected studies for additional references.
We identified 13 publications comprising retrospective or prospective studies in which NIV was one of the strategies used for patients with tracheostomies during weaning from IMV and/or decannulation. These studies were analyzed in relation to number of patients with tracheostomies, clinical location and setting of NIV application, success in weaning patient with tracheostomies from IMV, success of decannulation of the tracheostomy tube and necessity for home NIV after discharge. A flowchart of the study process is reported in Fig. 1.
Due to limited and heterogeneous data, it was not feasible to perform a statistical analysis or provide high quality evidence-based recommendations, but consensus recommendations and opinions are provided where appropriate.
RationaleFactors associated with difficulties in weaning patients with tracheostomies from IMV include an imbalance between the workload and the force efficacy of the ventilatory pump, further limited by any compromise of the upper airways (for example, bulbar dysfunction, low cough efficiency, vocal cord dysfunction and airway stenosis and/or oedema).
Even brief periods of IMV may result in diaphragm weakness due to a major decline of diaphragmatic contractile force together with atrophy of diaphragm muscle fibres. IMV, sepsis and malnutrition leading to mitochondrial oxidative stress and inflammation, resulting in diaphragmatic muscle atrophy and contractile dysfunction.13 Other factors contributing to respiratory muscle dysfunction are advanced age and use of medications like corticosteroids and neuromuscular blocking agents.14 The loss of efficacy from the ventilatory pump contributes to imbalance between the work of breathing and respiratory muscle reserve.3 Therefore, the first step in weaning from tracheostomy comprises reconditioning the respiratory pump and reducing workload imposed during spontaneous breathing.8
Generally, tracheostomy tubes are placed to facilitate weaning as they do decrease dead space, are generally more comfortable for the patient and permit a gradual decrease in ventilatory support until the patient has recovered enough to maintain independent unassisted ventilation. Often this involves nocturnal ventilatory support with increasing duration of unassisted breathing during waking hours until no longer requiring assisted ventilation. However, there is a subset of patients who are not able to discontinue mechanical ventilation with this approach, in whom NIV may be able to facilitate this transition. This favourable effect is due to several physiological advantages with NIV, as it allows: reduction of inspiratory effort and work of breathing, counters intrinsic positive end-expiratory pressure, recruitment of collapsed alveoli and thereby increase dynamic compliance.15 In addition, NIV may play a decisive role in allowing decannulation, since patients can initiate NIV with the tracheostomy tube still in place and continue to receive non-invasive support during and after decannulation. As NIV applies positive airway pressure, it may help maintain upper airway patency by preventing oro-pharyngeal collapse and potentially minimizing effects of vocal cord dysfunction. However, in some patients after tracheostomy, the continuity and integrity of the trachea may be damaged, which adds extra difficulties to NIV.16
One approach is to confirm upper airway patency using bronchoscopy, after which NIV can be applied using a facial mask, with the cuff deflated and the tracheostomy capped. This will permit a check for tolerance and clinical stability, after which decannulation could be considered.17
In patients with neuromuscular respiratory weakness or failure, combined non-invasive assistance of both the ventilatory pump and forced expiratory flow is needed to wean these patients off ventilatory support. Cough augmentation techniques (CAT) may play a decisive role in secretions management and reducing weaning failure rates, especially in those patients with neuromuscular respiratory weakness and clinical conditions associated with excessive respiratory secretions. The CAT is a useful adjunct and should be applied before each period of NIV application.18
The creation and development of respiratory high-dependence care units is crucial for the management of patients with tracheostomies, especially in view of the weaning process.19 It is also important to highlight that the process of decannulation includes a multidisciplinary approach between doctors, nurses, physiotherapist and speech therapists.20
Clinical studiesUdwadia et al.2 performed a study in ICU enrolling 22 patients with difficult weaning from IMV, 9 of them had tracheostomies. Nasal NIV was used while the cuff was deflated and the tube was occluded. Patients who tolerated NIV were transferred from the ICU to a general or high dependency ward within 24−48 h (only two patients did not tolerate NIV, but not explicitly specified whether they had a tracheostomy or endotracheal tube). In this study tracheostomies were closed in all patients who were weaned from IMV (Table 1).
Characteristics of included studies reported NIV as weaning procedure from tracheostomy.
| Study | Type | Conditions | NIV (n) | NIV interface | Weaning from IMV success rate | Decannulation Success rate (in weaned patients) | Home NIV (weaned patients) | Setting | |
|---|---|---|---|---|---|---|---|---|---|
| Udwadia et al.2 | Prospective | Various | 9 | Nasal | No specific data on tracheostomy patients | ICU | |||
| Körber et al.21 | Retrospective | Various | 37 | No data | 86% | No data | 91 % | Weaning centre | |
| Schönhofer et al.22 | Retrospective | Various | 114 | No data | 84% | No data | 100% | Weaning centre | |
| Quinnell et al.23 | Retrospective | COPD | 40 | Nasal Full-face | 96% | 100% | 63% | Weaning centre | |
| Heinemann et al.24 | Retrospective | COPD | 62 a | Nasal Oronasal | No specific data on NIV | No data | 63%a | Weaning centre | |
| Ibrahim et al.25 | Retrospective | Various | 26 | Tracheos-tomy | No data | No data | 21%b | ICU | |
| Ceriana et al.26 | Retrospective | Various | 51 | Not specified | 90% | 100% | 100% | Weaning centre | |
| Sancho et al.27 | Prospective | Various | 40 | Nasal Oronasal | 100% | 100% | 100% | Respiratory care unit | |
| Bonnici et al.28 | Prospective | Various | No data | No data | No specific data on relation to NIV | Weaning centre | |||
| Bach et al.29 | Prospective | Neuromuscular | 37 | Nasal Mouth-piece | No specific data | 86% | 81% | Respiratory care unit | |
| Duan et al.30 | Prospective randomized | Various | 15 | Face-mask | 93% | 43% | No data | Respiratory intensive care unit | |
| Pu el al.16 | Retrospective | Various | 26 | Nasal Full-face | 81% | 100% | No data | Respiratory department | |
| Budweiser et al.31 | Retrospective | Various | 135 | No data | No data | No specific data on relation to NIV | Weaning centre | ||
COPD: chronic obstructive pulmonary disease; ICU: intensive care unit; NIV: non-invasive ventilation.
Körber W et al.21 reported that 32 of 37 patients with tracheostomy who had been on long-term ventilation were successfully weaned off IMV using a volume-controlled intermittent ventilation via an individually adapted face mask. Out of 37 weaned patients, 29 were discharged with home NIV.
Schöenhofer et al.22 reported their ten-year experience, in weaning centre, on 306 tracheostomy patients, 59% with COPD, using a protocol directed T-piece weaning strategy. They applied NIV in patients with ongoing hypercapnia (PaCO2 > 50 mmHg (COPD) or >45 mmHg (restrictive disease) after 24 h without ventilatory support (after capping the tracheostomy). They identified 114 hypercapnic patients, 96 of whom were maintained off IMV and discharged home on NIV; the most common condition was COPD and the rest had either thoracic cage disorders or neuromuscular disease. No data was presented on the percent undergoing successful decannulation, but it was clear that NIV was fundamental in maintaining independent ventilation to permit discharge home.
In a similar report, Quinnell et al.23 described a nine-year experience in their weaning centre, focusing on 67 COPD patients with prolonged mechanical ventilation and tracheostomy tubes. They were able to wean 65 (96%) with 62 surviving to discharge, of which NIV was initiated in patients who were unable to tolerate unsupported spontaneous breathing trials without developing respiratory distress or hypercapnia, defined as PaCO2 > 56 mmHg. NIV was used to wean 40 and used as long term ventilatory support in 25. Although not explicitly stated, all except two were discharged without tracheostomies, with NIV provided via a nasal or orofacial mask. A one-way speaking valve was also used to facilitate communication and speech. NIV was associated with a better long-term survival.
Heinemann et al.24 analysed 117 COPD patients admitted to a weaning centre. Weaning was achieved in 82 patients (although it was not discriminated how many had tracheostomies). In patients with tracheostomies, NIV was applied according to clinical and laboratory (arterial blood gas analysis) evidence of respiratory failure. NIV was initiated in 62 patients after extubation or decannulation, and 39 patients were discharged home on NIV. However, the study did not clearly state the number/percent of patients in which NIV was necessary to achieve weaning from tracheostomy after decannulation. The overall success rate in weaning from IMV was 70.1% (no distinction made between endotracheal tube and tracheostomy). The initiation of home NIV after successful weaning was an independent prognostic factor for survival to one year.
In a retrospective observational study on 26 patients with tracheostomies, Ibrahim et al.25 proposed the use of NIV as an alternative technique to facilitate discharge of patients with tracheostomies who leave the ICU and eventually leave the hospital. NIV was connected to the tracheostomy tube, and 20 patients were discharged from the ICU and 16 from the hospital (no data on decannulation or need for home NIV).
Ceriana et al.26 reviewed their experience with patients requiring prolonged mechanical ventilation and tracheostomies. Over a 13-year period, they retrospectively analysed prospectively collected data on their cohort of patients. Out a total of 587 patients, they were able to enrol 51 (9%) into their NIV decannulation protocol, of which 46 (8%) were successfully weaned and discharged on home NIV. They identified patients as candidates for NIV weaning as those who could maintain unassisted breathing and had favourable criteria for decannulation, but with signs of inadequate ventilation defined as a PaCO2 > 50 mmHg, and/or an increase in PaCO2 ≥ 5 mmHg since suspension of IMV, and/or pH < 7.33 within seven days of spontaneous breathing. These patients underwent a protocol which included downsizing by 1 mm the cannula internal diameter without fenestration, capping of the tracheostomy cannula, and increasing periods of nocturnal NIV with the goal of achieving at least 4 consecutive hours of NIV (after two nights with good adherence they were switched to a domiciliary bilevel ventilator). After conducting an upper endoscopy to check the airways, the investigators decannulated patients who were admitted to a domiciliary NIV program. The mean time needed to protocol completion was 7.2 days. Home ventilators were set with a mean IPAP of 17.1 cmH2O and mean EPAP of 4.2 cmH2O. None of the patients required surgical closure of their tracheal stoma. Five patients failed due to claustrophobia associated with the mask and/or poor adherence to the mask. After one year, the survival rate was 82% and only one of the surviving patients was switched back to IMV. It was possible to decannulate all patients in whom NIV was successfully used for weaning from IMV.
In a one-year, prospective, multicentre study of respiratory care units in Spain, Sancho et al.27 identified 231 patients with tracheostomies out of a population of 4609, requiring prolonged mechanical ventilation. Of these 231 patients, 198 (86%) were successfully weaned and of that group, 40 (21%) needed NIV during weaning, which was applied when patients were not able to progress beyond 18 h on their spontaneous breathing trial for 5 consecutive days. The ventilator was set in pressure-support mode to achieve a tidal volume of approximately 8−10 mL/Kg. In this study, the tracheostomy stoma was either capped with a tracheal button or the tracheostomy tube was capped, with the cuff deflated and inner cannula replaced with a fenestrated tube. Bronchoscopy was performed to evaluate upper and lower airways for possible lesions. No differences were found between those with a capped tracheostomy tube or tracheal button. Treatment focused on nocturnal support and ventilatory goals included a PaCO2 < 45 mmHg and less than 5% of time with oxygen saturation under 90%. In subgroup analysis, they found obstructive sleep apnea, congestive heart failure and chronic renal failure as underlying conditions of patients requiring NIV. Prior use of home CPAP, NIV or chronic hypercapnia identified those most likely to need NIV during weaning. Baseline hypercapnia was also significantly increased with an average PaCO2 of 50 ± 10 mmHg. Although not explicitly reported, it appears that all the 40 NIV patients were successfully decannulated.
Bonnici DM et al.28 conducted a prospective study of patients with tracheostomies and neuromuscular and/or chest wall disorders, postsurgical, COPD and obesity-related respiratory failure. They found that 382% of the patients were weaned to self-ventilation. In this cohort, 24% of patients were discharged with nocturnal NIV and 1.9% of patients were discharged with both nocturnal and intermittently daytime NIV. However, numbers for patients on NIV and the decannulation success rate were not explicitly reported.
Bach et al.29 conducted a prospective study on 49 patients, including 37 with tracheostomies, with primarily neuromuscular insufficiency. When patients were clinically stable, the tracheostomy tube was switched to a fenestrated cuffed one, which was then capped, and the patients were started on NIV using mouthpiece and nasal mask while awake (during sleep they would use a nasal interface or lipseal). Mechanical insufflation-exsufflation was applied when needed. After decannulation (n = 32), 26 patients required home NIV (later, it was possible to stop NIV in 9). Decannulation was successful in 32 of the 37 patients.
Duan et al.30 performed a single center feasibility study to compare the NIV vs. a conventional strategy to accelerate weaning of patients with tracheostomies. This study enrolled 15 patients in the NIV group and 17 cases in control group. At the initial stages, all of the patients underwent conventional weaning strategies. If multiple spontaneous breathing tests failed, the patient was enrolled in this study. In the NIV group, the tracheostomy cuff was deflated, and the tube was capped. NIV was initially set to an IPAP 10 cmH2O and EPAP 4 cmH2O (titration to 8 mL/kg tidal volume), with facemask. During the application of NIV, airway management was especially important especially in patients with weak cough. If the sputum production decreased and was thin, and the ability to cough was strong, the tracheostomy tube was capped for more than 48 h. If the patient tolerated this trial, the tracheostomy tube could be removed. NIV allowed weaning from IMV in 14 patients. In this study, NIV reduced nosocomial pneumonia, shortened the days on ventilator weaning and ICU length of stay for these patients with tracheostomies. From the 14 patients weaned from IMV using NIV, decannulation was possible in 6.
In a retrospective study by Pu et al.16 conventional weaning approach in those with a tracheostomy (n = 24) was compared to a sequential invasive-noninvasive ventilation strategy (n = 26). The latter patients were started on NIV with a nasal of full-face mask, while tracheostomy was plugged and the cuff deflated. Weaning was possible in 21 patients from the sequential group (however it was not disclosed whether continued nocturnal NIV was required). PaO2 at 1 and 24 h after withdrawal of IMV was significantly higher in the sequential group. Also, the sequential group presented significantly shorter duration of IMV and incidence of ventilator-associated pneumonia, and a significantly higher rate of successful weaning. Although the decannulation success rate was not explicitly reported, it appears that all the 21 patients weaned from IMV in the NIV group were decannulated.
A retrospective study by Budweiser et al.31 evaluated the usefulness of a tracheostomy retainer during decannulation. From 384 prolonged weaning patients, a tracheostomy retainer was inserted in 166. After decannulation, NIV was applied to 135 of them, with a first decannulation success rate of nearly 72% (119 of 166), and 63 patients adapted to home NIV.
DiscussionDue to advances in medical care, there is an increasing number of patients surviving admissions to the ICU who require long-term care due to prolonged IMV with tracheostomy tube in place. This is associated with increasing healthcare costs and organizational challenges for health systems related to these patients’ debilitated state and poor long-term outcomes of these patients.3 Few studies have evaluated the role of NIV in weaning and decannulating patients with a tracheostomy.
Based on the analysed results from studies using NIV to facilitate weaning from IMV, several key points are evident: 1) the majority of the studies were retrospective analyses; 2) most occurred in weaning centres; 3) NIV appears to be effective even with a tracheostomy tube in place; 4) NIV may be a useful adjunct for the very difficult to wean patient requiring prolonged mechanical ventilation and a tracheostomy, resulting in successful weaning and discontinuation from mechanical ventilation in more than 80%, and with an equally high percentage tolerating decannulation); 5) hypercapnia during or after a spontaneous breathing trial may identify patients who may benefit the most from this modality); 6) In some patients, NIV will need to be continued, typically as nocturnal support in as many as 60% or more of those weaned.
The studies16,30 comparing conventional weaning with NIV suggest that NIV can provide enough support to result in higher weaning and decannulation success rates. There may be reduction in infection as well as the length of the weaning period.
However, there are considerable limitations and lack of ability to generalize results. First of all, in some studies, the distinction between patients with tracheostomies or those with endotracheal tube is unclear. The process of decannulation is not mentioned in a significant number of the studies, and decannulation success is not uniformly reported.
There is considerable heterogeneity in the patients treated and the methods by which NIV is applied. The best NIV modality and settings during weaning require additional physiological studies. Variables of interest included the volume of dead space, upper airways resistance and resistance of the tracheostomy tube.32 It is probably safe to assume that the level of NIV inspiratory and expiratory pressure needed during the weaning process is probably greater than that applied via tracheostomy during assisted ventilation. However, this may not be borne out as most of the studies did not report on exact ventilator settings during NIV.
Of course, the underlying cause of acute respiratory failure needs to be considered when planning the weaning process with NIV.33 An underlying obstructive or restrictive disease such as COPD or a neuromuscular respiratory failure require completely different NIV settings. Not surprisingly, based on our review the patients who may benefit the most from NIV during weaning have the same conditions which are best treated with NIV during acute respiratory failure, specifically COPD, neuromuscular respiratory failure disease and obesity/hypoventilation syndrome or obstructive sleep apnea.
The choice of the optimal NIV interface is another critical point.34 Nasal mask or mouthpiece intermittent positive pressure could facilitate expectoration and air staking manoeuvre during daytime hours as opposed to an oronasal mask which could be preferable during night-time NIV to avoid excessive leaks with open mouths.
It should also be noticed that tracheal manometry was not used in any of the reported studies. This could provide objective measurements of airway pressure during capping17 and may be a useful tool to include in future studies.
On the other hand, some studies and proposed decannulation protocols35,36,37 are not directly linked to NIV use but may be the foundation for future research. Studies directed to airway secretion quantification8 and secretion clearance are important as they may contribute to weaning failure, NIV effectiveness and safety.
High-flow tracheal oxygen (HFT) has been considered as an alternative to NIV or as an integrative tool and adjunct. However, although HFT allows a more accurate FiO2,38 bypassing upper airways with administration through a tracheostomy tube forfeits some potential benefits associated with high-flow nasal cannula.38,39 The flow should be at least 50 L/min for greatest benefit.38,40 High-flow oxygen has been successfully used in liberating intubated patients from IMV when compared to both conventional oxygen and NIV. However, evidence of the role of HFT alone or combined with NIV to facilitate weaning from those with tracheostomy tubes and decannulation is still lacking.
ConclusionsThere are increasing number of reports that incorporate NIV into the weaning of patients with a tracheostomy. Most call for NIV delivered through the facial interface while the tracheostomy tube is capped. This seems to facilitate the transition off ventilatory support and eventual decannulation. Additional research is needed to develop weaning protocols and compare NIV weaning to other weaning approaches and strategies in this population.
Authors contributionThe study has more than 6 authors, since it was initiated and revised by an international panel. Miguel Guia, Raffaele Scala and Antonio Esquinas conceived and designed this study. All authors have participated in data acquistion and/or analysis, and also in manuscript revision.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone.
Guy W. Soo Hoo, who revised English; Yasmin M.
Madney, Hadeer S. Harb and Haitham Saeed (members of International Association of Non Invasive Ventilation) for their contribution.