Anaemia is increasingly recognised as an important comorbidity in the context of chronic obstructive pulmonary disease (COPD), but remains undervalued in clinical practice. This review aims to characterise the impact of anaemia and iron deficiency in COPD.
MethodsLiterature review of studies exploring the relationship between anaemia/iron deficiency and COPD, based on targeted MEDLINE and Google Scholar queries.
ResultsThe reported prevalence of anaemia in COPD patients, ranging from 4.9% to 38.0%, has been highly variable, due to different characteristics of study populations and lack of a consensus on the definition of anaemia. Inflammatory processes seem to play an important role in the development of anaemia, but other causes (including nutritional deficiencies) should not be excluded from consideration. Anaemia in COPD has been associated with increased morbidity, mortality, and overall reduced quality of life. The impact of iron deficiency, irrespective of anaemia, is not as well studied, but it might have important implications, since it impacts production of red blood cells and respiratory enzymes. Treatment of anaemia/iron deficiency in COPD remains poorly studied, but it appears reasonable to assume that COPD patients should at least receive the same type of treatment as other patients.
ConclusionsAnaemia and iron deficiency continue to be undervalued in most COPD clinical settings, despite affecting up to one-third of patients and having negative impact on prognosis. Special efforts should be made to improve clinical management of anaemia and iron deficiency in COPD patients as a means of achieving better patient care.
Chronic obstructive pulmonary disease (COPD) is a highly debilitating and life-threatening condition characterised by an airflow limitation that is not fully reversible, is generally progressive, and associated with enhanced inflammatory response in the lungs and airways.1 COPD is associated with a variety of comorbidities that aggravate the overall prognosis, including cardiovascular, metabolic, pulmonary, and hematologic disease, as well as gastrointestinal and psychiatric disorders.2,3
The exact prevalence of COPD in most regions of the world is not known. Global prevalence has been estimated at 10.1% (11.8% for men and 8.5% for women),4 but prevalence reports vary widely according to region and population under study.1,5 In Portugal, specifically in the Lisbon area, Bárbara et al.6 have previously identified a prevalence of 14.7%. COPD is generally more prevalent among smokers, men, and older individuals.1 In many countries, the disease remains, however, vastly under-recognised and underdiagnosed since patients do not present until later stages of the disease, which is then reflected in prevalence and mortality estimates.1 In this context, COPD is still the third leading cause of death in Europe and is estimated to become the third leading cause of death worldwide by 2020.1 The increasing impact of COPD is mainly explained by past rates of smoking and the ageing population. The disease is expected to have major implications for quality of life and mortality, and will represent a considerable socio-economic burden over the next decades.1
A variety of systemic manifestations of COPD have been identified over the years. Recently, these have begun to be more closely studied to establish if there are significant underlying comorbid interactions impacting on the overall prognosis of COPD patients. Several comorbidities were found to impact on COPD prognosis, including heart failure, ischaemic heart disease, metabolic syndrome, pulmonary hypertension, anxiety and depression disorders, lung cancer, pulmonary fibrosis, osteoporosis, anaemia, gastroesophageal reflux disease and peptic ulcer disease, chronic kidney disease, malnutrition, and sleep disorders.2,3,7,8
Anaemia is increasingly recognised as an important comorbidity in the context of COPD, affecting a relevant number of patients and with established negative impact on overall prognosis. There are several disease mechanisms which could potentially explain the increased occurrence of anaemia in COPD patients, including iron deficiency and inflammatory processes. Nonetheless, evidence about the role of anaemia, iron deficiency, and iron deficiency anaemia in the COPD patient remains limited and, consequently, these conditions continue to be undervalued in most COPD clinical settings.
This review aims to provide a clinical overview of the impact of anaemia and iron deficiency in COPD, including the proposed mechanisms of disease, clinical consequences, and potential effects of different treatment strategies.
MethodsIn order to characterise the impact of anaemia and iron deficiency among COPD patients, we ran query on two electronic databases: MEDLINE via PubMed and Google Scholar. MEDLINE was selected because it is one of the most important aggregators of medical research reports worldwide. In addition, Google Scholar was also used to ensure that relevant research reports published in non-indexed journals were taken into consideration.
Both these databases were queried for clinical research reports published up till June 2016. The following search terms were used: “Anaemia”, “Anemia”, “COPD”, “Chronic obstructive pulmonary disease”; “Chronic bronchitis”; “Emphysema”; “Iron deficiency”; “Iron deficiency anaemia”; “Iron deficiency anemia”. Search results were initially scanned based on title and abstract and, in cases where this initial assessment was not sufficient, article full-texts were also reviewed.
The search results yielded several systematic reviews on specific aspects of the relationship between COPD and anaemia, but these reviews also had substantial limitations due to the underlying variability of study design and population. In this review we do not present systematic data, such as a summary table with all study results, because this information is already available elsewhere in reasonable updated publications. Instead, in this clinical overview, we aim to provide a more straightforward review of the evidence on the impact of anaemia in the COPD patient, highlighting the implications for clinical practice. In addition, we also explore in greater detail the impact of iron deficiency alone or in the form of iron deficiency anaemia in the COPD patient.
ResultsPrevalence of anaemia in COPDThe reported prevalence of anaemia in COPD patients has been highly variable, mostly due to the different characteristics of study populations and the lack of a consensus definition of anaemia in the context of COPD, which led to remarkably different estimates between studies.
In a 2011 systematic review, Yohannes et al.9 identified 7 individual studies reporting the prevalence of anaemia in COPD populations and found an overall prevalence of anaemia ranging from 7.5% to 32.7%. Most studies consisted of retrospective assessments of medical records, with no standardised anaemia definition and evaluating notably different—and virtually incomparable—COPD populations, which explains this variability in prevalence estimates.
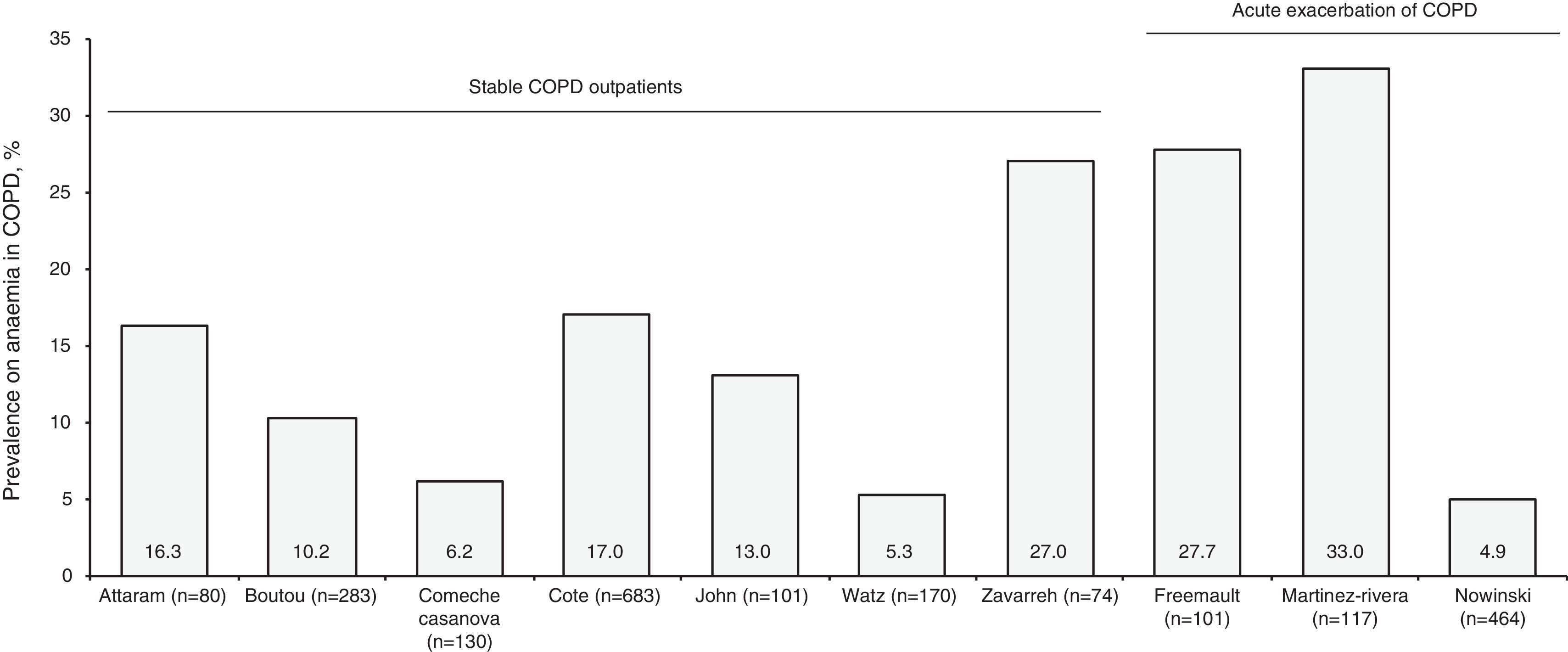
Two further updated reviews, conducted in 2015, identified 24 studies reporting on the prevalence of anaemia in COPD.10,11 These reviews encountered, nonetheless, the same issues highlighted in the initial systematic review, and further extended the range of prevalence from 4.9% to 38.0%.10,11 Variations in the prevalence of anaemia between different studies were attributed to both the intrinsic characteristics of each study population and the different definitions of anaemia—and even COPD diagnosis—applied throughout the studies.10 The definitions of anaemia varied substantially across different studies; while most authors used the World Health Organisation (WHO) definition, some used the same haemoglobin level for both men and women (since most women were post-menopausal) and others used haematocrit levels to establish anaemia. Additionally, there were also significant discrepancies in COPD diagnosis itself, with some studies not employing proper spirometric evaluation. All these issues critically impair comparisons of prevalence between different studies and populations. In an attempt at standardisation, Fig. 1 provides a comparison of reported prevalences in different settings, exclusively for prospective or cross-sectional studies, using spirometric evaluation to establish COPD and anaemia according to haemoglobin levels (including those with minor adjustments to WHO cut-offs). Further complete comparisons of all prevalence estimates are available elsewhere.10,11
Prevalence of anaemia in COPD patients reported by different prospective/cross-sectional studies defining anaemia based on haemoglobin levels (WHO definition, including minor adjustments) and establishing COPD using spirometric evaluation. COPD=chronic obstructive pulmonary disease. References: Attaram et al.85; Boutou et al.14; Comeche Casanova et al.16; Cote et al.13; John et al.12; Watz et al.17; Zavarreh et al.18; Freemault et al.20; Martinez-Rivera et al.23; Nowinski et al.24.
Overall, studies evaluated 4 broad groups of COPD patients: (1) stable COPD outpatients, (2) inpatients with acute exacerbation of COPD, (3) COPD patients from the general population, (4) and COPD patients under long-term oxygen treatment or non-invasive ventilation. Prevalence estimates for these specific subgroups are discussed in the following sections.
Stable COPD outpatientsThe reported prevalence of anaemia in stable COPD outpatients has varied from 5.3% to 17.0% in western populations12–17 (a higher prevalence (27.0%) was observed by Zavarreh et al.18 in Iran). John et al.12 conducted one of the pioneer studies in the field, and identified a prevalence of 13.0% in stable severe patients in Germany. Comparable prevalence estimates were then reported for COPD populations in the US,13 Greece,14 and the UK.15 Nonetheless, two additional studies also reported lower prevalence in a Spanish cohort (6.2%) and a different group of German patients (5.3%).16,17
Acute exacerbations of COPDIn patients with acute exacerbations of COPD the prevalence of anaemia appears to be higher, although there is also some variability in this context. Several studies showed prevalence of anaemia ranging from 18.0% to 27.7% in patients hospitalised for acute exacerbations of COPD19–22; one study found an even higher prevalence in this population, reaching 33.0%.23 Contrary to this trend of increased prevalence, two studies reported substantially lower prevalence; one study reported a prevalence of 4.9% in patients hospitalised for acute exacerbation of COPD in Poland24; other study with significantly different methodology (based solely on diagnosis codes present in a Spanish healthcare database) reported a prevalence of 9.8%.25
COPD patients from the general populationTwo large-scale, retrospective analyses of COPD inpatients and outpatients in the US estimated a prevalence of anaemia of 21.0% and 33.0%, respectively.26,27 However, these estimates were based on diagnoses introduced in healthcare databases and are subject to substantial limitations. Other studies based on COPD samples from large population-based surveys showed a much lower prevalence of anaemia, 7.3% and 7.5%, respectively.28,29 These findings could be due to the inclusion of less severe COPD cases in these population surveys, compared to inpatient and even outpatient settings.
COPD patients under long-term oxygen treatment or non-invasive ventilationThe prevalence of anaemia in patients receiving long-term oxygen treatment or non-invasive ventilation followed a pattern mostly similar to the outpatient population. Two studies in patients under long-term oxygen treatment showed prevalence ranging from 8.6% (in women only) to 11.3%.30,31 Other studies assessed anaemia in patients referred for treatment—but not necessarily treated long-term—and found higher prevalence of anaemia, ranging from 14.9% to 38.0%,32–34 which could be explained by increased disease severity and worse health status prior to treatment; additionally, treatment of acute exacerbations (oxygen treatment or non-invasive ventilation) may also explain the increased prevalence of anaemia in this specific subgroup.
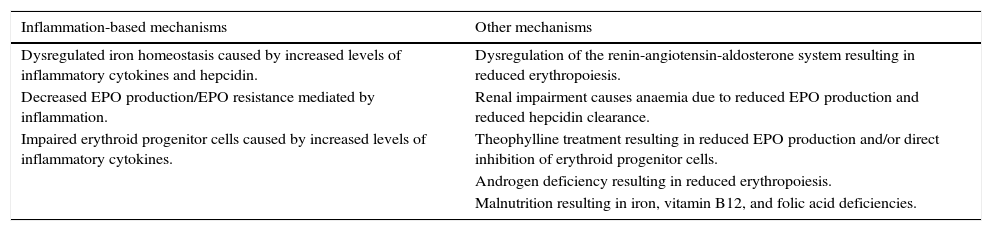
Mechanisms leading to anaemiaThe mechanisms leading to anaemia in COPD are complex, some are inter-related, and they have not yet been fully characterised. The chronic inflammatory state in COPD is thought to play the main role, since either directly or indirectly, inflammation is clearly associated with the development of anaemia of chronic disease (also referred as anaemia of inflammation). However, other factors besides inflammation have been described and could have significant impact in the development of anaemia, either alone or in association with inflammation-based mechanisms. Table 1 summarises the various proposed mechanisms leading to anaemia in the context of COPD.
Proposed mechanisms of anaemia in the context of COPD.
| Inflammation-based mechanisms | Other mechanisms |
|---|---|
| Dysregulated iron homeostasis caused by increased levels of inflammatory cytokines and hepcidin. | Dysregulation of the renin-angiotensin-aldosterone system resulting in reduced erythropoiesis. |
| Decreased EPO production/EPO resistance mediated by inflammation. | Renal impairment causes anaemia due to reduced EPO production and reduced hepcidin clearance. |
| Impaired erythroid progenitor cells caused by increased levels of inflammatory cytokines. | Theophylline treatment resulting in reduced EPO production and/or direct inhibition of erythroid progenitor cells. |
| Androgen deficiency resulting in reduced erythropoiesis. | |
| Malnutrition resulting in iron, vitamin B12, and folic acid deficiencies. |
COPD, chronic obstructive pulmonary disease; EPO, erythropoietin.
Disruption of normal iron homeostasis is a hallmark of anaemia of chronic disease, in which several factors contribute to reduce iron availability in the plasma and, consequently, impair erythropoiesis. In the context of a chronic inflammatory state (as seen in COPD) several processes can contribute to dysregulated iron homeostasis.35 Inflammatory cytokines such as interleukin (IL)-1, IL-6, IL-10, interferon-γ (INF-γ), and tumour necrosis factor 1-α (TNF-α) interfere with the normal function of several molecules involved in iron absorption, storage, and transport, including ferritin, transferrin, ferroportin, and divalent metal transporter 1 (DMT1).11,36–38 The effects exerted by these inflammatory cytokines—whose levels are generally increased in anaemic COPD patients11,36—on these molecules involved in iron metabolism lead to a reduction in serum iron levels and decreased iron availability for erythropoiesis. In addition to these direct effects on iron metabolism, inflammatory cytokines (particularly IL-6) have been found to strongly influence hepcidin production. Hepcidin is the most important regulator of extracellular iron homeostasis, exerting an inhibitory effect on the release of iron to the extracellular fluid (to avoid iron overload).39 In a context of normal iron homeostasis, hepcidin production is reduced in response to hypoxia and anaemia, so that erythropoietic iron demands can be fulfilled. However, in chronic inflammatory states, IL-6 induces synthesis and secretion of hepcidin by hepatocytes and, consequently, reduces extracellular iron availability.40–42
Erythropoietin (EPO) acts as the primary stimulus for erythropoiesis, being mostly produced by the kidneys in response to decreased tissue oxygenation.43 In COPD patients, two different changes in normal EPO functioning have been described. Non-clinical and clinical evidence suggests that EPO production could be inhibited by the effects of inflammatory cytokines.44–46 However, some clinical studies have also identified increased levels of EPO in COPD patients18,47–49 (consistent with normal response to tissue hypoxia). In any case, even increased EPO levels in COPD are not necessarily translated to enhanced erythropoiesis, which has been explained by EPO resistance in this population due to systemic inflammation.48,50
Inflammatory cytokines have also been found to directly impair the function of erythroid progenitor cells in various ways. INF-γ and TNF-α inhibit erythroid colony formation51 and IL-1 has direct inhibitory effects on erythropoiesis both in vitro and in vivo (mice).52 Additionally, direct action of inflammatory cytokines on erythroid progenitor cells favours the formation of free radicals,53 which hinders cell function and potentially leads to proliferation arrest or apoptosis.
These different mechanisms of anaemia based on chronic systemic inflammation are seen in a variety of conditions; in most cases the role of these mechanisms is non-exclusive, with inflammatory mediators influencing normal red blood cell homeostasis at different levels and, thus, impairing normal correction mechanisms. In any case, given the overall health status of COPD patients, it is also likely that other factors interplay with inflammation in the development of anaemia.
Other non-inflammation-based mechanismsThe renin-angiotensin-aldosterone system (RAAS) has been implicated in the regulation of erythropoiesis in COPD patients. Angiotensin II stimulates erythroid progenitor cells and promotes EPO production54; angiotensin-converting enzyme also shows increasing activity in contexts of hypoxia.55 Two clinical studies assessed the potential impact of RAAS in erythropoiesis in COPD patients. Significantly increased levels of renin and aldosterone were found in COPD patients with erythrocytosis vs. controls with similar EPO levels between groups, which indicates that RAAS could be involved in normal compensatory mechanisms.56 A decrease in haematocrit was also found in COPD patients under irbersartan (an angiotensin II receptor antagonist) for 4 months in a randomised trial.57 These data indicate that normal functioning of the RAAS could have a relevant role in the correction of hypoxia through erythropoiesis and, therefore, dysregulation of the RAAS in COPD patients (either through anti-hypertensive agents or other factors) might explain the development of anaemia.
Renal impairment, which is highly prevalent in COPD,58 can lead to anaemia by two different—and complementary—mechanisms. EPO is produced in the kidney and impaired renal flow leads to disruption in EPO production in response to hypoxia.59,60 Additionally, reduced renal clearance of hepcidin seen in patients with renal impairment leads to increased serum hepcidin levels, which limits iron availability for erythropoiesis.61
Theophylline treatment was associated with decreased haematocrit in COPD patients, as compared to untreated controls with similar oxygen saturation.62 The effects of theophylline on erythropoiesis are not fully characterised; an adenosine-mediated reduction in renal EPO production has been described,63 as well as a more direct inhibition of erythroid progenitor cells.64
Androgen deficiency, specifically testosterone deficiency, is a common finding in COPD (reaching a prevalence of up to 69%).65 Since testosterone is known to stimulate erythropoiesis, testosterone deficiencies could potentially explain the development of anaemia. In a general population study, such an association between testosterone and haematocrit has already been demonstrated66; specific studies on COPD patients are yet to be conducted.
Malnutrition or minor forms of deficient nutritional intake are common causes of anaemia in otherwise healthy individuals.67 Although it is generally assumed to be less common in contexts of chronic inflammatory disease such as COPD, nutritional deficiency should still be considered a potential important cause of anaemia. Some studies have reported deficient intake of various nutrients in COPD patients, including iron, vitamin B12, and folic acid,68–70 but the impact of nutritional intake in COPD patients remains poorly characterised and should be further investigated.
Lastly, oxygen supplementation has been hypothesised as potentially leading to reduced EPO production and impaired erythropoiesis. However, the effects are still poorly investigated, vary among studies, and are even counterintuitive for some studies.30,71
Consequences of anaemia in COPDAnaemia in COPD has been associated with increased morbidity, mortality, and overall reduced quality of life. Several clinical studies reported a significant deleterious effect of anaemia on exercise capacity, with anaemic patients presenting worse dyspnoea and shorter six-minute walk distance (6MWD). Initially, Cote et al.13 found anaemic patients to have significantly higher modified Medical Research Council (MRC) dyspnoea scale scores and lower 6MWD in a cohort of 683 stable COPD outpatients, with anaemia being a significant predictor of dyspnoea and exercise capacity. Boutou et al.14 reported comparable results in terms of dyspnoea and exercise capacity in a cohort of 283 stable COPD patients, although in this study exercise capacity was established based on respiratory parameters rather than 6MWD. Corlateanu et al.72 reached similar findings, identifying haemoglobin levels to be a significant predictor of dyspnoea and exercise capacity in a cohort of 80 elderly COPD patients, which explained 21% of the variation in MRC and 17% in exercise capacity. Ferrari et al.73 also reported significantly higher MRC scores and lower 6MWD in anaemic patients from a cohort of 105 COPD outpatients; here the authors also found significantly lower maximal oxygen consumption (VO2max). Interestingly, some studies also identified an association between the presence of anaemia and COPD severity,14,16,17 however, given their methodology, these studies cannot establish causality—anaemia could either be a result of worse overall health status in severe COPD or actually be a cause of increased COPD severity.
Health-related quality of life (HRQoL) was found to be significantly worse in COPD anaemic patients in two different studies. A post hoc analysis of a population-based study, which included 495 COPD patients, compared HRQoL between anaemic and non-anaemic COPD patients based on Short Form-36 (SF-36) scores.29 Unadjusted analysis showed that anaemic COPD patients had significantly lower physical functioning and physical component summary scores; however, both these scores were not significantly related to anaemia after adjustment for covariates.29 This study had limitations related to its design (post hoc analysis) and reduced sample size of anaemic COPD patients, which prevent definite conclusions on HRQoL. The previously mentioned study by Ferrari et al.73 revisited this issue by assessing HRQoL using the St. George's Respiratory Questionnaire (SGRQ), which was deemed more appropriate for a COPD population. Anaemic COPD patients showed significantly worse HRQoL compared to non-anaemic counterparts for all SGRQ components (i.e. symptoms, activity, or impact scores) as well as the total score. In regression analysis, after adjustment for covariates, higher haemoglobin levels were significantly associated with better HRQoL.73 Further prospective, large-scale studies would be of interest to better establish the impact of anaemia in the HRQoL of COPD patients.
Some studies that reported on comorbid anaemia in COPD also provided mortality estimates, showing an overall trend for increased mortality in anaemic COPD patients.9 However, these were mostly severely limited studies (in many cases retrospective analysis of healthcare databases) which were not specially designed to assess survival/mortality. Chambellan et al.31 conducted an analysis of 2524 COPD patients from the ANTADIR observatory to evaluate the relationship between haematocrit and survival in COPD. In this population, after multivariate analysis, haematocrit was found to be an independent predictor of survival, with a 3-year survival of 24% when the haematocrit was <35% (compatible with anaemia) versus 70% when the haematocrit was >55%.31 Rasmussen et al.22 examined the association between anaemia and 90-day mortality in a retrospective analysis of 222 COPD patients initiating invasive mechanical ventilation due to acute respiratory failure. After covariate adjustment, mortality was significantly higher in anaemic patients for both 30-days and 90-days timeframes.22 Martinez-Rivera et al.23 investigated the effects of anaemia on mortality in 117 patients hospitalised for acute exacerbation of COPD. After one year of follow-up, haemoglobin and haematocrit levels were significantly higher in patients who survived; multivariate analysis revealed anaemia and previous exacerbations as significant predictors of mortality. Additionally, in another study aimed at assessing other primary outcomes, haemoglobin levels were still identified as significant predictors of mortality in COPD.74
Given these impacts on morbidity, mortality, and quality of life, it would be reasonable to assume that anaemic states in COPD lead to significantly increased healthcare resource utilisation. In fact, some authors have approached this issue, mostly by characterising the increase in hospitalisations and respective length of stay. In several of the previously mentioned studies, anaemia was associated with higher risk of hospitalisation and increased length of hospital stay after adjustment for appropriate confounding factors,24,27,31 thus leading to increased healthcare expenditure. The effects on functional capacity and quality of life might also have substantial socio-economic costs, though these are not as well studied.
Treatment of anaemia in COPDTo date, few studies have investigated the merits of treating anaemia in COPD patients, and specifically the impact of such treatment in their overall, long-term prognosis. Schonhofer et al. evaluated the effects of raising haemoglobin levels through blood transfusions in critically-ill COPD patients in two early publications.75,76 One publication consisted of a controlled trial in which the authors evaluated 20 clinically stable patients with chronic anaemia, comparing 10 COPD patients to 10 patients without lung disease.75 All patients received 1 unit of packed red blood cells for each g/dL that their haemoglobin value was less than the target value. Among the 10 anaemic patients with COPD, there was a significant reduction in mean minute ventilation and decreased work of breathing, whereas patients without lung disease did not show significant changes in respiratory parameters.75 The other publication was a case series of 5 anaemic COPD patients in which weaning from the ventilator had been unsuccessful.76 The authors performed blood transfusions to increase the haemoglobin value to 12g/dL, and then all patients were successfully weaned.76
Given the preponderance of EPO in the regulation of erythropoiesis and its likely involvement in various mechanisms leading to anaemia, EPO-based treatment regimens were also recently studied. In a small study of 12 anaemic COPD patients with high levels of associated comorbidities (e.g. all had chronic kidney disease),77 treatment with a combination of erythropoiesis stimulating agents and intravenous iron resulted in increased levels of haemoglobin, haematocrit, red blood count, serum ferritin, and percent transferrin saturation; patient-reported severity of dyspnoea, as measured through a visual analogue scale was significantly improved.77
Although very limited, these studies provide some indications that correcting anaemia in COPD patients is at least associated with short-term improvements in respiratory measures such as mean minute ventilation, work of breathing, and patient-reported severity of dyspnoea. To the best of our knowledge, the long-term effects of correcting anaemia in COPD patients have not yet been studied in suitably powered studies. Ideally, large, prospective, controlled trials should be conducted to assess the effectiveness and safety of different treatment strategies, taking into account the intrinsic characteristics of the study populations (e.g. outpatients vs. acute exacerbation of COPD) and disease severity/stages of COPD. In any case, in light of the current evidence, it appears reasonable to assume that COPD patients should at least receive the same type of treatment of anaemia as patients without COPD. One could even argue that, given the high frequency and substantial clinical consequences of anaemia in COPD, special efforts should be made to prevent, diagnose, and treat anaemia as early as possible in these patients as a means of improving their overall prognosis.
Potential impact of non-anaemic iron deficiency in COPDIron plays an important role not only in respiration processes, but also in a variety of other cellular mechanisms. Iron deficiency is frequently described in contexts of anaemia as a potential causative factor. However, given the extended role of iron in normal body function, iron deficiency without anaemia has been studied in different contexts of health and disease. Non-anaemic iron deficiency has been reported to confer an increased risk for mortality in the general population78 and to be associated with exercise intolerance in otherwise healthy individuals.79 Similar deleterious effects were found in the context of chronic diseases; patients with heart failure and non-anaemic iron deficiency have increased severity of disease and mortality, and lower exercise capacity.80
In the context of COPD, the impact of non-anaemic iron deficiency has been very poorly studied, despite indications from other fields of the potential relevance of this condition. In COPD patients iron deficiency could potentially lead to worse prognosis through the various mechanisms of iron-deficient erythropoiesis previously described (and mostly related to functional iron deficiency dictated by inflammation) and, consequently, originate anaemia. However, it is also important to consider that non-anaemic iron deficiency could potentially worsen prognosis through other mechanisms, such as the impaired production and function of iron-containing enzymes, which are critical for normal function of respiratory musculature. Therefore, it is important to establish properly the frequency and clinical consequences of iron deficiency, independently from anaemia, in patients with COPD.
Barberan-Garcia et al.81 recently conducted the first study, to the best of our knowledge, to assess the impact of non-anaemic iron deficiency on aerobic capacity in a prospective cohort of 70 non-anaemic COPD patients, who were candidates to participate in an 8-week pulmonary rehabilitation programme. The authors identified a striking prevalence of non-anaemic iron deficiency of 48% in the study population (iron deficiency was defined as ferritin <100g/dL).81 After adjusting for potential confounding variables, patients with non-anaemic iron deficiency showed lower pre-training aerobic capacity and reduced training-induced response.81 These findings suggest that underlying iron deficiency impairs pulmonary rehabilitation. Since no further studies on the effects of iron deficiency correction are available, it is not possible to ascertain whether iron supplementation would be beneficial for these patients. In the context of heart failure, correction of iron deficiency irrespective of anaemia showed improvements in morbidity, mortality, and quality of life,82 which can be seen as an indication of possible beneficial effects for patients with COPD. But, additional studies need to be conducted to definitively validate the use of iron supplementation in patients with non-anaemic iron deficiency.
Assessing iron status and treating iron deficiencyIn chronic inflammatory conditions such as COPD, establishing iron status is particularly challenging, because the classic measures of iron status—ferritin, transferrin saturation, and total iron binding capacity—are known to be significantly altered by inflammation. New measures, such as the soluble transferrin receptor show some promise in providing a more accurate picture of iron status in these states. But, due to their novelty, these are not widely available in clinical practice and international laboratory standards for these measures are yet to be established.83
To overcome the difficulties in using classic measures of iron status, slightly adjusted definitions for assessing iron status have been used in some studies. In contexts of inflammation such as COPD, ferritin levels <100g/dL and transferrin saturation <20% are considered compatible with a state of iron deficiency.83 Going one step further, by combining iron status assessments with haemoglobin levels (generally defined as low if <12g/L in women and 13g/L in men), one can devise four different types (i.e. combinations) of anaemia/iron deficiency in COPD. Iron-deficiency anaemia (i.e. absolute iron deficiency) is characterised by low haemoglobin (levels mentioned above), transferrin saturation <20% and ferritin <100g/dL; anaemia with functional iron deficiency is characterised by low haemoglobin, transferrin saturation <20% and ferritin 100–300g/dL; anaemia without iron deficiency is characterised by low haemoglobin, transferrin saturation >20% and ferritin >300g/dL; and non-anaemic iron deficiency is characterised by normal haemoglobin and transferrin saturation <20% and ferritin <100g/dL.83
Treating iron deficiency in COPD—either in the presence of anaemia or in the form of non-anaemic iron deficiency—has not been sufficiently studied up to this point. Therefore, treatment decisions should be individualised, with consideration for the risk/benefit of such intervention for each patient. Overall, there are indications that iron deficiency (even irrespective of haemoglobin level) has negative impact on patient prognosis and, therefore, it should in principle be looked for and corrected for most COPD patients. Close-monitoring treatment response and tailoring iron supplementation to individual patient needs might be important, since excessive iron supplementation can also lead to oxidative stress and inflammation, which would contribute to actually worsening health status.
Given the fact that systemic inflammation is expected to reduce oral iron absorption (via increased secretion of hepcidin), intravenous (IV) iron supplementation might be the most appropriate treatment regimen in COPD. Some forms of IV iron supplementation, namely ferric carboxymaltose and iron sucrose have already been studied in other contexts of functional iron deficiency, such as heart failure,84 but specific studies in COPD populations should be conducted to provide assurance of effectiveness and measures of safety for this particular population.
DiscussionAnaemia is a relevant comorbidity in COPD, the impact of which is often underappreciated in the clinical setting. Accumulating evidence indicates that anaemia is an important comorbidity in COPD populations, but some specific aspects of the relationship between COPD, anaemia, and iron deficiency warrant further studies.
Estimates for the prevalence of anaemia in COPD patients remain inconsistent. In some respects, it could be expected that these estimates would vary significantly among different patient populations since the health status of COPD patients at different diseases stages will be substantially different. In this review, we presented 4 different types of COPD patients, for the purpose of prevalence measures. Stable COPD outpatients were the first group, in which lower prevalence of anaemia would be expected given that this group encompasses, generally, patients with mild disease and under proper medical follow-up and, at present, most studies have reported relatively lower prevalence of anaemia in this group. The second group included patients with acute exacerbations, which would be expected to present much higher prevalence of anaemia. This group includes patients with augmented inflammatory response, which can lead to anaemia and dysregulation of iron homeostasis resulting in iron deficiency. Additionally, this group might also include patients with respiratory failure that have frequent exacerbations and therefore present worse overall health status, favouring development of conditions such as anaemia. Most studies in this patient population showed, in fact, a very much increased prevalence of anaemia, affecting up to a third of patients; still two studies fell outside this trend and reported prevalence below 10%. The third group consisted of patients enrolled in general population studies, which could range from very mild to very severe COPD depending on the composition of each specific study sample. Interestingly, two studies showed prevalences more consistent with the inpatient acute exacerbation setting and the remaining two studies were more consistent with outpatient stable COPD setting, which are possibly attributable to their underlying population samples. The fourth group consisted of patients under longer-term oxygen treatment or non-invasive ventilation. These patients might present worse health status prior to treatment, but after long-term therapy—as assessed in these studies—could be expected to remain stable. The studies were consistent with this view, showing prevalences similar to that of stable outpatients. Therefore, overall, the prevalence of anaemia appears to increase with disease severity and with worse overall health status. But, further large-scale, prospective clinical studies with standardised consensus definitions of anaemia would be of interest to establish, with a greater degree of certainty, the actual prevalence of anaemia at different stages of the disease.
Among the different mechanisms that have been proposed as causes of anaemia and/or iron deficiency, those of inflammatory origin have been given the main role in the COPD setting. These mechanisms are both supported by theoretical claims based on the current knowledge of anaemia of chronic disease mechanisms and on clinical findings of altered inflammatory markers in COPD populations. Nonetheless, it is also important to consider other mechanisms, especially since some of those can actually be modifiable, such as nutritional deficiencies and theophylline treatment.
Anaemic states in COPD patients are associated with various deleterious clinical consequences, including decreased respiratory function and exercise capacity, impaired quality of life, increased mortality, and increased overall healthcare expenditure. These associations should be taken into account in clinical practice, particularly to support the inclusion of anaemia and iron status assessments as a means to improve COPD patient care.
The impact of iron deficiency in COPD, irrespective of anaemia, is not as well studied, but this state, per se, might have important implications for this population, since it impacts on production of red blood cells and respiratory enzymes. There are indications from other comparable fields (e.g. heart failure) that iron supplementation could have beneficial impact of patient prognosis and, thus, this treatment strategy should be individually considered according to each patient's risk/benefit profile.
In conclusion, anaemia and iron deficiency are relevant comorbidities in COPD patients with established negative impact on overall morbidity, mortality, and quality of life, which, given the prevalence of COPD, can have substantial societal consequences. Special efforts should be made to improve diagnosis, treatment, and prevention of anaemia and iron deficiency in COPD patients. These patients should receive at least the same care as other patients presenting with these conditions. Further studies need to be conducted to definitively establish the effectiveness of anaemia/iron deficiency treatment strategies in the context of COPD, to provide the basis for more specific guidelines on the management of these conditions.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article
Conflicts of interestThe authors declare no conflicts of interest related to this article.
The authors thank Tiago Campos, MSc (ARC Publishing) for providing editorial assistance in the preparation of this manuscript. These services were supported by an unrestricted grant from OM Pharma SA; the company had no role in the development of this manuscript.