Dear Editor
Community acquired pneumonia (CAP) remains the deadliest infectious disease worldwide, especially at the extremes of life and Streptococcus pneumoniae continues to be its most important pathogen.1 The role of combination antibiotic therapy with a macrolide in patients with Streptococcus pneumoniae severe pneumonia, admitted to hospital, although commonly recommended, is still controversial. Identification of patients who might benefit from this strategy is crucial to maximize its benefit whilst reducing antimicrobial overuse, bacterial resistance pressure and toxicity. Positive effects have been previously reported in patients with invasive mechanical ventilation,2 severe CAP3 and with bacteremia,4 although these studies have been carried out in the intensive care unit (ICU) population and the same benefit may not apply to the general population. Moreover, as the population admitted to the hospital is also changing (patients are commonly older and often present comorbidities), this deserves further clarification.
We performed a multicenter study addressing the outcomes of patients admitted with Streptococcus pneumoniae CAP. The study protocol was approved by the Hospital Vila Franca de Xira Ethical Committee at their 25-1-2019 meeting. Informed consent was waived due to the retrospective, observational only, nature of the study. All Ethical Committee of participating centers approved the submitted protocol.
We included 797 adult patients (53.4% male, mean age 72.4±16.5 years, 92.5% with at least one comorbidity) admitted to one of the 4 participating centers, between 2015 and 2018, with microbiological documented Streptococcus pneumoniae (either bacteremia or urinary antigen) CAP. Bacteremia was defined as a clinical and radiological syndrome consistent with pneumonia and ≥1 blood culture(s) positive for Streptococcus pneumoniae.
ICU admission was recorded in 18.8%. Demographic and clinical data, along with antimicrobial therapy, were collected. Outcome data included length of hospital stay, 30-day and 1-year all-cause mortality. Patients were split according to the presence of pneumococcal bacteremia (N=240, 30.1%). Their characteristics are presented in Table 1.
Characteristics of subjects with or without bacteremia.
| Bacteriemia | No | Odds Ratio (95% CI) | P Value | |
|---|---|---|---|---|
| Age (years) | 71.3±15.8 | 72.9±16.8 | 0.195* | |
| Time of symptoms before admission (days) | 2 [1-4.3] | 3 [1-5] | 0.037‡ | |
| CRP max (mg/dL) | 29.3±12.3 | 21.5±11.8 | <0.001* | |
| Diabetes | 28.2 | 26.5 | 1.09 [0.78-1.53] | 0.667† |
| Hypertension | 44.4 | 48.8 | 0.84 [0.62-1.14] | 0.283† |
| Smoking | 17.5 | 18.5 | 0.93 [0.63-1.38] | 0.766† |
| COPD | 15.5 | 18.1 | 0.83 [0.55-1.24] | 0.418† |
| Atrial Fibrillation | 24.2 | 17.6 | 1.50 [1.04-2.16] | 0.034† |
| Cachexia | 4.8 | 5.9 | 0.80 [0.41-1.60] | 0.616† |
| Malignant Neoplasm | 9.1 | 7.6 | 1.23 [0.72-2.1] | 0.483† |
| ICU admission | 27.0 | 15.3 | 2.04 [1.42-2.95] | <0.001† |
| IMV | 9.1 | 15.7 | 1.67 [0.95-2.93] | 0.093† |
| NIMV | 15.1 | 10.6 | 1.50 [0.96-2.33] | 0.078† |
| RRT | 13.5 | 12.1 | 1.13 [0.72-1.76] | 0.644† |
| Multilobar involvement | 39.0 | 38.3 | 1.03 [0.76-1.41] | 0.875† |
| Sepsis | 45.8 | 50.4 | 0.832 [0.62-1.13] | 0.248† |
| Hospital length of stay (days) | 13.8±11.9 | 10.8±8.5 | <0.001* | |
| Hospital mortality | 26.6 | 14.0 | 2.23 [1.54-3.23] | <0.001† |
| 30-day mortality | 26.2 | 16.3 | 1.83 [1.27-2.63] | 0.001† |
| 1-Year mortality | 38.5 | 30.4 | 1.43 [1.05-1.96] | 0.028† |
Data presented as %, unless otherwise stated; Continuous variables are presented as mean ± standard deviation or median [interquartile range] according to data distribution; CRP - C reactive protein; COPD – Chronic obstructive pulmonary disease; IMV – Invasive mechanical ventilation; NIMV – Non invasive mechanical ventilation; RRT – Renal Replacement therapy.
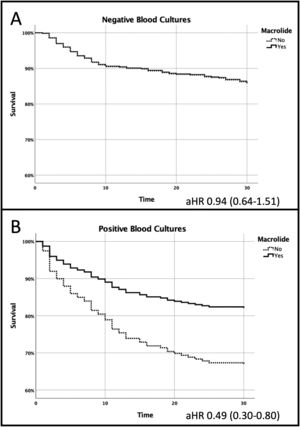
Cox proportional Hazards (HR), along with the 95% CI, was used for assessment of combination antimicrobial therapy with a macrolide, for patients with and without bacteremia.
Mean hospital length of stay was 11.7±9.8 days. The overall 30-day all-cause mortality was 19.2% (32.2% at 1-year follow-up). Patients with bacteremia had higher 30-day all-cause mortality (26.2% vs. 16.3%, age adjusted Hazards Ratio [aHR] 1.84; 95% CI 1.33-2.53) and 1-year all-cause mortality (38.5% vs. 30.4%, aHR 1.43; 95% CI 1.05-1.96). Combination of a ß-lactam plus a macrolide was given to 459 patients (57.6%), 57.1% of those with bacteremia and 57.8% of those without (p=0.88). This proved to be beneficial but only for patients with bacteremia (30-day all-cause mortality 18.8% vs. 36.1%, aHR 0.49 95% CI 0.30-0.80, p=0.004) - Fig. 1. After 1-year of follow up, patients with bacteremia, who received combination antimicrobial therapy with a macrolide, still had lower all-cause mortality, 31.3% vs. 48.1%, p=0.009.
A 30-day Mortality benefit was found in patients who received combination antimicrobial therapy with a macrolide but only in those with pneumococcal bacteremia (panel A); No differences were found in those without bacteremia (panel B): Age adjusted hazards ratio 0.49; 95% CI 0.30-0.80 and 0.94; 95% CI 0.64-1.51, respectively.
The benefit of combination antimicrobial therapy with a macrolide in patients with bacteremia was also found in a large 2007 retrospective study,5 even in patients who received only 24h of a macrolide.5 However, this study failed to provide a control group. The same benefit, improved survival of patients with pneumococcal bacteremia with combination antimicrobial therapy, was noted in another small study, but only in the most severe group. However, the population included was younger and healthier than ours, with an all-cause mortality rate of only 16.9%.4
The reasons for the benefit of macrolides may be related to its non-antibiotic properties, namely a potential “immunomodulatory” effect, although this needs further clarification.6 Persistent inflammation probably plays a contributing role in a worst short- and long-term prognosis in patients with CAP,7 especially related with an increased incidence of cardiovascular diseases. In our cohort 18.3% of patients discharged alive from the hospital died during the 1-year of follow-up, slightly higher than previously reported.8 It should be noted that our population was older (71±16.8 vs. 63 years old) and age is a well-known risk factor for long term mortality.
Our study has some limitations. It is retrospective and included all hospitalized patients diagnosed with Streptococcus pneumoniae CAP. However, there was no systematic patient assessment on admission, and a significant number may have been missed. Moreover, although collection of blood cultures is common practice in patients with CAP who require hospital admission, previous use of antimicrobials or failure to collect blood while still in the emergency department may have contributed to a misclassification. Also, our database included only patients admitted to the hospital between 2015 and 2018, before the SARS-CoV2 pandemic. However, we believe that no significant changes have been made to the approach to patients with pneumococcal CAP.9 Finally, we did not collect all patient’ clinical and laboratory data on hospital admission and severity imbalances between groups may have occurred.
In conclusion we presented a large cohort of patients with pneumococcal CAP. Isolation of Streptococcus pneumoniae bacteremia was associated with high 30-day and 1-year all-cause mortality. On the other hand, patients with bacteremia who received combination antimicrobial therapy with a macrolide had lower 30-day mortality, but this benefit was not found in those with negative blood cultures.
Financial supportThis work was supported by a research grant from Merck Sharp & Dohme Corp., a division of Merck & Co., Inc., Kenilworth, NJ, USA [IIS# 60150] under the Investigator Studies Program.
The content of this publication reflects only the views of the authors. The sponsor had no role in the analyses or interpretation of the data.
Authors contributionsJoão Gonçalves Pereira acts as guarantor of the integrity and accuracy of the data.
JGP, DL, PM, FF designed the study; AS, PVR, LC, RA, IS, MC, PM acquired the data and performed literature search; JGP, AG check the data for missing or implausible values; JGP, PM, IS, DL, AG analyse and interpret the data; JGP, PM, FF drafted the manuscript; JGP, AS, AG, PM, FF, DL revised the manuscript for important intelectual content; JGP, AG provided the statistical expertise. All authors review and approved the final manuscript.