Low physical activity (PA) levels have a negative impact on the health status of patients with Chronic Obstructive Pulmonary Disease (COPD). Smartphone applications (apps) focused on PA promotion may mitigate this problem; however, their effectiveness depends on patient adherence, which can be influenced by the technological features of the apps. This systematic review identified the technological features of smartphone apps aiming to promote PA in patients with COPD.
MethodsA literature search was performed in the databases ACM Digital Library, IEEE Xplore, PubMed, Scopus and Web of Science. Papers including the description of a smartphone app for PA promotion in patients with COPD were included. Two researchers independently selected studies and scored the apps features based on a previously developed framework (38 possible features).
ResultsTwenty-three studies were included and 19 apps identified, with an average of 10 technological features implemented. Eight apps could be connected to wearables to collect data. The categories ‘Measuring and monitoring’ and ‘Support and Feedback’ were present in all apps. Overall, the most implemented features were ‘progress in visual format’ (n = 13), ‘advice on PA’ (n = 14) and ‘data in visual format’ (n = 10). Only three apps included social features, and two included a web-based version of the app.
ConclusionsThe existing smartphone apps include a relatively small number of features to promote PA, which are mostly related to monitoring and providing feedback. Further research is warranted to explore the relationship between the presence/absence of specific features and the impact of interventions on patients’ PA levels.
Chronic obstructive pulmonary disease (COPD) is the third leading cause of death worldwide1 and the seventh leading cause of disability-adjusted life years.2 The Global Burden of Disease Study 20153 estimated 174 million cases of COPD globally and its prevalence is expected to increase in the upcoming years.4,5
Physical activity (PA) levels are reduced in most patients with COPD when compared to healthy peers,6 which have a negative impact on clinical outcomes (such as an increased risk of exacerbations, hospitalizations and mortality7) and can lead to the development of comorbidities, which further contribute to physical inactivity.8 Additionally, a decrease in PA levels over time across all severity grades of COPD has been demonstrated, in parallel with a worsening of lung function and health status.9 It has been suggested that increasing daily PA might be equally effective as smoking cessation to prevent morbidity and mortality in patients with COPD, although the consequences of continuous inactivity in this population might still be underestimated.10 Recent research has highlighted that even small changes in PA (e.g., increasing activity by 600 steps per day11) can be clinically meaningful for patients.10
The Global Initiative for Chronic Obstructive Lung Disease (GOLD)5 highlights the potential of technology-based interventions to provide accessible means to enhance PA in daily life. The value of technology became even more relevant during the COVID-19 pandemic, where several in-person healthcare services had to be adapted to reduce the burden on healthcare systems.12 Mobile applications (apps) aiming to promote PA may be a promising solution to help patients with COPD acquire healthy habits in their own environment, as smartphones are ubiquitous in daily life.13,14 In 2021, 67% of the world population subscribed to mobile services; of those, 75% were smartphone connections, and an increase to 84% is expected by 2025.15 Smartphone devices as a tool to promote PA in patients with COPD have shown small improvements in the short-term and no effects in the long-term.16 Poor adherence may be caused, among other things, by problems related to the device, affecting the effectiveness of these apps.16 Thus, technological features are a fundamental aspect of patient adherence and app success.17 Studies have suggested that different features can influence the effectiveness of PA promotion apps, such as goal setting adapted to the users’ context and progress14,18 and social media features,19 and these aspects have been identified as enablers of PA engagement in patients with COPD.20,21 Recent reviews have described the most common features in smartphone apps for PA promotion.17,18,22–26 However, these studies did not address apps designed for populations with specific health conditions, such as COPD. A review from Donevant and colleagues27 explored the relationship between the app features and PA outcomes in mobile health studies involving chronic respiratory diseases, diabetes and hypertension, but they have not stratified the findings by health condition. Given the added complexity and challenge in PA promotion and behavior change in patients with COPD,21 research is warranted to explore how smartphone app features have been implemented in this specific population.
The aim of this systematic review was to identify the smartphone apps developed, tested and/or implemented for PA promotion in patients with COPD, as well as to identify the technological features implemented by those apps, based on the framework of Mollee et al. (2017).26 This framework was developed to ensure a good coverage of the important features of apps aimed to encourage PA behavior.
MethodsEligibility criteriaThis systematic review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines28 and the protocol was registered at PROSPERO (ref. CRD42021252975).
For this review, physical activity was defined as any bodily movement produced by skeletal muscles that requires energy expenditure, including leisure time, transport/commuting time, exercise or as part of a person's work.29
Eligible studies had to include the design/development, description, testing and/or implementation of a smartphone app aiming to promote physical activity in patients with COPD. Original papers published in scientific journals or conference proceedings (observational and interventional studies), in English or Portuguese, were considered. Studies that presented smartphone apps for patients with chronic respiratory diseases were also included if COPD was considered. Studies with smartphone apps aiming to promote PA alone or in combination with other components (e.g., nutritional advice) were also included.
Exclusion criteria consisted of: 1) studies targeting populations other than COPD; 2) smartphone apps with a different aim (e.g., breathing retraining); 3) studies describing tablet-based applications; 4) non-original papers (e.g., reviews, commentaries to papers, theses); 5) abstracts without a full paper.
Information sources and search strategyA systematic literature search was performed in the electronic databases ACM Digital Library, IEEE Xplore, PubMed, Scopus and Web of Science. Search strings combined terms relating to smartphone apps, COPD and physical activity. Searches was restricted to studies published in English and Portuguese. The search was conducted from January 01, 2007 (i.e., the year that Apple launched the first smartphone) until January 21st 2022 for all databases except for the Web of Science, which was conducted at January 28th 2022 due to technical issues. The combination of terms was used with database-specific filters for language, date, and type of study to be included. More details on the search strategy are available in the Supplementary Material S1. All references were uploaded to and sorted in the Mendeley reference manager version 2.75.0 (Mendeley Ltd., London, UK). References of relevant studies were also screened for potential studies.
Selection processTwo independent reviewers (JS and NH) performed the initial screening of the articles based on their title and abstract, according to the eligibility criteria. In case of doubt, an independent full-text screening was made to decide its inclusion. The scoring codes were: “0” for exclusion, “1” for inclusion and “2” for uncertainty. The level of inter-rater agreement was calculated using the Cohen's kappa statistic, which can be interpreted as follows: 0 – 0.20 as indicating no agreement, 0.21 – 0.39 as minimal level of agreement, 0.40 – 0.59 as weak, 0.60 – 0.79 as moderate, 0.80- 0.90 as strong, and above 0.90 as almost perfect level of agreement.30 Disagreements were resolved by consensus. If agreement could not be reached, a third reviewer (JC) was consulted. If there was more than one study using the same app, all studies were included.
Data collection and synthesisThe information was retrieved based on the full-text and supplementary material of the papers, when available. Data were recorded in a structured table-format according to the following topics: first author's last name and year of publication; study design and country; name of the smartphone app (if available); operating system; web portal, if existing (for the patient and/or healthcare professional access); use of a wearable technology, if any; aim of the app and its key features. All data were extracted and summarized by one reviewer (JS) and checked by the other authors.
Then, the technological features for PA promotion were assessed in each smartphone app, according to the framework of Mollee et al.26 This framework is composed of 48 items/subitems which are organized into 38 features distributed in six categories: Measuring and monitoring, Information and analysis, Support and Feedback, Adaptation, Social, and Other. The 38 features are identified at the lowest level of the items/subitems in each category – for example, the item “(a) Does the app ask for input from the user?” of the category Measuring and monitoring has 2 subitems (“i. Does it ask for input to set up a personal profile?”; “ii. Does it ask for input to log activities?”); therefore, it includes 2 features. This hierarchical organization into categories, items and subitems enables the analysis of the apps in different levels of abstraction (i.e., the lower the level, the greater detail is provided), ensuring good coverage of relevant features.26 The list of the categories, items and subitems is provided in the Supplementary material S2. One additional category of the framework was not considered (Usability), as it required the reviewers to interact with the app.
The framework was implemented in a spreadsheet program where two reviewers scored each app independently, assigning for each item the score “1” (if the answer to the item was “yes”) or “0” (if the answer was “no” or if it was not clear whether the app included the described feature) (Supplementary material S2). If an item consisted of several subitems, it was scored “1” if at least one of the subitems was also scored a “1”, and “0” otherwise.26 If a paper described the presence of a certain item, but not specified that feature (i.e., it did not provide a clear answer to the subitems), a “n.s.” (not specified) was registered in the subitems and a “1” in the corresponding item. Discrepancies between reviewers’ scores were resolved by consensus. Inter-rater agreement was assessed with Cohen's kappa by calculating the agreement for each app separately and calculating the average. Items classified with “n.s.” were considered as “0” for this purpose.
Both the number of features per app and the number of apps which implemented each feature were determined. For the number of features per app, if an item was divided into several subitems, only these subitems were considered in the count, to avoid double counting of features. In cases where the subitems were scored with “n.s.”, the corresponding item was considered in the count, to ensure that the general feature was not overlooked. This strategy was also used for the number of apps with a specific feature.
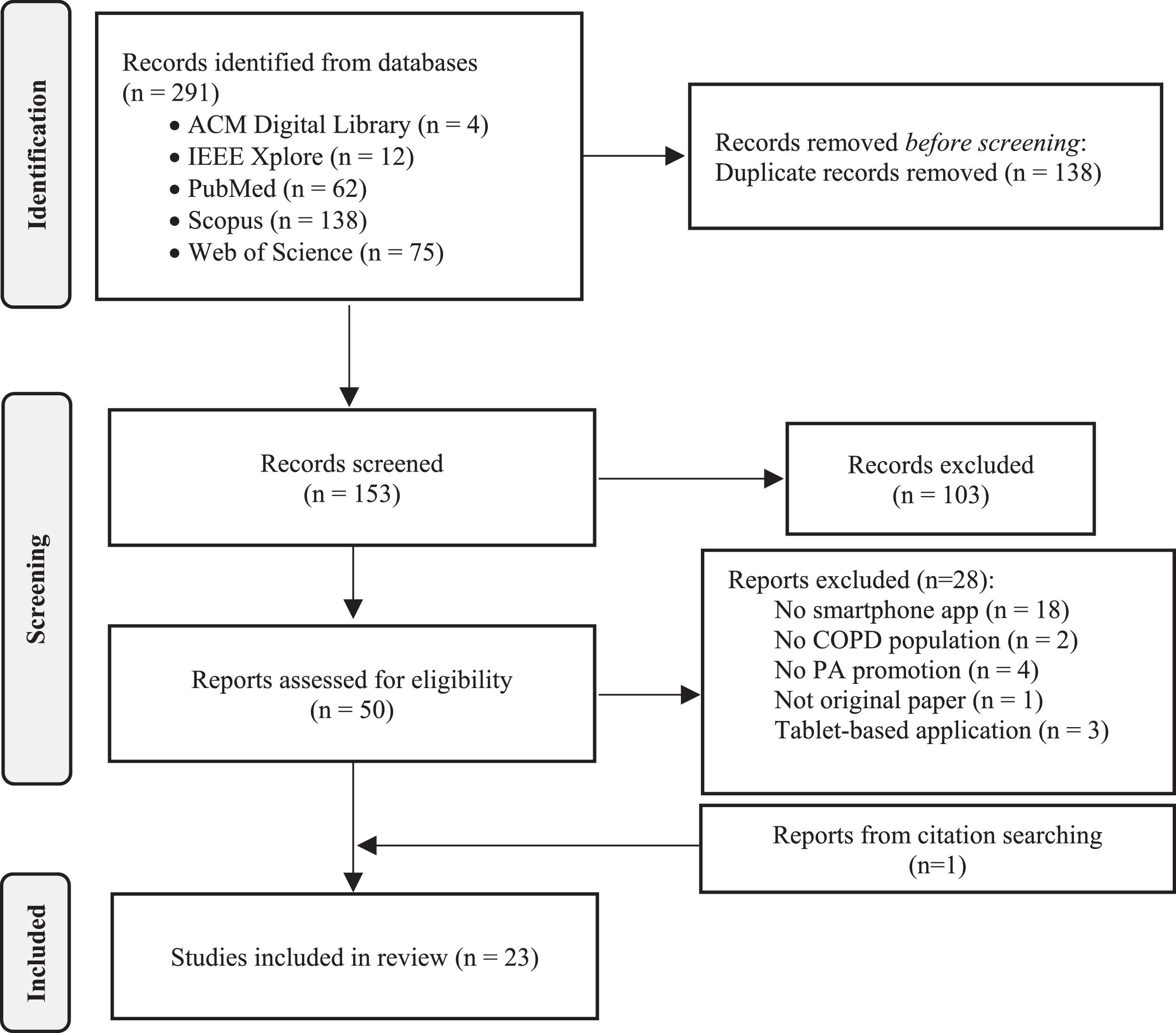
ResultsStudy selectionA total of 291 records were identified from searches in the five databases. After removing duplicates, 153 records were identified for title and abstract screening. Then, the full text of 50 papers was assessed for eligibility. Of these, 28 reports were excluded for the following reasons: did not include the design/development, description, testing and/or implementation of a smartphone app aiming to promote PA (n = 18); target population other than COPD (n = 2); the smartphone app had a different aim (n = 4); it was not an original paper (n = 1); the app was designed for a tablet (n = 3). One study was included when searching the references of relevant studies. In total, 23 studies were included in this review (Fig. 1). The level of inter-rater agreement was moderate (Cohen's kappa= 0.6).
Study characteristicsOf the 23 included studies, four were randomized controlled trials (RCTs),31–34 six were feasibility/pilot RCTs35–40; four were feasibility studies41–44; six were validation studies45–50; and three were protocols of an intervention/ RCT51–53 (Table 1).
Characteristics of the studies (n = 23) and the 19 smartphone apps, ordered by the last name of the first author (except when two papers are presenting the same app).
| Author (year) | Type of study | Country | App | O.S. | Web Portal | Wearables | Aim of the app | Key features | |
|---|---|---|---|---|---|---|---|---|---|
| Patient | Health professional | ||||||||
| An et al. (2021)48 | Validation study | China | COPDTrack | - | - | - | Smartband | Digital PR | Physical activity featuresRunning map with option to choose a preferred pathMonitoring and visualizing real-time body condition information (not specified) and option to send it to the physicianDigital 6MWT with monitoring from a smartbandDigital PR exercise coursesVisualization of progressOther featuresCreating and visualizing peak flow reports and option to send it to the physicianChat to communicate with the healthcare providerPatient-reported outcomes (not specified) |
| Bartlett et al. (2017)45 | Validation study | United Kingdom | Music and Maps System | - | - | - | - | PA promotion | Physical activity featuresSelf-goal setting (walking) and activity trackingUsers can choose music to listen while walkingFeedback on PA levels presented in a satellite map, as a summary table or in a calendarLocal exercise facilities highlighted on the map |
| Bartlett et al. (2017)45 | Validation study | United Kingdom | Online Community System | - | - | - | - | PA promotion | Physical activity featuresSocial support to build a community of like-minded users to encourage PA (walking)Communication between peers, while encouraging interaction through competition and collaborationUsers can track their activity and share information with othersPoints given when users achieve their goalsVirtual rewards (stars or trophies) and “real-world” rewards (vouchers or donating money to charity) |
| Bartlett et al. (2017)45 | Validation study | United Kingdom | Virtual Coach System | - | - | - | - | PA promotion | Physical activity featuresDialogue support with a virtual coach (static picture) which uses the user's name to personalize the system and encourage interactionProgressive goal setting (walking) defined by the coachOption to change goals, with coach's suggestionsReminders to complete the activity (optional)Audio encouragement from the coach while walking (optional)Feedback provided in graphs with praise and encouragement from the virtual coachSuggested exercise plans with increasing daily walking goals to reach an overall goal |
| Bentley et al. (2020)35 | Feasibility RCT | United Kingdom | SMART-COPD | Android | - | - | Smartband | PA promotion/ exercise training after PR | Physical activity featuresSelf-goal settingActivities include walking and daily exercises based on standard PR exercisesVideos demonstrating exercisesFeedback provided in graphs: time walking (using the smartphone accelerometer) and exercising (manual timer), number of stepsUsers gain flower petals as they get closer to the goal (daily walk) |
| Chong et al. (2021)49 | Validation study | New Zealand | mPR app | Android iOS | - | - | - | Digital PR | Physical activity featuresThree levels of exercise prescription - all levels include warm up, walking program, and resistance training for upper and lower limbs using hand-held weights. Level one also includes balance exercises• Automated messages based on user performanceTailored exercise videosDigital 1-min sit-to-stand test with a reminder to complete it every 2 weeksProgress visualization with circles that fill according to completion of daily activity targetsOther featuresAction plan for respiratory exacerbationsCAT questionnaire with a reminder every 2 weeksLung model visualization videoInformation for family members on how to support the loved one with chronic respiratory diseaseRelaxation audio |
| Whittaker et al. (2021)39 | Pilot study | ||||||||
| Demeyer et al. (2017)31 | Multicentre RCT | Belgium, Greece, United Kingdom, Switzerland, The Netherlands | PROactive Linkcare | Android | - | Monitor patients’ PA and usage | Step counter | PA promotion | Physical activity featuresMorning reminder of the daily target (number of steps) which remains the same throughout the weekEvening audio reminder for the user to send wirelessly the data collected by the step counter. Feedback is received, including a graph with daily performance and an educational tipWeekly feedback (Sunday) including proposals for being active based on the action plan, if the target was not reachedIf the patient reaches the target, the readiness to increase it is questioned and the target is increased if the patient agrees (automated or manual goal setting)Daily and weekly encouraging messages using both text and pictogramsBooklet containing home exercises (strengthening and stretching, 3 difficulties) to do on days with bad weather |
| Loeckx et al. (2018)41 | Feasibility study (secondary data from a RCT - Demeyer et al. (2017)) | ||||||||
| Deng et al. (2021)40 | Pilot study | China | - | Android iOS | - | Evaluate patients’ condition, adjust exerciseprescription and review exercise-related data to deal withdeviations | - | Digital PR | Physical activity featuresExercise-related data and early warning information is sent to healthcare professionals, who can adjust the prescription. Prescriptions can also be modified automaticallyDaily personalized exercise prescriptions and a weekly plan, including the exercise type, frequency, intensity and time, and the ability to record and upload exercise-related dataWalking speed monitoring using a rhythm audioFeedback to motivate patientsOther featuresSelf-management and symptom monitoringFollow-up visit and communication |
| Ding et al. (2019)51 | Protocol of the intervention | Australia | MH-COPD programme | Android | - | Yes (n.s.) | - | Self-management | Physical activity featuresAutomatic recording of steps with smartphone-embedded motion sensorsPersonalized prescription of the initial goal and automatic progressionDaily motivational messages according to the steps and goal achievedOther features10 health educational videos provided at scheduled times, with a questionnaire at the end for knowledge self-assessmentLinks to relevant educational webpagesDaily self-management of symptoms, with predefined severity levels. Recorded symptoms are automatically compared with those in the previous dayAutomated notification when increased symptom scores are detected to use the electronic COPD action plan(For smokers) Smoking behavior self-record and a self-defined goal, with motivational messagesVideos on how to use the prescribed inhaler(s) |
| Guerra-Paiva et al. (2021)53 | Protocol of the intervention | Portugal | DPO2 | Android iOS | - | Yes (n.s.) | Pulse oximeter, smartwatch (GPS tracker), sphygmomanometer | Digital PR | Physical activity featuresPatient progress tracking by counting the exercise time, number of exercises completed and effort scalesOutdoor activities tracking consisting of moving time, distance traveled and effort scales (walking, power walking, zumba, gymnastics)Exercise log, schedule and reminders, with recommended and established exercise programs (including demonstration photos)Real-time feedback on SpO2 and heart rateNotification during exercise when values of heart rate and SpO2 fall outside pre-defined valuesOther featuresPeriodic scheduled videocalls, with extra-videocalls if neededPanic button to contact relatives or local authorities when feeling unwell, and fall detection through device's accelerometer and gyroscope with an automatic alarmAppointment alarmsFrequently asked questions including visual and audio guidesAdvice on respiratory disease and medical care |
| Kwon et al. (2018)32 | RCT | South Korea | Efil breath | Android | Monitor patients’ data and display a list of patients with SpO2 <90% and modified Borg ≥7 | Pulse oximeter | Exercise training and monitoring | Physical activity featuresTwo apps consisting of:Fixed exercise regimen, with 6 levels of walking distance (600 m, 1200 m, 1800 m, 2400 m, 3000 m and 3600 m; level automatically increased based on user achievements)Interactive exercise regimen, with 12 levels of walking distance (initial intensity: 80% of the 6MWT; metronome to guide the walking speed; adjusted according to the modified Borg scale)Measurement of exercise compliance, heart rate and SpO2 (using the oximeter)Smartphone vibration when SpO2 <90%Guided resistance/strength exercises available with audio-guides and links to external demonstration videosExercise diary to summarize daily results | |
| Park et al. (2020)33 | RCT | South Korea | SASMP | Android | - | - | Pedometer (data inserted manually) | Self-management | Physical activity featuresEducational material and videos on how to perform home exercisesRecording of the time and type of exercise, and step count (pedometer)Exercise record and graphs with previous resultsDisplay of the PA/exercise goal (expert prescription) and achievement rateGroup-text and communication with other users and research teamOther featuresEducational material and videos on how to use inhalersFont size of all content can be adjustedRecording of symptoms, inhaler use, and healthcare use due to exacerbationsGraphical summaries of symptomsProfessional monitoring and automatic alert messages |
| Pereira et al. (2016)46 | Validation study | Portugal | Exercit@rt | Multiple platforms | Create exercise sessions, schedule meetings and exchange messages | - | Finger oximeter | Exercise training and monitoring | Physical activity featuresAccess restricted to users with an account on the web platformPreviously recorded sessions in the web platform can be chosen in the appConnection of the app with the oximeter to receive alerts based on SpO2% and heart rate (audio and visual warning)Monitoring and geolocating common daily activities (walking, running, biking, shopping, gardening, etc.)Performance graphs with distance travelled, heart rate and SpO2% dataPossibility to check the average values during a given periodPerformance values possible to share in social networksExplanatory texts and images/animations for each exercise |
| Rassouli et al. (2018)42 | Feasibility study | The Netherlands, Austria, and Switzerland | Kaia COPD | AndroidiOS | - | - | Smartwatch | Self-management | Physical activity featuresDaily exercises according to the user profile (strength and mobility training in short videos; education; mindfulness techniques)Monitoring of exercise duration and intensity, depending on user's exercise capacity (self-test in the app)Weekly activity goals based on individual fitness levelRecording of daily PA: number of steps (smartband), completed training sessions (patient's records)Reminders of activity goals via push notificationsOther featuresDisease progression tracked daily with a ‘feeling thermometer’ in a 10-point scale and dyspnea assessment on a Borg scaleVideos with the correct inhaler techniqueCoach chat for motivational and technical questions |
| Spielmanns et al. (2020)52 | Protocol of a RCT | The Netherlands and Switzerland | |||||||
| Simmich et al. (2021)36 | Pilot RCT | Australia | Grow Stronger | - | - | Monitor patients’ progress, send encouraging messages and restrict exercises | - | Exercise training | Physical activity featuresOne upper-body and one lower-body activity (+ difficulty and intensity) commonly used in COPD rehabilitation, chosen by the user every dayExercise time recorded, the timer can be paused/resumed/stoppedPerceived dyspnea reported after each activity using the modified Borg scale2 parallel game modes to be used together or separately:Single player mode - theme of growing a gardenCooperative multiplayer game mode - theme of a caravan trip around Australia. Activities completed by the other players in the last 24 hours are displayed, to whom the user can send a pre-set “cheer” messageRewards for completed activitiesOther features: COPD-related educational information provided on a daily basis |
| Spina et al. (2013)47 | Validation study | The Netherlands | COPDTrainer | Android | - | - | - | Exercise training | Physical activity featuresSmartphone attached in a holster to a body part involved in the exercise, to be used as an exercise monitoring/feedback deviceIllustrations guiding smartphone attachments and exercise performanceTeach-mode: allows therapists to personalize the system for a trainee under direct supervision and exercise parameters are stored for further use in the Train-modeTrain-mode: the exercises are arranged in a to-do list for the user to complete without therapist's supervisionInertial motion data recorded from the smartphone sensors and processed in real-time to count exercise repetitions and detect errorsAcoustic feedback on repetitions and errorsSummary display of the exercise performance |
| Tabak et al. (2014a)38 | Pilot RCT | The Netherlands | Activity Coach | Android | - | - | triaxial accelerometer | PA promotion (app)Self-management (web portal) | Physical activity featuresAccelerometer and smartphone worn on the hip to measure 3D body movements to estimate energy expenditureSensor connected with the smartphone by BluetoothFeedback on cumulative activity presented in a graph with a reference line identifying the goal to be achievedMotivational cues every 2 hours, based on the difference between the measured activity and the reference line - short summary of activity behavior and advice on how to improve it, in three possible ways:Encouraging (>10% deviation below reference line)Discouraging (>10% deviation above reference line)Neutral (≤10% deviation with reference line)Questions about self-perceived activity performance, dyspnea and fatigue (Visual Analogue Scale and/or multiple choice)Other features: Web portal with a symptom diary for self-management of exacerbations and an overview of the measured PA levels |
| Tabak et al. (2014b)37 | Secondary analysis of a Pilot RCT - Tabak et al37 | ||||||||
| Tabak et al. (2013)50 | Validation study | Netherlands, Norway and Romania | - | - | |||||
| Vorrink et al. (2016a) 34 | RCT | The Netherlands | - | Android | - | Monitor patients’ data, adjust goals and send text messages | - | PA promotion | Physical activity featuresDisplay of daily steps in real time in a quantitative and qualitative formatPersonalized PA goalAutomated persuasive messages and an emoticonWidget on the home screen showing PA statusVisual bar combining the amount and intensity of steps (goal met when a stripe reaches the green area), absolute number of steps and current advice on PAGraph with information of PA over time |
| Vorrink et al. (2016b)43 | Feasibility Study | ||||||||
| Yonchuk et al. (2021)44 | Feasibility study | United States,United Kingdom, and Germany | Respercise® | Android | - | - | Smartband (data inserted manually) | Digital PR | Physical activity featuresRelevant information on PA, exercise, goal setting and safety, with feedback and notificationsSmartband used for daily step count and strengthening exercises conducted thrice weekly using elastic bands“Walking dashboard” allows users to enter daily steps, see the trend of their step count over 7 days and receive encouragement messages/ awards towards their daily goals“Strength dashboard” with subsections for each of the 4 strengthening exercises including written instructions and a demonstration video, patients’ progress and an “add result” button: bicep curls, step-ups, upright rows, and sit-to-standStep count goals automated according to the app's algorithm, depending on participant data entry of completed exercises and daily PAOther features“Administration” section restricted to the site staff to setup the individual program for each participant“How to Respercise” section with information and educational content about COPD, the Respercise exercise program and lifestyle“Frequently Asked Questions” and “End User License Agreement” sections, contact information |
Abbreviations: 6MWT – six-minute walk test; CAT, COPD Assessment Test; COPD - chronic obstructive pulmonary disease; n.s. - not specified; O.S. - operative system; PA - physical activity; PR - pulmonary rehabilitation; SpO2 - peripheral oxygen saturation.
Studies were conducted in several countries: five studies in The Netherlands34,37,38,43,47; two in the United Kingdom35,45; two in Australia36,51; two in South Korea32,33; two in Portugal46,53; two in China40,48; two in New Zealand39,49 and six studies included several countries31,41,42,44,50,52 (Table 1).
Apps for physical activity promotion in COPDFrom the studies selected, 19 apps were identified. Table 1 provides a description of the features and characteristics of each smartphone app. One study45 described three different apps, and five apps were described in more than one study (mPR app,39,49 PROactive Linkcare,31,41 Kaia COPD,42,52 Activity coach,37,38,50 and one app with no specific name34,43).
Five of the apps aimed to promote PA in daily life,31,34,41,43,45 five apps aimed to promote structured PA (e.g., pre-set walking distance/time, resistance/strength exercises),32,35,36,46,47 and thirteen aimed to promote patient self-management including PA promotion.33,37–40,42,44,48–53 Self-management apps also contained educational material, disease/symptom monitoring, alerts, a chat, or a smoking self-record with motivational messages.
Thirteen apps31–35,37,38,41,43,44,47,50,51 were developed for the Android operative system, six apps39,40,42,49,52,53 for both Android and iOS operative systems, and one app46 was available on multiple platforms (not specified). The operative system was not reported in three apps.36,45,48
Eight apps31,32,35,37,38,41,42,46,48,50,52,53 could be connected to wearable devices (e.g., activity tracker, oximeter) to collect data which were then transmitted to the app. In two apps,33,44 data from the activity trackers had to be inserted manually.
One of the studies50 included an additional digital intervention called Orange Submarine to motivate patients to exercise, with the goal of catching the greatest possible number of air bubbles, directing a submarine towards them, in a pattern adapted to the patient's exercise goal. This game provides real-time feedback about the score, heart rate and peripheral oxygen saturation, and includes a sensor node with a triaxial accelerometer to control the submarine. This intervention was not described further in this review because it was not a smartphone app but rather a computer game (thus, only the app used in this study was described).
Technological features of the apps for physical activity promotionBelow we provide a summary of the number of technological features included in each smartphone app, as well as the number of apps with the same feature. The features of the apps are also available in the Supplementary Material S2, based on the framework of Mollee et al.26 Inter-rater agreement was moderate (Cohen's kappa = 0.6; values for each app are presented in the Supplementary Material S3).
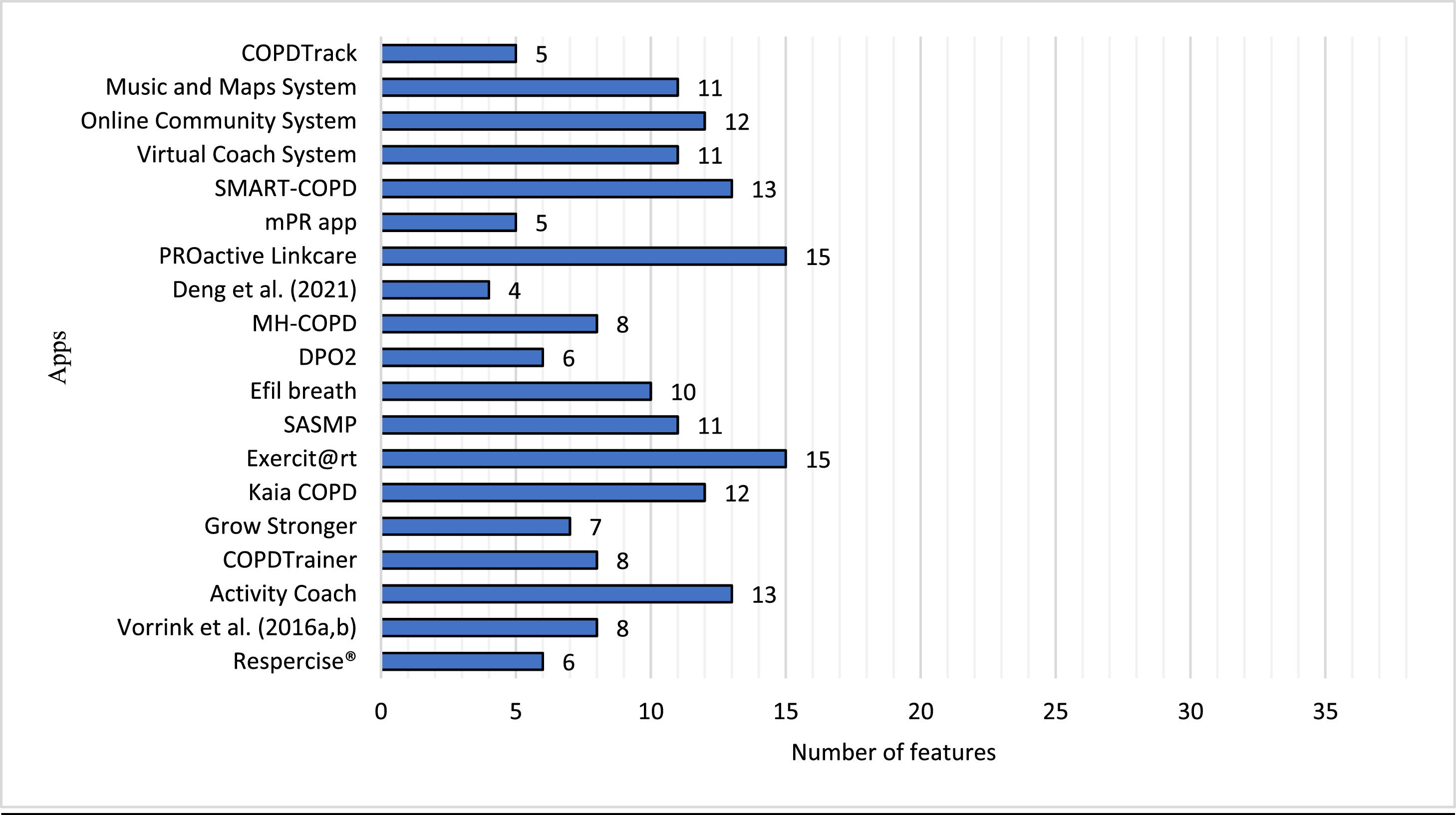
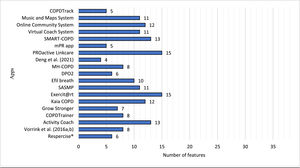
Number of physical activity promotion features per appFig. 2 shows the number of features identified for each of the 19 apps analyzed. The average number of features implemented in the apps was 10 out of 38 possible features (26%). The app with the lowest number of features was the app developed by Deng et al.,40 with only 4 features identified (11%). The PROactive Linkcare31,41 and Exercit@rt46 apps had the highest number of features implemented, both with 15 features (approximately 40% of the maximum possible number of features).
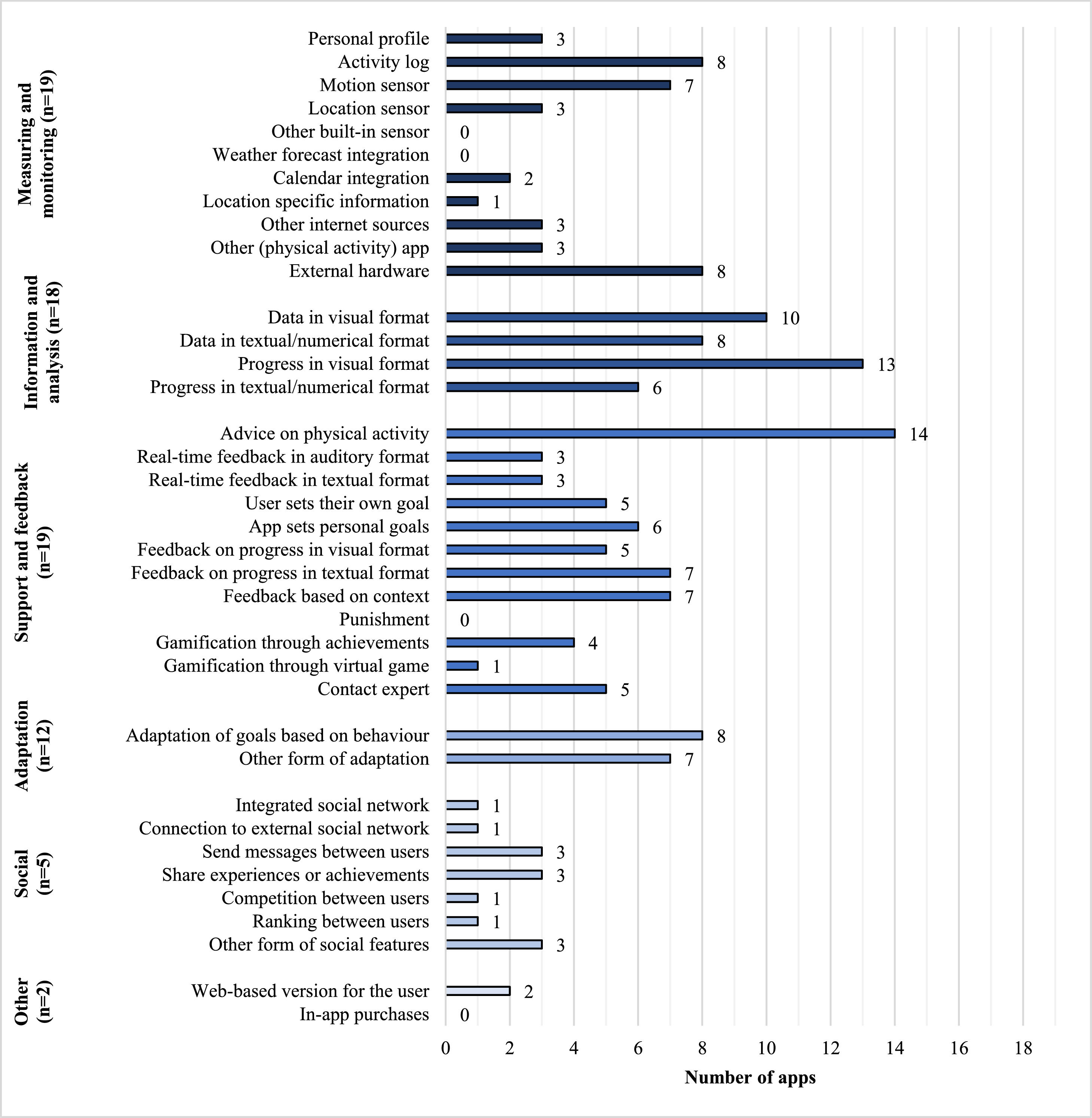
Number of apps with a specific featureThe number of apps which implemented each of the 38 possible features is shown in Fig. 3. The categories Measuring and monitoring and Support and Feedback were present in all apps (i.e., included at least one of the features in the category), Information and analysis was included in eighteen apps, Adaptation in twelve apps, Social features in five apps, and Other features were implemented in just two apps. Overall, the most implemented features were “progress in visual format” (n = 13), “advice on physical activity” (n = 14) and “data in visual format” (n = 10), which were implemented in at least half of the apps.
Within the Measuring and monitoring category, the most frequent features were the activity log by the user (n = 8), the use of external hardware (n = 8) and the use of a motion sensor (e.g., built-in gyroscope and/or accelerometer; n = 7). None of the apps implemented the features “other built-in sensor” or “weather forecast integration”.
In the category Information and analysis, progress in visual format (e.g., graphs and/or calendars) was the most employed feature (n = 13), and progress in textual/numerical format (e.g., list of logs and/or statistics) was the least common feature (n = 6).
In the category Support and feedback, advice on PA was the most implemented feature (n = 14), and ‘punishment’ for not meeting goals/commitments was not present in any app. As for Adaptation, the two existing features (i.e., adaptation of the goal or other form of adaptation) presented a similar frequency (n = 8 and n = 7, respectively).
Within the Social category, the features “send messages between users”, “share experiences or achievements” and “other form of social features” were present in three apps. The remaining features of this category were implemented in one app only.
Finally, only two apps had a feature in the category Other, which included a web-based version of the app available for the users where they could view more detailed information.
DiscussionThis review identified the technological features implemented in smartphone apps designed to promote PA in patients with COPD, along with the scores of these features using the framework developed by Mollee et al.26 The 19 apps identified in the present study included a relatively low number of features for PA promotion, with an average of 10 features per app (i.e., 26% of the 38 possible features), which were mostly related to PA monitoring, data analysis, feedback/support and adaptation. These findings may be useful in the development of interventions aiming to promote PA in patients with COPD using mobile solutions.
A possible explanation for the low number of features included in each app was previously pointed out by Mollee et al.26 The authors hypothesized that it could be related to the technical and conceptual complexity of the implementation of some features. For example, in their study, Vorrink et al.43 mentioned that battery life posed a major problem while developing the app, thus not all desired options, such as GPS-tracking and continuous measurement, were possible to implement due to the limited capacity of the smartphone battery. In addition, as shown in Table 1, several apps were not specific for PA promotion; therefore, they may have scored low in the PA features framework due to the primary aim of the app (i.e., self-management), where PA promotion is only a module. For example, the MH-COPD programme51 registered eight PA-related features; however, there was a substantial number of features related to other self-management modules (e.g., education, symptom management, smoking behavior). Nonetheless, the authors decided to include these apps since they include a component of PA promotion.
This review showed some heterogeneity in the categories/features implemented in the smartphone apps – while some features or categories were frequently applied, others were rarely or never implemented in the apps. Considering the most implemented features, the ‘advice on physical activity’ is particularly important since information and education on PA have been identified in the literature as an enabler for PA promotion following Pulmonary Rehabilitation, by increasing individuals’ understanding of the associated health benefits.21 The ‘Information and analysis’ features (i.e., presentation of the user's PA in visual/textual format) were also common. These features are important when promoting active lifestyles in patients with COPD, as they can recognize their personal improvements and may be more engaged/motivated by the outcomes, thus feeling more empowered to maintain the PA levels achieved.21 Some apps supported the use of external hardware, such as smartbands for daily PA tracking.31,32,35,37,38,41,42,46,48,50,52,53 This feature may allow greater flexibility in monitoring PA in specific situations, e.g., when the patient is at home and leaves the smartphone on the table or elsewhere, as smart bands can still collect PA data. However, connection or synchronization issues between the external sensor and the app were identified in three studies.35,41,44 These issues should be considered when developing apps for PA promotion as they can lead to lower patient adherence to the app.
The features related to the category Adaptation were also frequently implemented, which differs from the PA apps for healthy adults identified in the work of Mollee and colleagues,26 where these were one of the least addressed features.26 This could indicate that there is a greater effort to customize the features of PA promotion apps developed for patients with COPD. In fact, personalization features, such as adapting the user's goals based on individual behavior/needs, have shown to increase the effectiveness of PA apps in the general population.14,23 Furthermore, personalization and self-goal setting have been described as enablers for PA engagement in patients with COPD,20 the latter being especially relevant, as self-regulatory strategies are not only identified as determinants of PA in these patients,20,21 but also as an important aspect within behavior change techniques, helping people to modify their PA levels.54 This may be addressed in future research on PA promotion apps for patients with COPD.22,23 In addition, it would be useful to identify the factors that influence patients’ PA behavior, described in the literature (i.e., barriers and enablers20,21), which are addressed in each app to understand whether the apps consider the (partially) modifiable factors when promoting PA and/or adjust recommendations based on non-modifiable factors.
Weather forecast integration was not implemented in any of the apps, even though converging evidence has demonstrated that adverse weather (e.g., temperature, rain) and air quality conditions can have a negative impact on COPD symptoms55 and PA levels.20,56 In a RCT that implemented a smartphone app to promote daily PA,31 included in this review, patients were reminded they could exercise at home on days when the weather prevented them from going outside; however, these reminders were sent manually by the researchers. Thus, integrating weather forecast information in the apps could alleviate this barrier by providing opportunities to engage in PA even in case of bad weather. Furthermore, the apps could be connected to wearable devices that would detect changes in air pollution levels and provide appropriate advice (e.g., to exercise at home or select the route with lower levels of air pollution). There are several commercial wearable/portable solutions for environmental monitoring in the market, although their accuracy is still questionable.57 As sensor/wearable technology is rapidly advancing, it is possible that such solutions will exist in future apps for PA promotion to enable better choices of where and when to perform activities and provide personalized recommendations.57,58
Calendar integration was implemented less often, although this feature could help patients establish a routine and, therefore, be an important strategy to create PA habits.20,21 The number of apps with the possibility to contact an expert, and with social features, was scarce. These features may be relevant considering the importance that social support has on PA engagement in patients with COPD.59 Individuals’ relationships with others may have a large impact on their PA levels – feeling understood and encouraged to be physically active by family members, friends and peers can facilitate an active lifestyle.20,21 Moreover, support from healthcare professionals may be important for individuals, as it can create a sense of trust.21
This review has some limitations that need to be acknowledged. Firstly, the authors did not consider the Usability category, as described in the framework developed by Mollee et al.26 In this category, the apps were scored for clarity and attractiveness, which required interaction with the app. In the present review, the authors excluded this category because the apps were not possible to download, and the authors could not provide a reliable scoring simply by analyzing the images provided in the articles (when available). Nevertheless, this aspect could be of interest, since it is not known how the clarity and attractiveness of the apps may influence patient adherence, and if the number of features in the app are related to its usability. Mollee et al.26 found that easy-to-find information in an app was not compromised by the number of implemented features, but there was a moderate positive correlation between the number of features and the attractiveness score.
Secondly, the fact that none of the apps were downloaded or used by the authors restricted the number of features identified. Often, studies did not provide a detailed description of the apps, including only information about the fundamental features; therefore, it is possible that certain features were overlooked in the present study. This is also a weakness of the research in this area – although there were 19 apps identified to promote PA in patients with COPD, most are still not available online for clinical use.
Thirdly, the scoring process of the technological features using the framework of Mollee et al.26 was not always easy to perform, as shown by the results of inter-rater agreement available in the Supplementary material S3. Specifically, some questions (i.e., items and subitems) were not described in sufficient detail in the original paper to make a clear decision on whether a specific feature was present or not in the smartphone app, which sometimes led to some subjectivity in the process. For example, the two raters had slightly different interpretations of the question “Does the app give the user feedback based on their physical/social context?” (Support and feedback category), concerning the definition of “physical”. One reviewer considered this as a “environmental context”, and the other as a “biological context”, being the latter the agreed interpretation. Even so, the average inter-rater agreement was moderate, which shows that scoring the apps features using this classification framework is feasible.
Finally, the analysis of individual, clinical and sociodemographic characteristics of patients who participated in studies implementing the smartphone apps was beyond the scope of this review, although it could provide important information on who would benefit most from this type of technology, as there is no ‘one size fits all’ approach. A previous study found that patients with COPD who use mobile apps in daily life are younger and have a higher physical capacity than those who do not use them (age: 64.2 ± 8.9 vs. 69.2 ± 6.3 years; six-minute walking distance: 462.9 ± 91.7 vs. 414.9 ± 82.3 m, respectively), although 73% of the sample reported being interested in using a COPD-specific app for PA promotion, if it was available.60 Future research should identify the best candidates for interventions using mobile solutions.
Among the strengths, this review was the first to address technological features of smartphone apps to promote PA in patients with COPD. It identified the most used features and the ones that may need more attention in future development of these apps.28 Future research should address the impact of these apps on patients’ PA levels, and how the results relate to the presence/absence of specific technological features of the apps. Likewise, it would be important to adjust the features of the apps based on the factors associated with PA engagement in patients with DPOC (e.g., symptoms, having a dog, taking care of grandchildren).61–63
ConclusionsThis review identified the technological features of 19 smartphone apps designed to promote PA in patients with COPD, based on the framework developed by Mollee and colleagues.26 The apps included 10 out of 38 possible features, with the most prevalent features being “advice on physical activity”, “data in visual format” and “progress in visual format”. Weather forecast integration, calendar integration, possibility to contact an expert, and social features were less often implemented, although they may be relevant to improve patients’ PA behavior. Future research should explore the impact of these apps on patients’ PA levels, as well as the effect of the presence/absence of specific technological features on the results.
Declaration of Competing InterestThe authors declare there is no conflict of interests.
This work is part of a project funded by FEDER - Fundo Europeu de Desenvolvimento Regional by COMPETE 2020 – Programa Operacional Competitividade e Internacionalização (POCI) and national funds by Fundação para a Ciência e a Tecnologia (FCT), entitled “OnTRACK project - Time to Rethink Activity Knowledge: a personalized mHealth coaching platform to tackle physical inactivity in COPD” (POCI-01-0145-FEDER-028446, PTDC/SAU-SER/28446/2017). SF and NH are being financially supported by PhD fellowships DFA/BD/6954/2020 and 2021.05188.BD, respectively, funded by FCT/MCTES, FSE, Por_Centro and UE. PM acknowledges the support provided by the FCT with the PhD fellowship. The authors acknowledge the financial support provided by FCT to their research unit – Center for Innovative Care and Health Technology (UIDB/05704/2020).