Leiomyomas account for less than 2% of all benign lung tumors. Only one third is endobronchial in location, usually presenting as primary solitary lesions and airway obstruction findings. Literature on primary endobronchial leiomyomas is therefore scarce, with a few more than 100 cases being reported.
We describe a case of a 44-year-old female that presented with asthma like symptoms and an obstructive pneumonia, due to a right main bronchus primary leiomyoma that was successfully resected using Nd:YAG laser through rigid bronchoscopy.
The purpose of this case is to enhance the rarity of primary endobronchial leiomyoma diagnosis and report the relevance of laser resection in its definitive treatment. A brief review on lung leiomyomas is discussed over the text.
Os leiomiomas representam menos de 2% de todos os tumores benignos do pulmão. Apenas um terço tem origem endobrônquica, geralmente apresentando-se como lesões primárias solitárias condicionando obstrução da via aérea. A literatura sobre os leiomiomas endobrônquicos primários é portanto escassa, incluindo o relato de pouco mais de 100 casos.
Descreve-se o caso de uma doente de 44 anos com sintomas sugestivos de asma brônquica e uma pneumonia obstrutiva no contexto de um leiomioma primário do brônquio principal direito, que foi removido com sucesso utilizando o Nd:YAG laser através da broncoscopia rígida.
Pretende-se realçar a singularidade do diagnóstico de um leiomioma endobrônquico primário e a relevância da ressecção laser no seu tratamento definitivo. Uma breve revisão sobre os leiomiomas pulmonares é apresentada ao longo do texto.
Primary lung leiomyomas are rare benign tumors of smooth muscle origin. Of all surgically excised tumors from the lung, about 1.9% are benign1 and of these, only less than 2% are leiomyomas.2,3
The majority of lung leiomyomas, approximately 51%, are located in the parenchyma, endobronchial accounts for 33% and tracheal for the remaining 16%.3
In women, parenchymal leiomyomas can occur as primary lung lesions or as a result of a benign extrauterine growth of smooth muscle cells, an entity called benign metastasizing leiomyoma (BML).4 Endoluminal leiomyomas are usually described as primary solitary lesions.
Literature on primary endobronchial leiomyomas is scarce, with a 2009 review reporting only 108 cases.5 Although rarity and nonspecific clinical presentation may impose diagnostic challenge, an excellent prognosis is usually obtained when removal by bronchoscopic techniques is feasible.
We present a case of successful laser resection of a right main bronchus (RMB) primary leiomyoma causing asthma-like symptoms and an obstructive pneumonia in a middle age female.
Case PresentationA 44-year-old Portuguese white female presented with sporadic dry cough and wheezing for over three months. She had been treated with inhalation therapy for bronchial asthma without improvement. Exercise dyspnea appeared on the previous two weeks. The patient denied other symptoms, namely constitutional ones. Her medical past history was negative, including gynaecologic problems, and she was a lifetime non-smoker.
Physical examination was unremarkable, except for chest auscultation, which revealed diminished breath sounds on the right hemithorax.
Blood test showed an increased C-reactive protein (4.7mg/dl), without any others abnormalities.
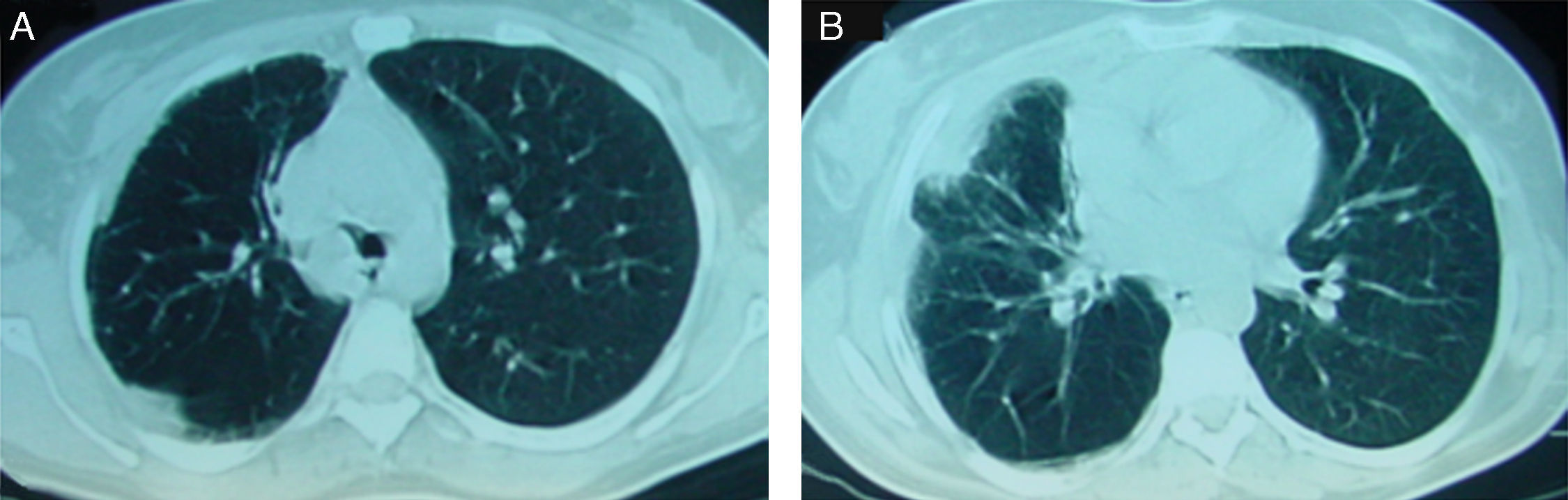
Chest computed tomography (CT) demonstrated a RMB well defined occlusive opacity and a right middle lobe consolidation with air bronchogram along with a small homolateral loculated pleural effusion (Fig. 1A, B).
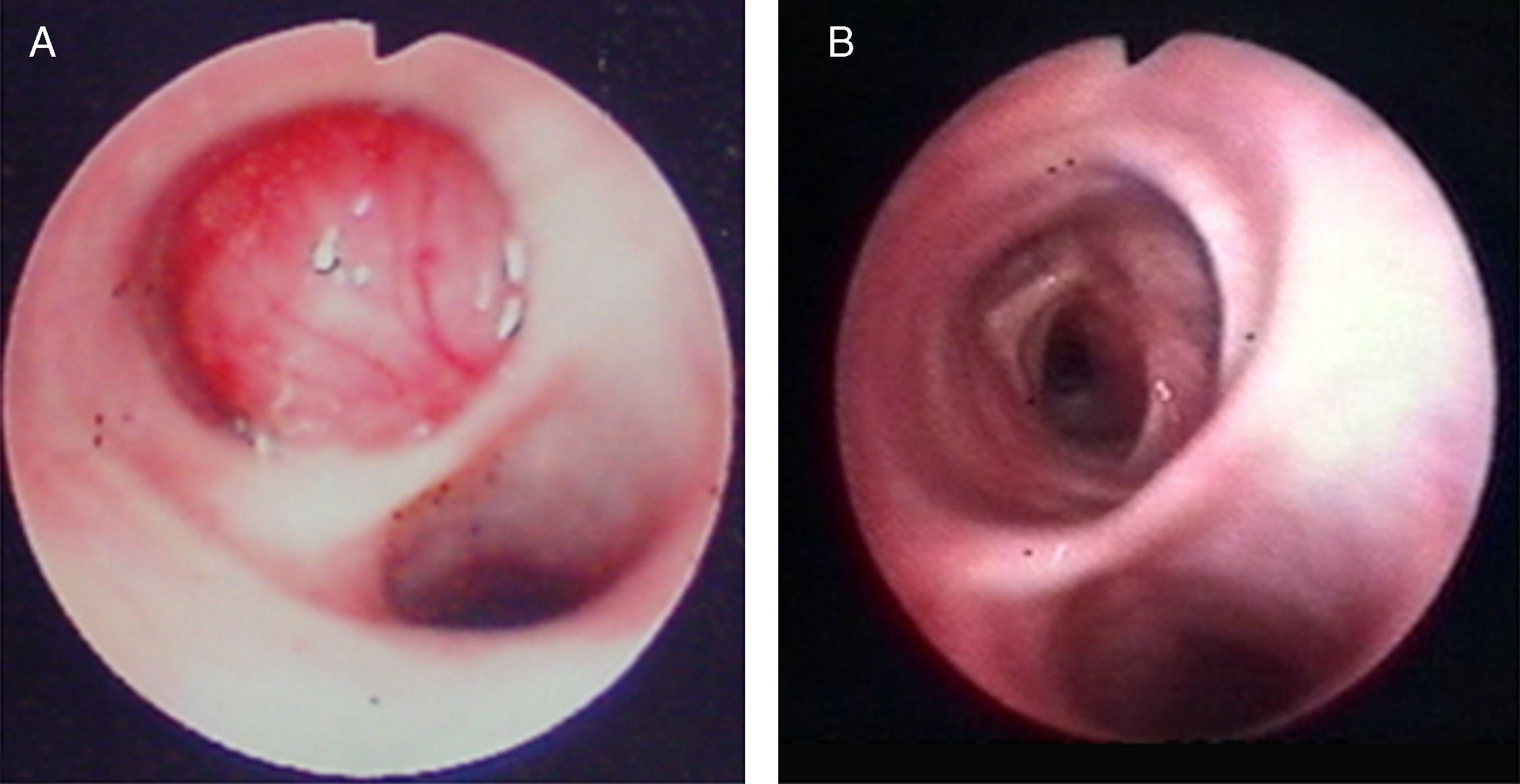
Flexible bronchoscopy revealed a round smooth and vascularised lesion in the RMB near the main carina, arising from medial wall of the bronchus and causing occlusion of more than 90% of its lumen (Fig. 2A).
Rigid bronchoscopy was performed with diagnostic and therapeutic purposes, given the limited base of tumor insertion and patency of the remaining bronchial tree. Mechanical debulking along with neodymium: yttrium-alluminum-garnet (Nd:YAG) laser allowed successful resection of the lesion with restoration of normal bronchial caliber in one session (Fig. 2B).
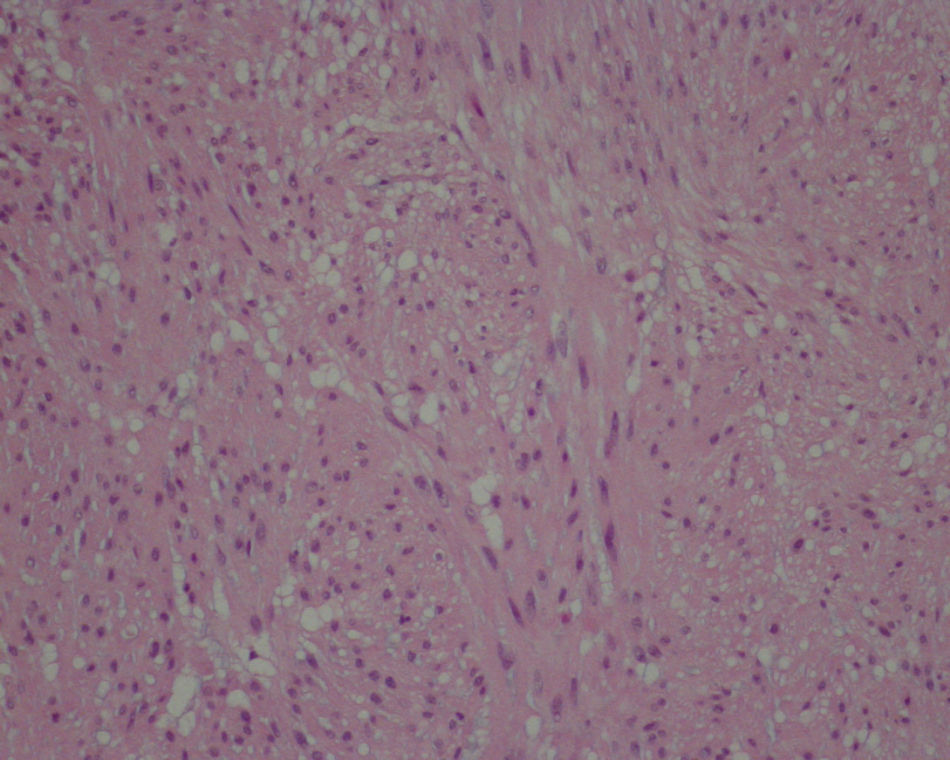
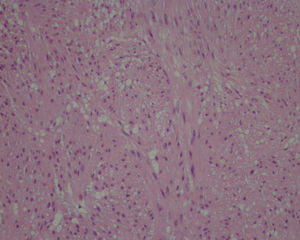
Histopathology was consistent with a lung leiomyoma (Fig. 3) showing fusocellular proliferation of spindle cells with cigar-shaped nuclei, eosinophilic cytoplasms, no atypia or areas of necrosis, no mitotic activity and diffuse positivity for actin and desmin and weak for vimentin on immunohistochemistry stain.
There was also no clinical evidence of other organs involvement, namely in the uterus, which was confirmed by gynecological and ultrassonografic examination, and estrogen receptors were negative in histology.
The patient was also given empiric antibiotics with clinical and radiological resolution, and spirometry was normal. After 2 years of follow-up, the patient is well and no endoscopic signs of relapse were detected.
DiscussionEndobronchial leiomyomas are rare benign tumors of the lung, usually presenting as primary solitary lesions arising from bronchial tree smooth muscle layers. The review of 108 primary endobronchial leiomyomas showed that they occur with no anatomic bronchial predilection, are common in middle aged (35±3 years) patients and affect equally both sexes.5 In contrast, lung leiomyomas, in general, occur predominantly in women, and this may reflect the previous overreporting of pulmonary leiomyomas secondary to the variant of BML.5
The majority of patients with endobronchial leiomyomas have respiratory symptoms due to partial or total obstruction of airways.3 Cough is the most common symptom, wheezing and dyspnea may also be present, sometimes being erroneously described as bronchial asthma, like in this case.6 Obstructive atelectasis and pneumonia can occur later in natural history of occlusive endoluminal lesions.3 Bronchiectasis, hemoptisys and even a pneumothorax resulting from air trapped behind the endoluminal lesion were also described.7
Radiology is unspecific and may reveal features of bronchial obstruction. Chest CT can be useful in characterizing lesions and demonstrating endoluminal tumors. Final diagnosis may be achieved with bronchoscopic direct visualization and biopsy of lesions.3
Even so, differentiation of an endobronchial leiomyoma from a BML or a low-grade leiomyosarcoma is especially important. Little or absence of mitotic activity is the most important predictor of benignity of these tumors.4 BML is histologically similar to primary leiomyomas, except that it has estrogen and progesterone positive receptors and usually presents as multiple parenchymal nodules in women with a previous or current history of uterine leiomyomata.4 Since no signs of leiomyomatous disease were found in other organs, and hormonal receptors were negative in histology, our case was considered unrelated and therefore a primary endobronchial leiomyoma.
Treatment of endobronchial leiomyomas, whether symptomatic or not, implies resection,8 which depends on location, size, base of implantation of lesions, as well as secondary lung destruction.1
Given the benign nature of these lesions and long-term outcomes after limited excision, treatment is essentially based on conservative techniques.3,5,8,9 Although lobectomy and pneumonectomy have been commonly used in endobronchial leiomyomas treatment, parenchymal resection should be reserved only for situations in which advanced irreversible destruction secondary to chronic infections occurs.3,5,8,9 Bronchoplasty and bronchotomy were also described as an alternative for lesions arising from the main stem or proximal part of the lobar bronchus. 3 If complete resection is possible, current knowledge favours, however, bronchoscopic intervention with a variety of techniques, including electrocautery, argon plasma coagulation, cryotherapy and laser being documented with good results.5,8,9. Best indications include strictly endoluminal tumors, with limited extent within the endobronchial tree and central location.1,9,10 Except for cryotherapy, the remaining techniques provide a rapidly target ablation.10
Nd:YAG laser assisted mechanical debulking through rigid bronchoscopy has been reported in the literature as safe and effective in curative intent treatment of such benign tumors, with a minor rate of complications when used by training physician.1,9,10 Our patient presented with a right main bronchus primary leiomyoma located immediately below the main carina, with a limited insertion base, which allowed successful Nd:YAG laser resection and an excellent prognosis, avoiding the need for a higher surgical risk procedure.
ConclusionPrimary endobronchial leiomyomas are rare tumors that must be considered when symptoms of bronchial obstruction develop and persist. In women, a secondary leiomyomatous origin must be excluded. Successful laser resection and excellent prognosis can be achieved in limited extent central endobronchial leiomyomas.
Please cite this article as: Vaz AP, et al. Leiomioma endobrônquico primário—ressecção laser endoscópica. Rev Port Pneumol. 2011. doi:10.1016/j.rppneu.2011.01.002.