Tracheal tumors are rare, representing only 0.2% of the respiratory tract malignancies. Chondrosarcoma arising in the trachea was first described in 1959 by Jackson et al. and since then only 20 cases have been described. We report the second documented case of malignant transformation from an endotracheal chondroma, in a 75-year-old woman, and review the literature.
Primary tracheal tumors are rare, 80% are malignant and account for 0.2% of all respiratory malignancies. The most common histologic types are squamous cell carcinoma and adenoid cystic carcinoma, followed by carcinoid tumor, adenocarcinoma, and small cell carcinoma. The remaining tumors are diverse and include chondroma, chondrosarcoma, fibrosarcoma, among others.1,2 Jackson et al. described the first case of tracheal chondrosarcoma in 1959 and since then only 20 cases have been reported (Table 1).3–23 We add a new case leading to a review of the literature.
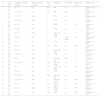
Characteristics of patients with tracheal chondrosarcoma.
| N° | Age, Sex | Symptoms, duration (months) | Tracheal segment involved | Size (cm) | Treatment | Recurrence | Follow-up (years) | Authors, year |
|---|---|---|---|---|---|---|---|---|
| 1 | 32, M | C, 72 | Inf | NR | ER | No | 6 | Jackson et al 19593 |
| 2 | 73, M | D, O, W, 8 | Inf | 2.5 | ER | local | 2 | Daniels et al 19674 |
| 3 | 48, F | C, W, 15 | Sup | 4 | STR | no | 5 | Fallahnejad et al 19735 |
| 4 | 71, M | H, C, D 4 | Med | 3 | STR | no | 5 | Weber et al 19786 |
| 5 | 58, M | D, 24 | Inf | 2 | STR | no | 2.5 | Slasky et al 19857a |
| 6 | 74, M | P, acute | Sup | 2 | STR | no | 1 | Arévalo et al 19868 |
| 7 | 72, M | H, D, 7 | Med | 5 | ELD and STR | no | 0.5 | Matsuo et al 19889 |
| 8 | 54, M | W, D, 1 | Inf | 2 | STR | local, distant | 14 | Salminen et al 199010b |
| 9 | 64, M | D, 36 | Inf | 2.3 | STR | no | 1 | Kaneda et al 199311 |
| 10 | 72, M | D, 36 | Inf | 6.5 | STR | no | NR | Leach et al 199412 |
| 11 | 54, M | W, D, 1 | Inf | 2 | ELD and STR | no | 3.5 | Kiriyama et al 199713 |
| 12 | 84, M | C, D, St, 24 | Med | NR | STR | no | 3 | Hervás et al 199714 |
| 13 | 87, M | D,12 | Med | 3 | ELD and RT | local | 1 | Farrell et al 199815 |
| 14 | 49, M | St, D, acute | Sup | NR | ELD and STR | no | 4 | Aznar et al 200116a |
| 15 | 78, M | D, 3 | Inf | NR | ELD and STR | no | 0.5 | Maish et al 200317 |
| 16 | 34, M | H, D, 8 | Sup | 2.5 | STR | no | 6.3 | Umezu et al 200818 |
| 17 | 72, M | O, D, W, 12 | Sup | NR | ELD and RT | no | 7 | Mendonça 200919 |
| 18 | 34, M | C, W, D, 18 | Sup | 2 | ER and TSR | no | NR | Wagnetz et al 200920a |
| 19 | 35, M | W, D | Sup | NR | ER and TSR | no | NR | Almeida et al 201021a |
| 20 | 63, M | W, D, 6 | Med | NR | ER and TSR | no | NR | Mirza et al 201022 |
| 21 | 74, M | W, D | Sup | NR | TSR | no | NR | Mohajeri et al 201323 |
C, cough; W, wheezing; St, stridor; D, dyspnea; O, orthopnea; H, hemoptysis; P, pneumonia; Inf, inferior; Med, medium; Sup, superior; STR, surgical tracheal resection; ER, endoscopic resection; ELD, endoscopic laser debulking; RT, external beam radiotherapy; NR, not reported.
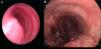
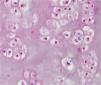
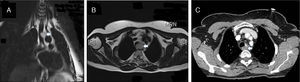
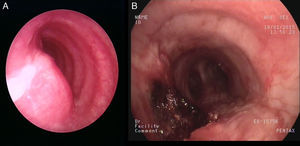
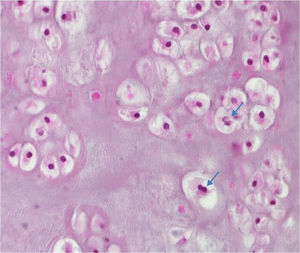
A 75-year-old woman with a past medical history significant for hypertension, diabetes mellitus and carotid artery disease reported having a chronic non-productive cough and dysphagia for about one year. Six years prior to this presentation, she had undergone endoscopic resection of a tracheal chondroma diagnosed during investigations for multiple episodes of respiratory distress mimicking asthma. No further treatment was done at that time. At presentation, a chest-computed tomography (CT) revealed a mass (25mm×30mm×25mm) located in the left postero-lateral wall of the mid-trachea without lymphadenopathy (Fig. 1). Her physical examination and pulmonary functions tests were normal. Gastroesophagoscopy revealed extrinsic compression at 18cm from the dental arch, with normal mucosa. Rigid bronchoscopy confirmed the lesion described in CT, which protruded into the tracheal lumen, occupying less than half of its diameter and covered with regular mucosa. After rigid scissors incision, mechanical debridement and laser application restored normal lumen patency (Fig. 2). Histopathological analysis showed cartilaginous tumoral proliferation with increased cellularity and occasional binucleate chondrocytes as well as necrotic remains, in favor of low-grade chondrosarcoma (Fig. 3). The diagnosis was confirmed by the regional referral center for sarcoma. The case was discussed in our multidisciplinary tumor board and the patient deemed unfit for surgery. At present, 9 months after the second endoscopic intervention, the patient is asymptomatic with stable residual tumor (Fig. 1, panel C).
Chondrosarcoma refers to a group of tumors that consist predominantly of cartilage and can be classified into 3 histologic grades (I, II and III), based on cellularity, atypia, and pleomorphism. The higher the grade, the more likely the tumor is to spread and metastasize.24 Low-grade chondrosarcoma resembles benign cartilaginous tumors, and it is difficult to differentiate the two lesions on the basis of histologic features alone. Extraskeletal chondrosarcoma is uncommon and its location in the airway is more frequent in the larynx.25 Of all tracheal chondrosarcomas (TCS) reported, the tumor was grade II in 4 cases and grade III in one. TCS tend to be slow-growing and in general do not metastasize, in contrast to chondrosarcomas found elsewhere in the body.
Its etiology is still unknown and there is no tracheal segment predilection. Patients’ ages have ranged from 32 to 87 years and only one female patient was previously reported.3–23 Most frequent presenting symptoms are chronic cough and dyspnea, often with associated wheezing potentially masquerading as adult onset asthma or COPD.17,20,23 Unlike previous reported cases, dysphagia was observed in our case, related to an extraluminal growth when the tumor recurred, in contrast to the preponderance of intraluminal obstruction in the initial presentation of most reported cases.
Investigations usually start with a chest X-ray which may show narrowing of the tracheal shadow or mediastinal mass. However, in most cases the chest X-ray is normal. CT imaging allows an accurate location of the lesion and provides information about tumor extension. Calcification is present in 75% of cartilaginous tumors.20 Magnetic resonance imaging may provide a better assessment of the tumor relationship with surrounding structures but its value remains controversial.26
Bronchoscopy is the best method for the diagnosis and offers the opportunity of initial management and allows for surgical planning if indicated. The optimal treatment seems to consist of tracheal sleeve-resection with end-to-end anastomosis. Incomplete resections are at risk of local recurrence with an increased risk of metastatic disease.10
The first 2 reported cases were treated with endoscopic resection alone, whereas surgery followed initial endoscopic laser debulking (ELD) in 7 cases. The majority of cases (n=10) were treated with solely surgical resection. Chemotherapy seems to be inefficient in low-grade chondrosarcoma, but there is no much literature on the subject.27 Historically, chondrosarcoma has been considered as radioresistant but several studies have challenged this notion and radiation may be indicated as an adjuvant therapy after incomplete resection, in tumors considered unresectable, in surgically unfit patients or where there is metastatic disease.25 Two TCS cases have been treated with ELD followed by conventional radiotherapy (RT), both after incomplete endoscopic resection. In the first case, an 87-year-old patient refused surgery and follow-up was limited to one year but there was no obvious progression of the remaining lesion. In the other case, the patient was not deemed a suitable candidate for surgery, and there was no evidence of disease after 7 years of follow-up.
The prognosis of TCS appears excellent if adequate resection is achieved. Local recurrence has been described in 3 cases and may be managed endoscopically or surgically.4,10,15 Salminem et al. reported the only case in which the patient died after malignant transformation of a chondroma, 14 years after the initial diagnosis with metastatic disease. We report, to the best of our knowledge, the second case of tracheal chondroma presenting with malignant transformation during its course.
In conclusion, tracheal chondrosarcoma is a relatively slow-growing lesion that should be treated surgically with tracheal resection. Bronchoscopy is the gold-standard for diagnosis and rigid bronchoscopy with ELD can be the first therapeutic option but can also be definitive when surgery is not an option. Despite the small numbers of cases on which to base opinion, it appears to have an indolent behavior, even when it recurs.
Conflict of interestThe authors have no conflicts of interest to declare.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article
Right to privacy and informed consentThe authors declare that no patient data appear in this article.