Bronchiolitis, asthma and pneumonia are leading causes of hospital admission for acute illness in pediatric population,1 ranking among the top 10 of inpatient costs.2–4 Level of hospital care, both clinical and nonclinical procedures and length of hospital stay (LoS), represent targets for resource use optimization.5
The identification of trends through administrative data sources provides relevant information to understand the epidemiology related to disease burden and interventions, and to optimize resources use and standards of care.2,6,7
We aimed at analyzing central administrative data of acute pediatric hospitalization trends in Portugal for bronchiolitis, pneumonia and asthma, both as primary or secondary diagnosis, over the decade that preceded the publication and implementation of national guidelines for these diseases and the introduction of pneumococcal vaccines.
We collected administrative data (January 2002–December 2012) from the Diagnosis-Related Group database of the Portuguese Central Health System Administration (ACSS) as age-restricted codes from the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) for hospital admissions in mainland Portugal (bronchiolitis codes 466.1, age range 0–23 months; asthma codes 493 and pneumonia codes 480–486). For asthma and pneumonia, children 0 to 17 years old were eligible and data analyzed as 0–23 months and 2–17 years of age.
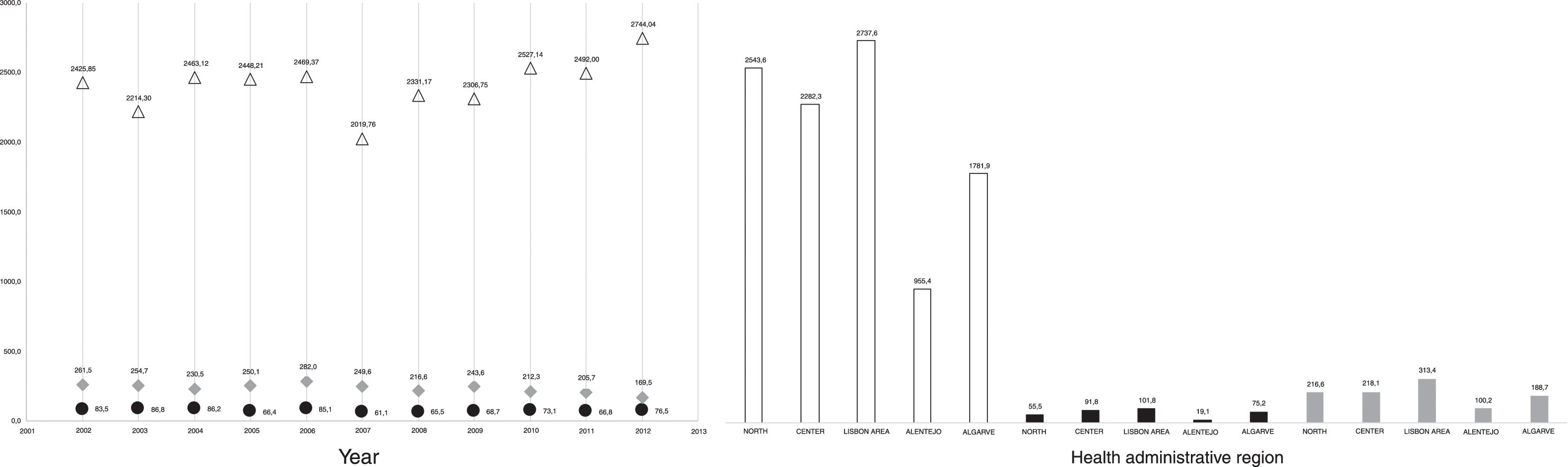
Hospital resource's use was evaluated by mean LoS, severity-related procedures [non-invasive (NIV) or invasive ventilation (IV) use] and inhospital mortality. Portuguese National Institute of Statistics data from 2001 and 2011 Census was used to estimate the yearly hospitalization rate for each diagnosis/100,000 inhabitants, adjusted for age range (Fig. 1).
Bronchiolitis- (white), Asthma- (gray) and Pneumonia- (black) related pediatric hospitalizations in Portugal, 2002–2012. (a) Mean number of admissions per 100,000 inhabitants aged 0–24 months for bronchiolitis and aged 0–17 years for asthma and pneumonia; (b) mean number of admissions per 100,000 inhabitants in the five health administrative regions in Portugal.
Analysis was performed based on the primary discharge diagnosis for each condition. Descriptive analysis of demography was performed. Trends in bronchiolitis, asthma or pneumonia, and yearly and health administrative regions admissions were assessed by bivariate analysis and linear regression (using time as independent variable). Due to personal data protection, and because of low numbers per age group, some data on mortality was not disclosed. IBM® SPSS Statistics v24.0 or Microsoft® Excel v15.39 were used considering a significance level of 5%.
During the 11-year study period 117,857 admissions occurred due to these three-respiratory diagnoses: bronchiolitis (n=52,601), asthma (n=15,315) and pneumonia (n=48,143), representing a mean (SD) of 4732 (357.8) patient admissions/year for bronchiolitis, 1330 (189) for asthma and 4494 (644.1) for pneumonia, as primary diagnosis.
Mean (SD) annual frequency hospitalization was 2448.2 (186.3), 73.1 (9.1) and 243.6 (30.0) for 100,000 children for bronchiolitis, asthma and pneumonia, respectively.
Global hospital admission rate for bronchiolitis showed a small nonsignificant increase in all health administrative regions (r′=22.47, p=0.223), except for the Center (r′=−0.669, p=0.024), whereas for asthma a nonsignificant small decrease (r′=−0.535, p=0.09) occurred, despite a non-statistical significant increase trend in North region and Algarve.
For pneumonia, a statistically significant decrease in global pneumonia hospitalization rate (r′=−7.76, p=0.007) was perceived, maintained on age groups (r′=−0.881, p=0.0 in 0–23 months; r′=−0.515, p=0.105 in 0–17 years), although in Alentejo and Algarve a non-statistical significant increase trend was observed.
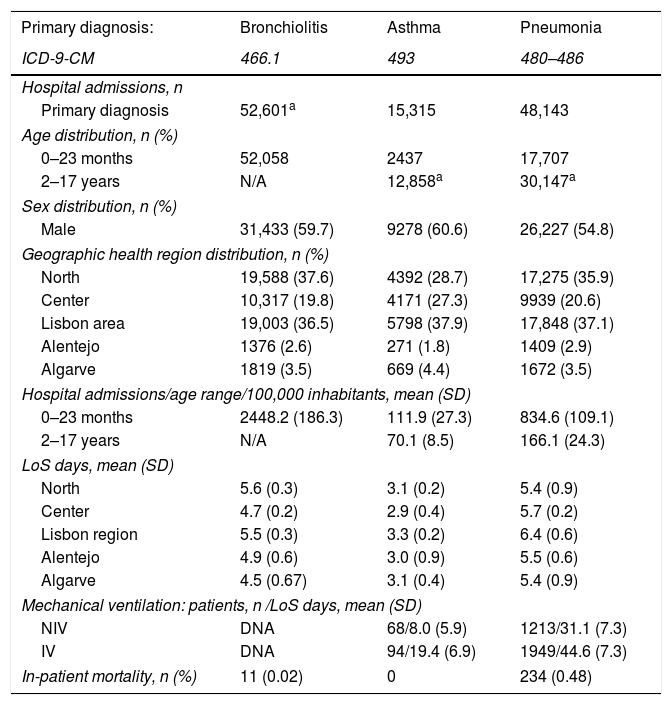
Demographic features and patterns of regional distribution are summarized in Table 1.
Demographic characteristics of study population, number and regional distribution of cases, length of stay (LoS), mechanical ventilation and in-patient mortality in bronchiolitis, asthma and pneumonia, 2002–2012.
| Primary diagnosis: | Bronchiolitis | Asthma | Pneumonia |
|---|---|---|---|
| ICD-9-CM | 466.1 | 493 | 480–486 |
| Hospital admissions, n | |||
| Primary diagnosis | 52,601a | 15,315 | 48,143 |
| Age distribution, n (%) | |||
| 0–23 months | 52,058 | 2437 | 17,707 |
| 2–17 years | N/A | 12,858a | 30,147a |
| Sex distribution, n (%) | |||
| Male | 31,433 (59.7) | 9278 (60.6) | 26,227 (54.8) |
| Geographic health region distribution, n (%) | |||
| North | 19,588 (37.6) | 4392 (28.7) | 17,275 (35.9) |
| Center | 10,317 (19.8) | 4171 (27.3) | 9939 (20.6) |
| Lisbon area | 19,003 (36.5) | 5798 (37.9) | 17,848 (37.1) |
| Alentejo | 1376 (2.6) | 271 (1.8) | 1409 (2.9) |
| Algarve | 1819 (3.5) | 669 (4.4) | 1672 (3.5) |
| Hospital admissions/age range/100,000 inhabitants, mean (SD) | |||
| 0–23 months | 2448.2 (186.3) | 111.9 (27.3) | 834.6 (109.1) |
| 2–17 years | N/A | 70.1 (8.5) | 166.1 (24.3) |
| LoS days, mean (SD) | |||
| North | 5.6 (0.3) | 3.1 (0.2) | 5.4 (0.9) |
| Center | 4.7 (0.2) | 2.9 (0.4) | 5.7 (0.2) |
| Lisbon region | 5.5 (0.3) | 3.3 (0.2) | 6.4 (0.6) |
| Alentejo | 4.9 (0.6) | 3.0 (0.9) | 5.5 (0.6) |
| Algarve | 4.5 (0.67) | 3.1 (0.4) | 5.4 (0.9) |
| Mechanical ventilation: patients, n /LoS days, mean (SD) | |||
| NIV | DNA | 68/8.0 (5.9) | 1213/31.1 (7.3) |
| IV | DNA | 94/19.4 (6.9) | 1949/44.6 (7.3) |
| In-patient mortality, n (%) | 11 (0.02) | 0 | 234 (0.48) |
DNA: data not available; LoS: length of stay; n: total number; N/A: not applicable based on disease definition; NIV: non-invasive ventilation; IV: invasive ventilation; SD: standard deviation.
A slight predominance of male sex is shown and the first 2 years of age represent 61.3% of all admissions (all cases of bronchiolitis, 15.9% and 37.0% of cases for asthma and pneumonia).
LoS trend analysis revealed a statistically significant decrease for the three conditions (p=0.000 for bronchiolitis and asthma and p=0.001 for pneumonia), with mean (SD) LoS of 5.4 (0.17), 3.1 (0.18) and 5.9 (0.45) days for bronchiolitis, asthma and pneumonia respectively.
Hospital readmissions were only available for asthma and pneumonia during 2011 and 2012, which were 8.2% and 8.9% and 8.2% and 9.4% respectively.
For asthma, mechanical ventilation was documented in 162 patients [NIV in 68 and IV in 94] representing 0.44% and 0.61% of asthma hospital admissions and mean (SD) LoS for mechanical ventilated patients was 8.0 (5.92) and 19.4 (6.87) days, for NIV and IV. For pneumonia, mechanical ventilation was reported in 3162 patients, [NIV in 1213 and IV in 1949 patients] representing 2.52% and 4.05% of pneumonia hospital admissions, and a mean (SD) LoS for mechanical ventilated patients of 31.1 (7.29) and 44.6 (7.27) days, for NIV and IV patients.
Complete data on mortality was not disclosed due to confidentially, but 11 deaths were reported for bronchiolitis, dispersed throughout the study period and between regions; no inhospital mortality for acute asthma was disclosed and for pneumonia a mortality rate of 0.48% was registered.
In conclusion, a significant hospital admission rate decline for pneumonia was noticed, probably following the introduction of anti-pneumococcal vaccines as reported here for the first time from administrative data in Portugal in the pediatric age group, which parallels internationally reported data.8 Asthma admissions slightly decreased over the period analyzed, which was already reported by Santos N et al. for an almost similar period,9 both globally and under 2 years of age. We recognize that there is clinical overlapping between the three entities studied particularly in children under 2 years-old.3 Our results are comparable with those reported in another audit where around 1/3 of pediatric asthma hospitalizations occurred in children under 2 years of age.10
A slight increase in hospital admission rate for bronchiolitis was noticed. A recently published study showed similar results.11 Although data on readmissions and ventilation was not available in our study, Mendes-da-Silva et al showed an increase in mechanical ventilation mostly because of NIV use not explained by severity.11 Children under 2-years of age represented the highest burden for all the acute diseases in analysis, including asthma and pneumonia [incidence increase 1,6 and 5-fold].
For all diseases and age groups, male sex predominates. In all groups, a decrease in LoS was noticed, but the use of mechanical ventilation increased. As such, our data provide a benchmark, which may contribute to optimize health resources.
Author contributionsAll listed authors participated in the study conception, in the data acquisition/analysis and in the writing of the article.
Funding sourceThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestThe authors have no conflicts of interest to declare.