Flexible bronchoscopy is a key diagnostic and therapeutic tool. New endoscopes and technologically advanced navigational modalities have been recently introduced on the market and in clinical practice, mainly for the diagnosis of mediastinal lymph adenopathies and peripheral lung nodules. Bronchoscopic sampling tools have not changed significantly in the last three decades, with the sole exception of cryobiopsy.
We carried out a non-systematic, narrative literature review aimed at summarizing the scientific evidence on the main indications/contraindications, diagnostic yield, and safety of the available bronchoscopic sampling techniques.
Performance of bronchoalveolar lavage, bronchial washing, brushing, forceps biopsy, cryobiopsy and needle aspiration techniques are described, focusing on indications and diagnostic accuracy in the work-up of endobronchial lesions, peripheral pulmonary abnormalities, interstitial lung diseases, and/or hilar-mediastinal lymph adenopathies. Main factors affecting the diagnostic yield and the navigational methods are evaluated.
Preliminary data on the utility of the newest sampling techniques (i.e., new needles, triple cytology needle brush, core biopsy system, and cautery-assisted transbronchial forceps biopsy) are shown.
Take Home MessageA deep knowledge of bronchoscopic sampling techniques is crucial in the era of technological bronchoscopy for an optimal management of respiratory diseases.
Flexible bronchoscopy represents an essential diagnostic and therapeutic tool when managing patients with complicated and difficult-to-treat respiratory diseases.1 After the introduction of the first fiberoptic instruments in 1967, new types of endoscopes were developed: video-bronchoscopes (i.e., endoscopes with a video camera at the distal tip) can significantly improve the quality of the images, ultrathin instruments (i.e., diameter size <3...mm) can explore distal airways beyond segmental bronchi, echo-bronchoscopes can significantly improve the diagnostic accuracy for mediastinal lymph adenopathies.2...4
The widespread use of sensitive computed tomography, magnetic resonance imaging, and positron emission tomography have broadened the clinical indications of bronchoscopy and have provided an accurate guide for endoscopic samplings.3,5,6
Flexible bronchoscopy is usually recommended for the diagnosis and staging of lung cancer, diagnosis of respiratory tract infections (both in immunocompetent and immunocompromised patients) and of interstitial lung diseases. Furthermore, its use is required for patients with hemoptysis, with unexplained cough and stridor/wheezing, and staging of thoracic malignancies.1,3,7...11
Flexible bronchoscopy, performed under conscious sedation and with topical anesthesia, is safe in all age groups, including the elderly, with serious complications and mortality occurring in 1.1% and 0.04% of the cases, respectively.1,3,12,13
Bronchoscopic procedures comprehensively assess endobronchial abnormalities (e.g., airway stenosis, bleeding, secretions, etc.) and frequently are adopted to collect specimens for microbiological and/or pathological exams,1,3 quality and quantity of which is key to increase diagnostic accuracy (e.g., idiopathic pulmonary fibrosis, IPF, and lung cancer).14,15
New endoscopes and technologically advanced navigational modalities have been recently introduced, mostly for the diagnosis of mediastinal lymph adenopathies and peripheral lung nodules.16
With the sole exception of cryobiopsy, bronchoscopic sampling tools have not changed significantly in the last three decades.16
The aim of this review is to summarize the scientific evidence on the main indications/contraindications, diagnostic yield, and safety of the available bronchoscopic sampling techniques.
MethodsWe carried out a non-systematic, narrative literature review. The search engine Pubmed was used to retrieve the most relevant articles on the above-mentioned topic. The search was conducted without any time restrictions. Only epidemiological studies performed on adult human beings and written in English were selected. The following keywords were combined to address our research question: bronchoscopy; sampling methods; bronchoscopic tools; needle aspiration; biopsy techniques; bronchoalveolar lavage; bronchial washing.
ResultsBronchoalveolar lavageBronchoalveolar lavage (BAL) is a safe and minimally invasive bronchoscopic sampling method recommended for patients with several lung medical conditions (e.g., immune-mediated, inflammatory, and infectious diseases). It can provide specimens for cytological and microbiological exams (Table 1).17
Summary of bronchoscopic sampling techniques and methods of guidance according to the target lesion.
| Endobronchial lesions | Peripheral pulmonary lesions | Hilar and mediastinal lymph adenopathies | Interstitial lung diseases |
|---|---|---|---|
| BW | BAL | TBNA | BAL |
| EBB | TBB (fluoroscopy or newer navigational modalities-guided) | EBUS-TBNA | TBB (fluoroscopy-guided) |
| EBNA | TBNA (fluoroscopy or newer navigational modalities-guided) | EUS-B-FNA | Cryobiopsy (fluoroscopy, rEBUS-, CLM- and Cone Beam CT-guided) |
| Brushing | Brushing (fluoroscopy or newer navigational modalities-guided) | EBUS-ca-TBFB | |
| Cryobiopsy | Criobiopsy (EMN and rEBUS-guided) | ||
| Triple brush (EMN and Cone Beam-guided) | |||
| GenCut Core Biopsy (EMN and Cone Beam-guided) |
BW: bronchial washing; BAL: bronchoalveolar lavage; CLM: confocal laser microscopy; EBB: endobronchial forceps biopsy; EBNA: endobronchial needle aspiration; TBB: transbronchial biopsy; TBNA: conventional transbronchial needle aspiration; rEBUS: radial probes endobronchial ultrasound; EBUS-TBNA: endobronchial ultrasound transbronchial needle aspiration; EUS-B-FNA: endoscopic ultrasound (with bronchoscope) fine needle aspiration; EBUS-ca-TBFB: endobronchial ultrasound guided cautery-assisted transbronchial forceps biopsy.
It is contraindicated in patients with cardiopulmonary instability and/or with a severe haemorrhagic diathesis and It could rarely exacerbate interstitial lung diseases (ILD).18,19 Transient hypoxemia and low-grade fever within the first 24...h after lavage are the most frequent adverse events.1,6
BAL is performed after the assessment of the tracheobronchial tree and before any biopsies.15,17,20
The bronchoscope should advance as far as possible to the complete occlusion of the bronchial lumen of a third or fourth bronchial subsegment, in a wedged position. Room temperature sterile saline is employed: 100...300...ml, divided into three to five aliquots, are introduced through the suction channel of the bronchoscope. A volume higher than 5% of the original one (ideally >30%) is collected using a negative suction pressure (<100...mm Hg) avoiding airway collapse.
Interstitial lung diseasesBAL is helpful in patients with suspected ILD21 both for the diagnosis itself and the differential ascertainment. A high resolution chest CT should be performed within 6 weeks for the optimal identification of the sampling anatomical area.17
A differential cellular count for the identification of the inflammatory pattern (i.e., lymphocytic, neutrophilic, eosinophilic, and mast cellular), may be useful in the differential diagnosis of interstitial lung diseases. A minimal volume of 5...mL of a pooled BAL sample is needed for BAL cellular analysis (the optimal volume is 10...20...ml).
Bloody fluid, with increasing colour intensity in sequential aliquots, can suggest a diffuse alveolar haemorrhage22 (microscopic diagnosis supported by hemosiderin-laden macrophages).17 Cloudy (i.e., milky or light brown-beige colour) fluid with flocculent material settling by gravity within 15...20...min and PAS-positive amorphous debris suggests a pulmonary alveolar proteinosis (PAP).
An increased number of CD-1a cells (>5% of BAL cells) strongly suggests pulmonary Langerhans cell histiocytosis.23
BAL cellular pattern may help discriminate IPF from eosinophilic pneumonia (eosinophilia >25%), sarcoidosis (high proportion of lymphocytes and CD4/CD8 ratio), and infections.15
In patients with a fibrotic interstitial lung disease BAL lymphocytosis of at least 30% may suggest nonspecific interstitial pneumonia and extrinsic allergic alveolitis.24
A recent retrospective study that aimed to study the role of bronchoscopy in acute respiratory failure related to ILD, failed to demonstrate a different management and mortality between patients with positive and negative BAL findings.25
Peripheral pulmonary lesionsBAL should be used for patients with slowly resolving/non-resolving pneumonia (sensitivity >70%).1,26 BAL can play a key role in the TB diagnosis for sputum smear-negative patients or in those in whom sputum cannot be collected.27 BAL diagnosis of pulmonary TB relies on smear microscopy (sensitivity range: 4.7...58.0%), nucleic acid amplification techniques (sensitivity: 31.3...83.8%; specificity: 92.4...98.2%), and culture (highest diagnostic accuracy).27
BAL can help rule out opportunistic infections in immunocompromised hosts,1 with a sensitivity up to 98% for Pneumocistis jiroveci. Sensitivity of smear microscopy for TB disease in HIV-positives ranges from 10 to 30%, increasing to 85.7% and 52...95% when nucleic acid amplification techniques and culture are adopted, respectively.27...29 In immunocompromised hosts with invasive aspergillosis, BAL can help detect fungal hyphae (34...64% of the cases) and galactomannan antigen (sensitivity and specificity of respectively 79...90% and 84...94%), and can increase the rate of culture positivity (23...85%).1,30,31
BAL shows a low accuracy in the diagnosis of peripheral lung malignancies (mean sensitivity 43%), whereas lymphangitic carcinomatosis and pulmonary lymphoma may be diagnosed using BAL samples.6,32,34
Bronchial washingBronchial washing (BW) consists of instillation and subsequent aspiration of saline mixed up with bronchial secretions, into a specific bronchial trap. It may be useful to assess the microbiology of central airways secretions.6 In the diagnosis of TB, BW smear microscopy and Xpert MTB/RIF show a sensitivity of 25...41% and 80...92.3% and a specificity of 87.7...95.8% and 81.6...98.6%, respectively.27,33...35
A limited diagnostic support was found for endobronchial lung cancers (mean sensitivity: 47%). (Table 1).
The diagnostic yield of bronchoscopy when bioptic techniques (i.e., endobronchial needle aspiration and forceps biopsy) are used is not affected by BW.36
Needle aspirationNeedle aspiration, which is the most versatile bronchoscopic sampling technique, is recommended for the diagnosis of endobronchial and peripheral lesions and in case of hilar/mediastinal lymph adenopathies (Table 1).37,38
A thin (25...19 gauge), retractable needle attached to the distal tip of a flexible catheter is inserted into the working channel of the endoscope and is pushed into the target lesion, while the catheter is moved back and forth for few seconds at its proximal end. The vacuum inside the syringe causes tissue to be suctioned into the needle.37,38 The needle may be inserted in an endobronchial lesion under direct endoscopic vision and into a hilar/mediastinal lymph node, through the tracheobronchial wall, with or without endoscopic ultrasound guidance. Fluoroscopy and/or other navigational techniques are necessary to reach peripheral lung abnormalities.38
The collected specimen may be smeared on a glass slide or directly placed in formalin solution (technique named formalin-fixed, paraffin-embedded cell-block). Rapid on-site evaluation (ROSE) of the aspirates may be performed, allowing bronchoscopists to stop sampling when sufficient material has been harvested for diagnosis and molecular analysis, thus potentially avoiding useless samplings and reducing the complications of bronchoscopy.36,37
Endobronchial lesionsEndobronchial needle aspiration (EBNA) is a useful and safe technique adopted for the diagnosis of endobronchial lesions (mainly lung neoplasms).
It has a mean sensitivity of 56%, with a rate of complications (mostly minor bleedings) <1%.36,39,40 It significantly increases the accuracy of bronchoscopy in the diagnosis of central lung cancers when combined with endobronchial forceps biopsy. EBNA is particularly helpful in sampling submucosal/peribronchial (i.e., growing in deeper layers of the airways) and necrotic lesions. Needle can penetrate the mucosa and can sample neoplasms spreading in the deeper layers.36
In the diagnosis of endobronchial tuberculosis, Altin et al. reported a lower sensitivity of EBNA than forceps biopsy in the detection of granulomas (19% vs 84%, respectively).27,41
Peripheral pulmonary lesionsTransbronchial needle aspiration with the guidance of fluoroscopy has been adopted to sample peripheral lung lesions (both nodules and masses) since 1984 (Fig. 1B).42 A recent systematic review and meta-analysis showed a diagnostic yield of 53% and a rate of complications <9%, with pneumothorax and bleeding being the most frequent events.43 Several clinical and procedural variables may affect its accuracy: CT bronchus sign, an underlying malignant process, diameter of the lesions >3...cm, and ROSE employment are the most important predictive factors of a positive aspirate (Table 2). Notably, data on comparison between TBNA and transbronchial forceps biopsy (TBB) in studies where both procedures were performed in the same patients showed a significant diagnostic advantage when TBNA is performed (diagnostic yield: 60% vs. 45%, respectively), although studies have shown that TBNA is still a underused sampling technique.43,44
Recently, new navigational methods, which may be coupled with fluoroscopy, have been adopted to sample peripheral lesions. TBNA guided by electromagnetic navigation bronchoscopy (EMN) showed a diagnostic yield of 46.3%, while needle aspiration guided by radial probes endobronchial ultrasounds (rEBUS) of 49.5...62.5%.44,45 When added to TBB, rEBUS-TBNA significantly increases the accuracy of bronchoscopy in the diagnosis of peripheral lesions.45
Hilar and mediastinal lymph adenopathiesConventional transbronchial needle aspiration (i.e., not guided by ultrasounds) was introduced by Wang in 1984.42
American College of Chest Physician (ACCP) guidelines showed a sensitivity of 78% in the diagnosis and staging of non-small cell lung cancer, with a complication rate of 0.3%.46,47 It was also used for the diagnosis of sarcoidosis stage I and II and mediastinal tuberculosis (sensitivity of 72...79% and 65...100%, respectively %).27,48...50
Currently, cTBNA has been replaced by endobronchial ultrasound (EBUS)-guided TBNA: it includes an echobronchoscope (i.e., a bronchoscope with a convex probe at the distal end) and allows a real-time visualization of the lymph nodes and mediastinal vessels. Unlike cTBNA, EBUS-TBNA can diagnose lymph adenopathies sized <1...cm and lymph node stations without endobronchial landmarks.6,47 EBUS-TBNA shows a higher sensitivity and negative predictive value (89% and 91%, respectively) than conventional technique in the diagnosis and staging of NSCLC.39,47 Its sensitivity in the diagnosis of sarcoidosis and tuberculous lymph adenopathies is 79...84%51,52 and 87%, respectively. Both conventional and ultrasound-guided techniques increase the diagnostic accuracy of bronchoscopy when combined with other sampling techniques (bronchial and transbronchial forceps biopsy and BAL).51,52
Recently, a new needle aspiration technique, named endoscopic ultrasound (with bronchoscope) fine needle aspiration (EUS-B-FNA) has been proved to be effective53: an ultrasound guided needle aspiration of mediastinal lymph adenopathies is performed with an echobronchoscope introduced in the esophagu,.53 Transbronchial and transesophageal needle sampling can be performed with the same instrument, in the same endoscopic session, and by the same operator (i.e., a trained pulmonologist), thus maximizing time and reducing costs. The transesophageal approach can be also used to sample nodes within reach of EBUS, when the clinical conditions contraindicate the transbronchial route (e.g., respiratory failure, cough, etc.).54,55
The combined approach increases the accuracy of endosonography and is now recommended by international guidelines.56
EUS-B-FNA may safely diagnose extra-thoracic targets, such as abdominal lymph nodes, liver and left adrenal glands metastatic lesions.57 Both EBUS-TBNA and EUS-B-FNA may diagnose lung parenchymal lesions adjacent to the central airways and the esophagus.58,59
Needle size does not significantly affects the diagnostic yield.60
Several studies demonstrated the suitability of ultrasound-guided needle aspiration samples for molecular analysis in advanced NSCLC, on both cytology smears and cell-block preparations.61...63
Complications of endosonographic needle aspiration procedures are rare (serious adverse events rate of 0.14%).64
Forceps biopsyForceps has been adopted to collect lung tissue samples through the bronchoscope since the initial implementation of bronchial endoscopy (Table 1).65
Endobronchial lesionsEndobronchial biopsy (EBB) is recommended for the diagnosis of visible endobronchial lesions39: forceps should be opened outside the distal end of the operating channel and pushed against the lesion providing the right orientation to the instrument, according to the localization of the target site. The tip of the forceps is then closed, pulled out of the operating channel of the bronchoscope and the specimen is then placed in formalin solution.66 The different characteristics of the forceps (serrated or smooth edge, fenestrated or unfenestrated cups, needle between the cups) make it potentially suitable for specific settings/lesions. However, the diagnostic yield of various forceps biopsy types was not statistically different.38
EBB is usually employed for suspected bronchogenic cancer with a sensitivity of 74%39: ...3 biopsies are recommended for diagnosis, although at least 6 biopsies can provide sufficient tissue for immunohistochemical and molecular testing.39,67 Several studies36,68,69 demonstrated that the combination of EBB and endobronchial needle aspiration can achieve the best diagnostic performance.
EBB, when combined with transbronchial biopsy, can increase the sensitivity of bronchoscopy by 10...20% in the diagnosis of sarcoidosis: sampling should be performed where the mucosa is abnormal and in the first and second carina if the mucosa seems normal (4...6 endobronchial biopsies); 30% with normal mucosa may have positive EBB.70...72
Forceps biopsy showed a sensitivity of 72.2...100.0% in the detection of TB granulomas (endobronchial TB), and may be useful in ruling out malignancies.27,41,73
The most frequent complication is minor bleeding, which can resolve spontaneously in the majority of the cases or can be treated with ice-cold saline or vasoconstrictive agents (e.g., epinephrine). On this basis, caution may be warranted when sampling is performed for vascularized lesions (i.e., carcinoids).74,75
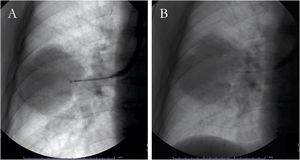
Peripheral lung lesionsA transbronchial biopsy is performed when the lesion cannot be directly assessed with the bronchoscope: it is wedged in the bronchus pertaining to the anatomical site of the lesion, and the closed forceps are pushed in the peripheral area of the lung, opened at 5...6...mm from the lesion and then closed to collect sample (Fig. 1A).6 Fluoroscopy guidance can improve the sensitivity in case of peripheral focal and diffuse cancer lesions.6,76,77 Observational studies have demonstrated that navigational methods (i.e., electromagnetic navigation bronchoscopy, radial probes ultrasounds, virtual bronchoscopy) and/or ultrathin instruments may increase the diagnostic yield of conventional, fluoroscopy-guided technique (77...84%).44,78...80
The diameter of the lesion affects the accuracy of the technique: the sensitivity is <35% in case of nodules sized <2...cm.39 Moreover, sensitivity is 24% performing only a single biopsy and 70% when six biopsies are collected.81,82 The presence of the CT-bronchus sign is associated with a higher yield (Table 2).83,84
TBB may increase the sensitivity of BAL for the diagnosis of Pneumocystis jirovecii pneumonia, including non...HIV patients.85 In sputum smear negative or sputum scarce TB patients with peripheral lung lesions, TBB86...88 may help detect cytological and histological TB findings (i.e., necrotizing granulomatous inflammation), ruling out malignancies.89
Finally, TBB is a safe and repeatable procedure monitoring early signs of graft rejection in lung transplant recipients.90
Mild bleeding and pneumothorax are the most frequent complications. Pneumothorax can occur in 1...5% of the cases; its variability can depend on the use of mechanical ventilation, surrounding emphysema, lesion near to the pleura, and poor expertise of the healthcare worker.6
Bleeding can be a risk in patients with coagulopathy disorders and/or taking anticoagulant and anti-platelet drugs.6
Interstitial lung diseasesSensitivity of TBB in diffuse lung disease varies widely.91 The main limitations are the small size of the sample and the difficult preservation of the tissue integrity, for which a surgical biopsy or a cryobiopsy may be more suitable.92 Exceptions are conditions involving the centrilobular region (both at the terminal and respiratory bronchioles or along the lymphatic distribution, such as sarcoidosis, hypersensitivity pneumonitis, organizing pneumonia, eosinophilic pneumonias, and lymphangitic spread of malignancy). Sensitivity ranges from 55% in stage I to 80% in stage III93 in sarcoidosis. Higher yield is found when biopsies are performed in >1 lobe and in the area of the most affected tissue in stage II/III disease.94
Guidelines on Idiopathic Pulmonary Fibrosis (IPF) do not recommend for or against TBB when the HRCT suggest a probable UIP pattern. In this context, TBB could be only clinically helpful to exclude mimickers.15,95
BrushingEndobronchial lesions and peripheral lung abnormalitiesBrushing consists of a rigid central wire surrounded by brushes of various sizes and shapes. A brush inserted through the operating channel performs both a back and forth and a spinning movement on the surface of the mucosa. Cytological material may be smeared on glass slides or placed in formalin solutions. The diameter or the length of the brush does not affect the diagnostic yield6 (mean sensitivity in the diagnosis of endobronchial malignancy: 61%).39 Addition of bronchial brushing to forceps biopsy and needle aspiration does not increase the sensitivity of bronchoscopy.36,40,69
It showed a diagnostic yield of 47...54% in the diagnosis of peripheral lesions,39 which is usually lower than that reported for TBB and TBNA, even if guided by novel methods of navigation (Table 1).39,44,80
Quantitative cultures of protected brushing (i.e., a double-lumen catheter brush system with a distal occluding plug to prevent secretions from entering the catheter during passage through the bronchoscope channel) can be performed to diagnose pneumonia in critically ill patients, (mean sensitivity: 89%).96,97
Minor bleeding is the most likely incidental complication.
CryobiopsyCryoprobe is a therapeutic and diagnostic tool traditionally adopted for endobronchial tumour ablation and airway recanalization or by removal of blood clots and foreign bodies.98...100
Only recently several studies proved its accuracy as endobronchial and transbronchial biopsy technique (Table 2).101
Its activity is based on the principle of the Joule-Thomson effect, wherein the adiabatic expansion of a compressed gas leads to a rapid cooling. The cooled tip of the cryoprobe, inserted in the working channel of the bronchoscope, adheres to the tissue due to crystallization of water molecules at the interface. After a few seconds of cooling, the probe is extracted with a specimen, which is placed in formalin.
Cryobiopsy may be used with flexible bronchoscopes with local anaesthesia, deep sedation and/or general anaesthesia, with laryngeal mask or in patient intubated with orotracheal tube or rigid tracheoscope (during spontaneous breathing or mechanical ventilation). Intubation with deep sedation or general anaesthesia and administration of a bronchial blocker are recommended to prevent severe bleedings in the diagnostic work-up of ILD.102
Endobronchial lesionsHetzel et al. demonstrated the higher efficacy of cryobiopsy in the diagnosis of endobronchial malignant lesions when compared with conventional forceps: it can collect larger specimens without disrupting the morphological structure. Cryoprobes increase the diagnostic yield of bronchoscopy (up to 95%), without a higher rate of bleeding.98 Several studies have confirmed these findings,103 including the safety in the diagnosis of carcinoid tumours.104
Peripheral lung lesionsSchumann et al. evaluated the accuracy in the diagnosis of peripheral lesions with the guidance of rEBUS: the diagnostic yield of 74.2% was not significantly higher in comparison with that of EBUS-guided forceps biopsy (61.3%); however, samples were significantly larger than those collected by TBB.105
Other studies showed a diagnostic yield of 69...85% when guided by ultrasounds or EMN, and confirmed the advantage of larger samples and a better preserved architecture, thus improving the specimen quality for the molecular diagnosis.106...110
Mild bleeding and pneumothorax were the most common incidental adverse events.
Interstitial lung diseasesTransbronchial lung cryobiopsy (TBLC) is a minimally invasive alternative to surgical lung biopsy (SLB), which is the gold standard in the histopathological diagnosis of many ILD. Conventional forceps biopsies are inadequate in diseases characterized by a heterogeneous histological pattern and in those with histological abnormalities located at the periphery of the secondary lobule (e.g., usual interstitial pneumonia, UIP).102
Larger biopsy size and lack of crush artifact make cryobiopsy more suitable for the diagnosis of diffuse lung diseases if compared with conventional forceps biopsy.111
IPF Guidelines recommend cryobiopsy only in experienced centers, when HRCT pattern is probable UIP, indeterminate for UIP or suggesting an alternative diagnosis.15
Tomassetti et al., who recruited 117 patients with fibrotic ILD needing a pathological diagnosis, demonstrated that the addition of TBLC was associated to an increased diagnostic confidence in the multidisciplinary diagnosis of idiopathic pulmonary fibrosis, similar to that provided by SLB.112
Samples should be taken under fluoroscopic guidance in the distal part of the lung parenchyma, avoiding high density fibrotic areas. Biopsy should be performed at a distance >1...cm from the pleura to reduce the occurrence of pneumothorax.113
As suggested by Ravaglia et al., collection of ...2 samples from two different segments in the same lobe or from different lobes in case of inter-lobar radiographic heterogeneity is recommended to increase the diagnostic yield.102,113...115
A systematic review and meta-analysis showed a pooled diagnostic yield of 79%.116
Two studies evaluated the accuracy of cryobiopsy in comparison with surgical biopsy: Romagnoli et al. found a poor concordance between TBLC and SLB (concordant coefficient (k): 0.22, percentage agreement: 38%),117 whereas a multicentre, prospective study , found a histopathological agreement of 70.8% (weighted k: 0.70) and a final diagnostic agreement of 76.9% (k: 0.62).118
The frequency of pneumothorax and moderate/severe bleeding is 9.5% and 1.1...8.7%, respectively.113
Guidelines suggest the use of fluoroscopy, of a bronchial blocker, and a small (i.e., 1.9...mm) cryoprobe to reduce the complication rate.113
One prospective study reported on the utility of a radial EBUS miniprobe to avoid injuries of pulmonary vessels during biopsy.119 Confocal laser microscopy (CLM) is a minimally invasive endoscopic technique that provides real time in vivo microscopic imaging of the distal lung through a thin probe advanced through the working channel of the bronchoscope until the alveolar area. Preliminary data demonstrated that CLM may be a useful guidance tool for transbronchial cryobiopsies. It helps to distinguish fibrotic vs. not fibrotic areas and to avoid the pleura thereby reducing the risk of pneumothorax.120
Likewise, Cone beam CT-guided TBLC, which evaluates the probe-to-pleura relationship based on 3D CT scans, has a safe profile, with low risk of pneumothorax and moderate/severe bleeding.121
The main contraindications are bleeding diathesis, use of anticoagulants, thienopyridines, antiplatelet drugs, and thrombocytopenia (<50........109/L), pulmonary hypertension, and severe respiratory functional impairment.102
New toolsNew flexible needles of different size have recently been introducedonto the market for endosonographic sampling of hilar/mediastinal lymph nodes. New needles may provide more visibility on ultrasound images while the needle penetrates the lymph node, more flexibility to target paratracheal and hilar stations, and a larger amount of tissue for histopathological analysis.122
New tools for diagnosis of endobronchial and peripheral lesions can be directly inserted into the working channel of the endoscope or passed into a guide sheath to reach peripheral lung abnormalities. Triple cytology needle brush may trap larger tissue samples. A new core biopsy system (i.e. GenCut core biopsy system) consists of a flexible tool with a rounded, blunt tip, a port and blade along the distal and lateral sides with a hollow core: suction is applied follow by rotation and agitation to collect intact tissue.44,80
Cautery-assisted transbronchial forceps biopsy (ca-TBFB) is a new sampling technique which collects larger amount of tissue from mediastinal lymph nodes: a target lymph node is identified with EBUS while an electrocautery knife is advanced through the working channel of the endoscope toward the airway wall. Then, cautery is applied and the knife inserted through the tracheal/bronchial wall defect (under EBUS real-time guidance), created by the cautery edge. After the penetration, the knife is withdrawn and a spiked forceps advanced into the lymph node to collect the sample.123,124
Two observational studies showed a higher sensitivity in comparison with that of EBUS-TBNA in the diagnosis of sarcoidosis and lymphoma.123,124
Another study proved an increased sensitivity of EBUS forceps biopsy in patients with mediastinal lymph nodes in whom ROSE of EBUS-TBNA failed to show positive findings.125