Pulmonary hypoplasia is a rare congenital abnormality in which normal pulmonary tissues are present but underdeveloped.1 It is usually diagnosed during childhood, and there are very few patients who survive beyond 18 years,2 because they generally die due to intercurrent infections and other congenital abnormalities. Because of this, there are few patients who reach adult age.3 A review of the literature shows that the first case of an adult patient was reported in the year 1964.4
We present a case of a 64-year-old woman, previously hypertensive, obese (BMI 35) and ex-smoker (30 pack-years). She had been reporting recurrent respiratory infections since childhood, which were treated with antibiotics by her family doctor. She was admitted to hospital with chronic non-productive cough and dyspnea of two years of evolution which increased until it became dyspnea on minimal exertion in the previous month. The clinical picture was not accompanied by chest pain, orthopnea, hemoptysis or weight loss.
In the physical examination, the patient's vital signs were normal, with an oxygen saturation of 89%. Cardiac auscultation revealed normal heart sounds. Pulmonary examination findings revealed decreased breath sounds in the right lung, without wheezing.
Laboratory tests did not show alterations with negative D-dimer. With regard to gasometry, the patient presented global respiratory failure (pH 7.44, pO2 50mmHg, pCO2 52mmHg, HCO3 35.3mmol/L).
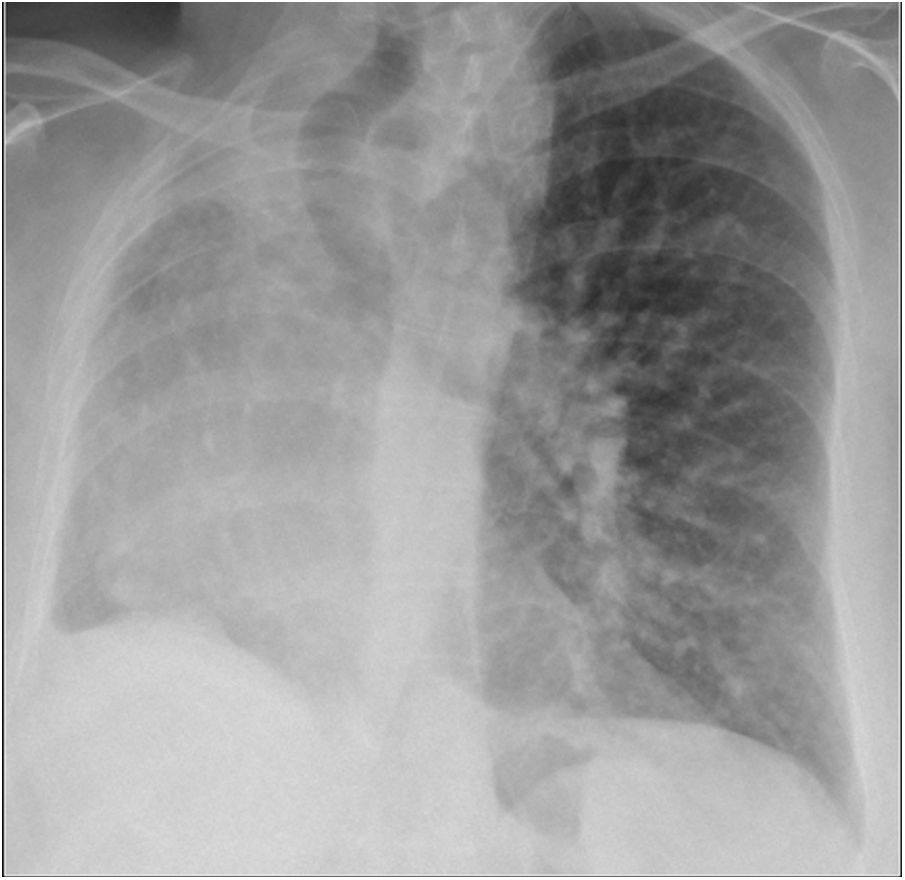
The thoracic X-ray revealed volume loss in right hemithorax, atelectasis of right upper lobe and tracheal deviation to that side, without pleural effusion or other hyperdense areas (Fig. 1).
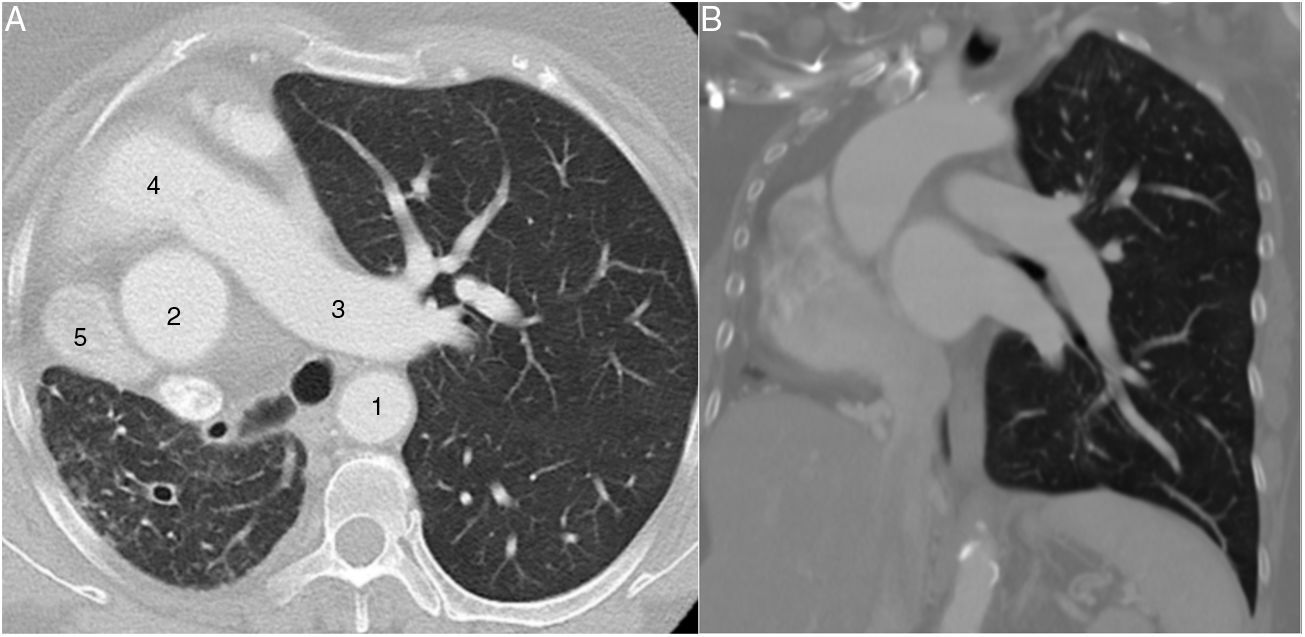
A computerized tomography (CT) was carried out to characterize the radiological findings described and to rule out a pulmonary neoplasm as a first possibility. This test revealed a lack of right pulmonary artery and right pulmonary veins, with hypoplasia of the right lung and displacement of mediastinal structures toward that side. Abundant collateral bronchial and intercostal circulation could be seen on the right side. The hypoplastic lung revealed arterial supply dependent on the abdominal aorta and venous drainage toward the inferior vena cava. On the other hand, there was compensatory hyperinflation of the left lung and hypertrophy of left pulmonary arteries (Fig. 2).
Afterwards, pulmonary function test results were obtained, which were compatible with very severe obstructive ventilatory defect, increased pulmonary resistance and air trapping. The bronchodilator test was negative.
In addition, the echocardiography suggested pulmonary arterial hypertension with mean pulmonary artery pressure of 60–65mmHg without any other alteration.
The patient is currently receiving pulmonary rehabilitation and domiciliary oxygen. Due to persistent daytime hypoventilation (pCO2 ≥45mmHg) caused by multifactorial origin, she is being treated with non-invasive mechanical ventilation, which has improved her basal status and gasometry.
DiscussionSometimes, dyspnea may present as a diagnostic challenge. It is a very unspecific symptom which is present in many conditions, mainly cardiovascular and respiratory diseases.
Generally, the patient diagnosed with pulmonary hypoplasia is asymptomatic,5,6 which means that most of the times the diagnosis is incidental, following a thoracic X-ray in the context of an acute process, as happened with the present patient.
The left lung is more commonly affected,7 and in up to 50% of the cases there is an association with cardiovascular, gastrointestinal, genitourinary, neurological or musculoskeletal malformations.8 In all cases, it is important to rule out any potential association with other diseases such as cystic fibrosis, immunological deficiencies or inborn errors of metabolism.8 In our case, no other malformation or associated disease were found.
Currently, the diagnostic technique of choice is thoracic CT scan,9 because it makes it possible to visualize the rudimentary lung as we described in the clinical picture.
A simple thorax X-ray generally shows opacity and a decrease in the intercostal spaces of the affected hemithorax, herniation of the healthy lung and a mediastinum displaced toward the affected hemithorax. It is not uncommon to find skeletal abnormalities such as kyphoscoliosis. The differential diagnosis must be carried out using entities that reduce the volume and increase the density of the hemithorax: atelectasis, mainly due to pulmonary neoplasm; post-pneumonectomy changes; fibrothorax; and tuberculosis.10
There are other tests that can assist in diagnosis, such as bronchoscopy, pulmonary angiography, bronchography, ventilation–perfusion scintigraphy and magnetic resonance.8
Pulmonary function tests generally show a restrictive ventilatory disorder. In some cases, such as the one in our study, they may also present an obstructive component caused by age, hyperinflation or the presence of recurring infections, stimulated by the production and retention of secretions in the rudimentary pulmonary tissue.7
Pulmonary artery agenesis and hypoplasia is a rare cause of pulmonary hypertension caused by the situation of hyper-flow in the remaining pulmonary artery.11
The most favorable survival rates have been observed in cases of left lung hypoplasia because of the satisfactory compensatory hypertrophy of the larger right lung.12,13
The global treatment of pulmonary hyperplasia is medical care in most cases, with respiratory physiotherapy and intensive treatment of bronchopulmonary infections.7
To sum up, isolated pulmonary hypoplasia in adults is extraordinarily uncommon, as we highlighted in our case. That is the reason why this entity should be included in the differential of a chest radiograph with a contracted hyperlucent hemithorax.
Authors’ contributionVirginia Guevara drafted the manuscript, Soraya Jodra and Marco Lopez managed drafting, Miguel Ángel Hernández collected and retouched the pictures, José María González and Miguel Barrueco supported data collection and all authors revised the manuscript and approved its final version.
Conflicts of interestAll authors declare that there is no conflict of interest regarding the publication of this article.