The Swan-Ganz catheterization provides valuable hemodynamic information but presents current specific indications. Its routine use in critically ill patients and in patients with severe cardiopulmonary disease and high risk of intraoperative hemodynamic compromise undergoing surgery was abandoned due to lack of prognostic improvement and risk of complications.1 However, it remains an important diagnostic procedure in patients with suspected or previous history of pulmonary arterial hypertension (PH).1 Pulmonary artery (PA) injury is a rare but most feared complication with an estimated incidence of 0.031% to 0.05% and a mortality that ranges from 50 to 70 percent.2
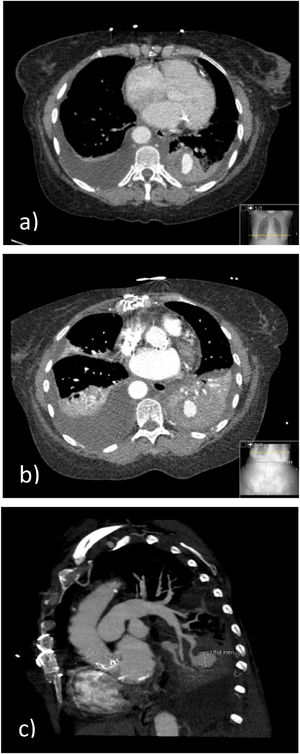
We describe the case of a 67-year-old non-smoker female patient, with a personal history of systemic sclerosis, PH, systemic arterial hypertension, aortic stenosis submitted to biological valve prosthesis placement, epilepsy, and osteoporosis, usually medicated with enalapril, amlodipine, bosentan, pentoxifylline, acetylsalicylic acid, sodium valproate and inhaled fluticasone and salmeterol. The patient was admitted to the ICU due to the development of massive hemoptysis during right cardiac catheterization to measure pulmonary capillary wedge pressure, experiencing cardio-respiratory arrest in asystole treated with advanced life support maneuvers, orotracheal intubation with a large bore single lumen endotracheal tube (ETT), bilateral lung invasive mechanical ventilation and blood transfusion. Bronchoscopy at admission, 48h after the critical episode and on the day of extubation revealed no active bleeding. Chest computed tomography (CT) angiography showed a nodular lesion with contrast enhancement at the level of the posterior segment of the left inferior lobe, suggestive of a pseudoaneurysm with a mural thrombus (Fig. 1A). Given the spontaneous bleeding control after the first episode, and the lack of prompt access to embolic therapy, requiring inter-hospital transportation, priority was given to clinical stabilization and supportive care, with improvement. After extubation, arterial embolization was proposed to prevent recurrence, which the patient refused. A conservative attitude was adopted, according to the patient's wishes, with favorable outcome. Chest CT-angiography on the 7th day (Fig. 1B and 1C) and chest CT, without contrast administration at patient's request, two weeks later, showed PA pseudoaneurysm stability. Six-year follow-up revealed clinical stability with no bleeding recurrence.
(A) Chest CT-angiography at ICU admission. consolidation at the left inferior lobe (LIL) with areas of spontaneous hyperdensity and "ground glass" opacities; Nodular lesion with contrast enhancement, at the posterior segment of the LIL, in continuity with a pulmonary artery tree branch, suggestive of a pseudoaneurysm with a mural thrombus. (B) and (C) Chest CT-angiography (7th day of hospitalization). Pseudoaneurysm arising from the posterior basal branch of the left inferior lobar pulmonary artery; bilateral pleural effusion with passive atelectasis; and consolidation due to hemorrhagic alveolar filling at the LIL.
Hemoptysis due to PA injury during Swan-Ganz catheterization presents high mortality and morbidity rates2,3 PA injury occurs more frequently in women with >60 years old, PH, mitral valve disease, hypothermia, and under anticoagulants.1,2 Right pulmonary arterial circulation involvement predominates, and hemoptysis is the main manifestation which develops on the day of the procedure in half the cases.2 PA injury may result in intrapulmonary hemorrhage, pseudoaneurysm, or re-endothelization.2 Pseudoaneurysms, usually diagnosed on contrast enhanced CT,1 may be manifested by massive life-threatening hemoptysis, but there is a broad spectrum of manifestations with asymptomatic cases and findings from imaging studies. These are at risk of subsequent hemorrhage that can be fatal.1,2,4
The therapeutic approach to this complication involves two main concerns: first, the immediate protection of the airway and, secondly, the prevention of a new bleeding episode originating from the injured PA. Intubation with a large bore ETT is recommended in life-threatening hemoptysis to facilitate blood and thrombus extraction as well as early interventional and diagnostic bronchoscopy, but its passing should not delay intubation.5 In most patients, both lungs are ventilated but single lung or double lumen ventilation can be considered for patients who continue to bleed.5 In single lung ventilation, tidal volumes should be reduced accordingly.5 There is still no consensus on the most effective endobronchial method for preventing asphyxia from airway bleeding.2,5,6,7 However, several authors have suggested that, when performed by experienced professionals, the simultaneous use of a dual lumen ETT and a balloon catheter may offer the best protection, preventing flooding of the contralateral lung and the ipsilateral non-bleeding bronchial segments.2,6 The role of inhaled tranexamic acid in life-threatening hemoptysis needs further investigation.5 In patients with pseudoaneurysms, the favorite treatment option to prevent bleeding recurrence seems to be arterial embolization,1,4 which has shown a high success rate (∼89%).2,3 Complications associated with this procedure include contrast-associated nephrotoxicity, rare erroneous migration of the embolization material to other arterial beds with risk of pulmonary infarction or paraplegia, and pseudoaneurysm recurrence.2,5,7 Other therapeutic procedures include surgical resection and local injection of thrombin. However, there is currently insufficient data on the most appropriate and effective therapeutic strategy.2 The incidence of bleeding recurrence in patients with the development of pseudoaneurysms in whom a conservative "watch and wait" strategy is adopted is of 30-40%, with a mortality rate of 40-70%.2
In the case described, there were several risk factors for the occurrence of this complication: age over 60 years, female gender, and the main diagnosis of PH. Although involvement of the right pulmonary arterial circulation is more frequent, the pseudoaneurysmal lesion was located at the left inferior lobar PA, providing an atypical presentation of this unusual adverse event. This complication, though rare, is potentially fatal and raises questions about the procedures to be followed. Unfortunately, it can occur even to a highly experienced practitioner who had already successfully performed thousands of exams.