The simultaneous occurrence of sarcoidosis and lymphoproliferative disease is a rare but well-established entity called sarcoidosis-lymphoma syndrome. Despite being increasingly recognized, it remains a diagnostic challenge due to clinical and imaging similarities.1 In most cases, sarcoidosis precedes lymphoma, with non-Hodgkin's lymphoma being the most commonly associated type.1,2 In this case report we describe a rare presentation of endobronchial Hodgkin lymphoma in a patient with sarcoidosis-lymphoma syndrome.
A thirty-seven-year-old male, non-smoker, was diagnosed with lymph node, bone and cutaneous sarcoidosis in 2018, initially treated with prednisolone 40mg/day, later tapered to a maintenance dose of 10mg/day; and with Stage IV classic Hodgkin's Lymphoma (HL), in 2019, treated with ABVD (doxorubicin, bleomycin, vinblastine and dacarbazine) and achieving complete remission in 2020. He was asymptomatic to date.
In February 2021 the patient started to complain of dry cough, fever and night sweats. Physical examination was unremarkable. Laboratory investigations revealed worsening microcytic anemia (hemoglobin of 8.0g/dL) and both high erythrocyte sedimentation rate (72mm/h) and C-reactive protein (11mg/dL). Chest radiograph was normal.
18-FDG Positron emission tomography was performed and showed multiple supra and infradiaphragmatic foci with active metabolism (elevated maximum standardized uptake values (SUVmax)) suggesting active lymphoproliferative disease.
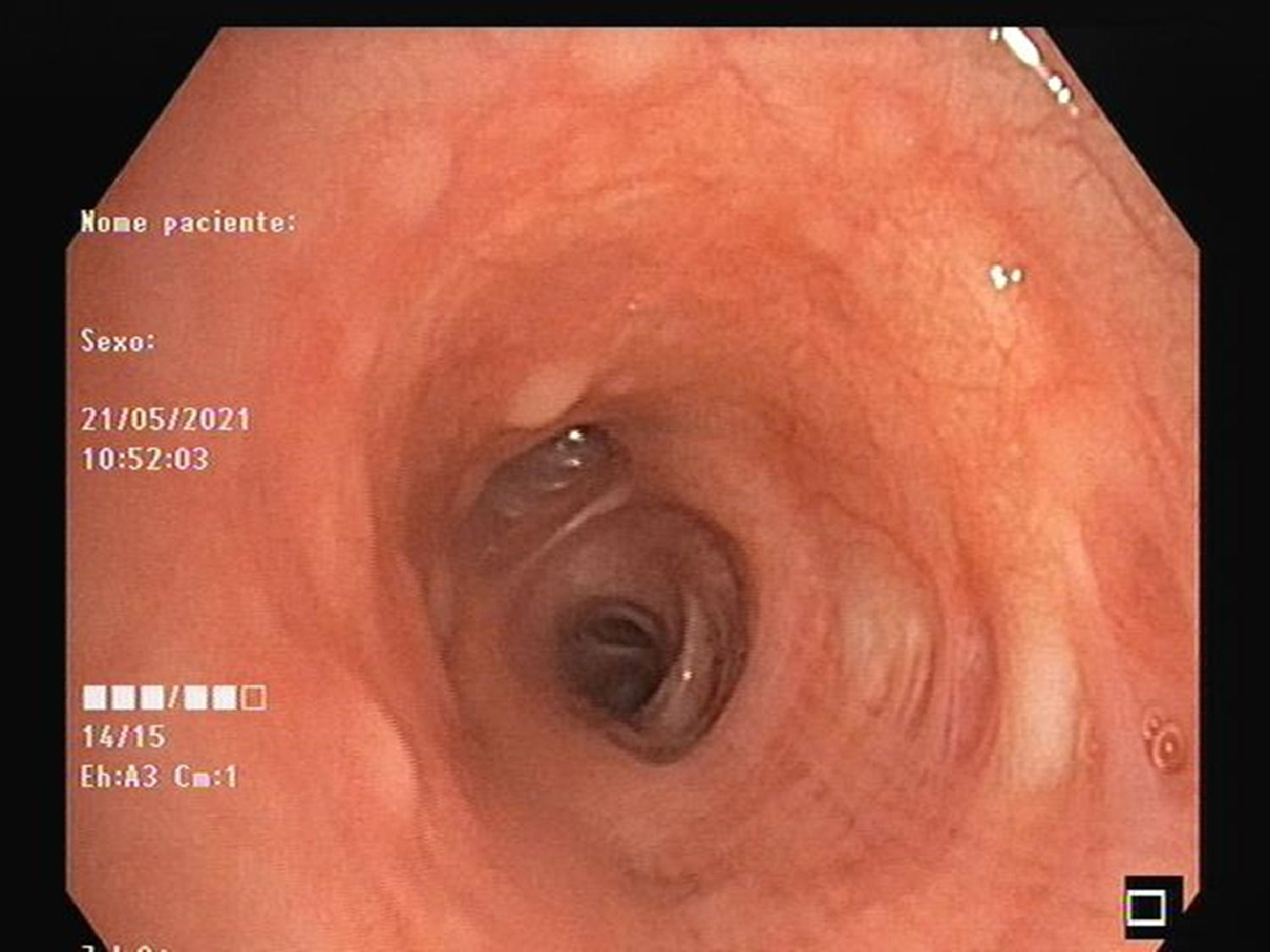
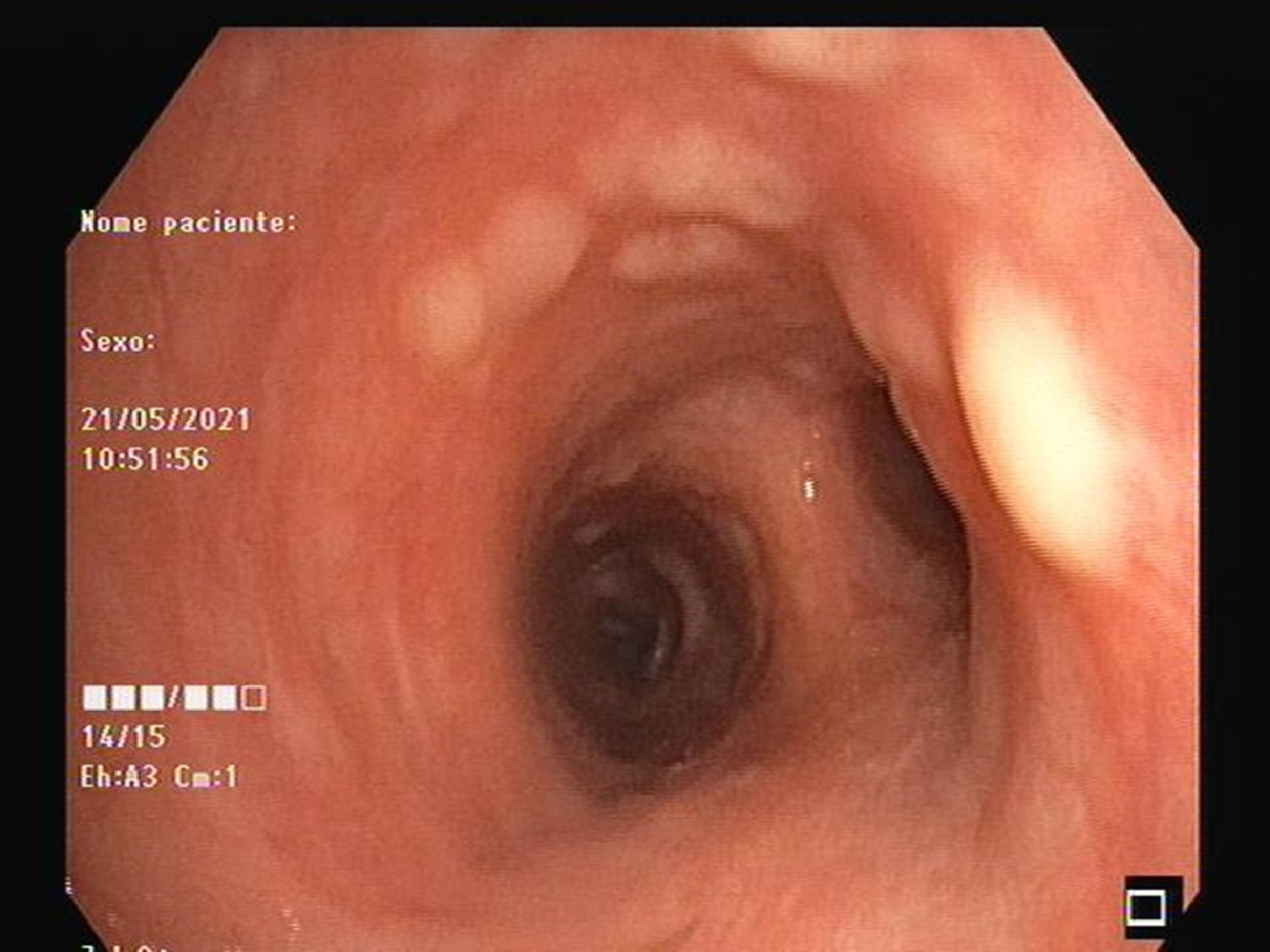
As there was no biopsiable peripheral lymphadenopathy, the patient underwent endobronchial ultrasound (EBUS). The procedure revealed multiple pearly nodular lesions throughout the tracheobronchial tree (Figs. 1 and 2). Bronchial biopsies were performed and mediastinal lymph nodes were punctured at stations 4R and 7 by EBUS-transbronchial needle aspiration.
The anatomopathology of the endobronchial lesions showed HL infiltration and the examination of the lymph nodes showed non-caseating epithelioid granulomas compatible with sarcoidosis. HL relapse was assumed.
The patient was started on chemotherapy treatment with protocol DHAP (dexamethasone, cytarabine, cisplatin and prednisolone), having completed five cycles, with an intermediate response. On reassessment in January 2022, there were signs of disease progression with PET-CT scan showing splenic, multifocal osteomedullary and supra and infra-diaphragmatic lymph nodes involvement. Excisional lymph node biopsy of cervical adenomegaly was performed which, again, confirmed relapse of Hodgkin's Lymphoma and the patient was started on 3rd-line chemotherapy with BV-GVD (brentuximab vedotin + gemcitabine, vinorelbine and doxorubicin) and was proposed for autologous stem cell transplantation.
The sarcoidosis-lymphoma syndrome was first described in 1986 by Brincker.2
Lymphoproliferative disease develops relatively frequently in patients with chronic active sarcoidosis, probably as a consequence of immunological abnormalities observed in this pathology, such as an increased number of T-helper cells in granulomatous tissues, a decreased number of circulating T-helper cells and hyperactivity of the B-cell system. The prolonged immunosuppression therapy, may also have an important role.2,3
The diagnosis of sarcoidosis-lymphoma syndrome is a challenge, since granulomatous inflammation can occur in infections and neoplasms, and is not, in isolation, a diagnosis of sarcoidosis. In our patient, other analytical changes, such as the increase in angiotensin-converting enzyme (ACE) and hypercalcemia, helped the initial diagnosis of sarcoidosis.
The diagnosis of lymphoma was made later by histologic examination of lymph nodes, thus allowing the diagnosis of sarcoidosis-lymphoma syndrome.1,2 A rare aspect of this case is the association between Hodgkin lymphoma and sarcoidosis, which, despite being less common, is also described in the literature.
Another unusual aspect that is highlighted in this clinical case is the recurrence of lymphoma with a rare endobronchial presentation. Pulmonary involvement of HL may occur in up to 40% of cases, but endobronchial involvement is rare, or may be underdiagnosed.4,5 Its frequency varies according to the authors (described in living patients between 1.9-14% of patients with HL). The frequency of endobronchial lymphoma is higher post-mortem.5 The secondary bronchi and bronchioles are most often affected, in relation to the main bronchi and trachea. The origin physiopathology is thought to involve transmural spread of hilar adenopathies or blood spread from an extrathoracic focus.6 Lesions may present as platyform mucosal infiltrates with superficial ulceration or, more rarely, a single polypoid mass.
In this patient, the diagnosis of endobronchial lymphoma was an incidental finding during EBUS procedure aimed to evaluate mediastinal lymphadenopathy. The presence of non-caseating epithelioid granulomas could be inferred as a recurrence of sarcoidosis.
In summary, this case highlights the differential diagnosis between sarcoidosis and lymphoma, the possibility of their overlap and the need for systematic exploration of the tracheobronchial tree in suspected lymphoma. Bronchoscopy evaluation in these patients might allow the histological diagnosis through lesion biopsy and the evaluation of the extent of HL, which will influence the prognosis and treatment of the disease.
Authors’ contributionStudy Conception and design: Catarina Barata, José Pedro Boléo-Tomé.
Data acquisition: Catarina Barata, Margarida Isabel Pereira, Miguel Barbosa.
Data analysis and interpretation: Catarina Barata, Margarida Isabel Pereira, Miguel Barbosa, Filipa Mousinho.
Dafting of the manuscript: Catarina Barata, Margarida Isabel Pereira, Miguel Barbosa
Critical revision of the manuscript for important intelectual content: Filipa Mousinho, José Pedro Boléo-Tomé.
All authors read and approved the final manuscript.