To compare imaging findings, lung function variables and cardiopulmonary exercise testing (CPET) results between Brazilian sandblasters of shipyard and stone carvers with silicosis.
MethodsOf the 41 patients, 25 subjects were sandblasters and 16 were stone carvers, with median ages of 52 and 46.4 years, respectively. All of the patients underwent pulmonary function tests (PFTs) and CPET. Chest radiographs were classified according to the International Labour Organization recommendations. The following parameters were examined through the use of high-resolution computerized tomography (HRCT): nodules, progressive massive fibrosis (PMF), emphysema, and intrathoracic lymph node enlargement.
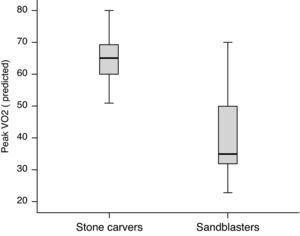
ResultsLarge opacities on chest radiography were observed in 76% of sandblasters and only 18.7% of stone carvers. Using HRCT, PMF was identified in 92% of sandblasters and only 43.7% of stone carvers. Although carbon monoxide diffusing capacity results were significantly different between the sandblasters and stone carvers, these differences were more pronounced in the CPET results. While 92% of sandblasters failed to reach at least 80% of their predicted peak oxygen uptake (VO2), this was observed for only 43.7% of stone carvers. A breathing reserve of less than 25% was observed in 40.5% of sandblasters but not in any of the stone carvers.
ConclusionIn silicosis, imaging findings, lung function and CPET results are strongly influenced by the type of exposure to silica dust. Additionally, CPET abnormalities are more pronounced compared to measurements taken at rest.
Comparação dos achados de imagem, função pulmonar e teste de exercício cardiopulmonar (TECP) entre jateadores de areia de estaleiro e escultores de pedra com silicose no Brasil.
MétodosDos 41 pacientes, 25 eram jateadores de areia e 16 eram escultores de pedra, com medianas da idade de 52 e 46,4 anos, respetivamente. Todos os pacientes se submeteram aos testes de função pulmonar e ao TECP. As radiografias de tórax foram classificadas de acordo com as recomendações da Organização Internacional do Trabalho. Os seguintes parâmetros foram avaliados na tomografia computadorizada de alta resolução (TCAR): nódulos, fibrose maciça progressiva (FMP), enfisema e aumento dos linfonodos intratorácicos.
ResultadosGrandes opacidades na radiografia de tórax foram observadas em 76% dos jateadores e em somente 18,7% dos escultores. Por utilizar a TCAR, FMP foi identificada em 92% dos jateadores e em somente 43,7% dos escultores. Embora os resultados da capacidade de difusão do monóxido de carbono tenham sido significativamente diferentes entre os 2 grupos, essas diferenças foram mais acentuadas nos resultados do TECP. Enquanto 92% dos jateadores não conseguiu atingir pelo menos 80% de seu pico de consumo de oxigénio (VO2) predito, isto foi observado em somente 43,7% dos escultores. Foi observada uma reserva ventilatória de menos de 25% em 40,5% dos jateadores e em nenhum dos escultores.
ConclusãoNa silicose, os achados de imagem, função pulmonar e TECP são fortemente influenciados pelo tipo de exposição à poeira de sílica. Adicionalmente, as anormalidades do TECP são mais acentuadas quando comparadas com aquelas medidas tomadas em repouso.
Silicosis, the most prevalent form of pneumoconiosis, is a preventable, but untreatable, environmental pulmonary disease that can be fatal through the impairment of overall health status.1 The disease occurs when workers are exposed to quartz-containing dust; common professions at risk for silicosis include tunneling, quarrying, mining, and foundry work.3
Although sandblasting was reported as a source of silicosis in Brazil, the use of sandblasting has been banned by the Ministry of Labor and Employment since 2005.4 However, many former shipyard workers in the city of São Gonçalo of Rio de Janeiro State still live with the consequences of silicosis.5,6 Exposure through sandblasting appears to be more hazardous compared to many other known sources of silica dust because of the intense exposure during long work hours under very poor hygienic conditions without any efficient respiratory protection.1,7
In Brazil, silicosis is also observed among stone carvers.8 In the region of the Baixada Fluminense of Rio de Janeiro State, various workers produce stone souvenirs, frequently for export. All belong to the informal economy and work in small and rudimentary workshops.9
The use of CPET in clinical medicine has become established, primarily as a tool for understanding the mechanisms of exercise intolerance and fatigue. In patients with silicosis, dyspnea on exertion is frequently reported by these patients, even when resting cardiopulmonary measurements (including PFTs and arterial blood gas levels) are within the reference ranges. Thus, CPET may constitute a more sensitive way of assessing pulmonary impairment than resting functional evaluation.10
Given the different activities that lead to silicosis, the objective of this study was to compare the imaging findings, lung function variables and CPET results between sandblasters and stone carvers with silicosis.
MethodsPatientsA cross-sectional study was performed to evaluate 52 nonsmokers with silicosis. Silicosis was defined as a chest radiograph with an International Labour Office (ILO) classification of ≥1/0 in a worker with a history of silica dust exposure.11 Smokers and former smokers were excluded, as were individuals in whom the radiological findings indicated pulmonary tuberculosis. Subjects whose laboratory findings indicated cardiac or neuromuscular disease and subjects who failed to undergo CPET were also excluded. Based on these criteria, 11 patients were excluded for history of smoking (5), imaging findings consistent with pulmonary tuberculosis (4), cardiac disease (1), and neuromuscular disease (1). Prior to participation, subjects were informed about the objective of the study and gave written informed consent. The study protocol was approved by the Research Ethics Committee of the State University of Rio de Janeiro (Number 1117-CEP/HUPE).
In total, 41 patients diagnosed with silicosis were investigated. Of these, 25 were sandblasters and 16 were stone carvers. All sandblasters were former workers in shipyards. These workers had used sandblasting as an abrasive method to remove rust and coating residues contained in ship's hull. Subjects had not worked in other silicosis-causing jobs previously. Additionally, none of the subjects reported engaging in hobbies associated with a risk for silicosis. No exposure assessments or worksite visits were performed.
MeasurementsDyspnea severity was estimated using the following standard five-point scale from the Medical Research Council.11
Chest radiographs were taken in the anteroposterior position using a Siemens X-ray unit model LX30 (Siemens AG, Erlangen, Germany). Three “B” readings interpreted the radiographs in independent sessions. Small opacity profusions were classified as follows: 0/−, 0/0, 0/1, 1/0, 1/1, 1/2, 2/1, 2/2, 2/3, 3/2, 3/3 or 3/+. According to the ILO standards, large opacities were classified as type A, B or C.12 Results are presented as the median values for all readings.
All HRCT examinations were performed using a high-resolution scanner (GE HiSpeed Advantage, General Electric Medical Systems, Milwaukee, WI, USA). All images were reviewed by 4 experienced radiologists, and consensus findings were reported. For the purpose of this study, PMF was defined as the presence of at least an opacity or coalescence larger than 1cm following the ILO classification of coalescence or large opacity.5,13,14
PFTs were completed using the Collins Plus Pulmonary Function Testing System (Warren E. Collins, Inc., Braintree, MA, USA); American Thoracic Society standards were followed for both the procedure and data interpretation.15,16 The results are expressed as a percent of the predicted values for the Brazilian population.17–19
Each subject performed symptom-limited maximal exercise testing using an electronically braked cycle ergometer connected to the Collins Plus Pulmonary Function Testing System (Warren E. Collins, Inc., Braintree, MA, USA). Breathing reserve was calculated as the difference between the measured resting maximum voluntary ventilation (MVV) and the peak minute ventilation (VE) and was expressed as a percentage of the MVV [1−(VE/MVV)×100].20,21 Heart rate reserve (HRR) was calculated as the difference between the peak and resting heart rates [(220−age)−peak HR].22 These values were then compared to values predicted by Neder et al.23 for the adult Brazilian population.
Statistical analysisTo check the homogeneity of the sample, a Kolmogorov–Smirnov's test was used. Results are expressed as the median and interquartile range values or frequencies (percentage). The sandblaster group was compared to the stone carver group using the Mann–Whitney test for numerical variables and Fisher's exact test for categorical variables. Data analysis was performed using SAS 6.11 software (SAS Institute, Inc., Cary, NC, USA). Differences were considered significant when P<0.05.
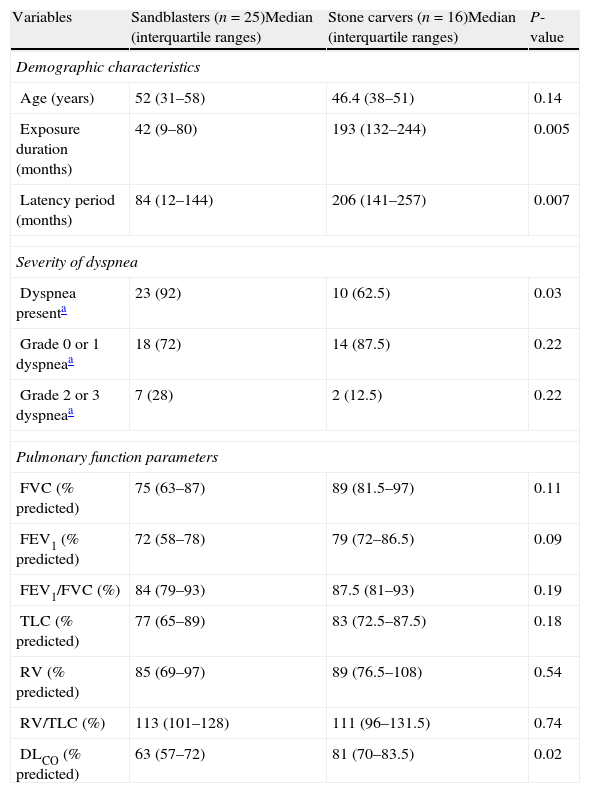
ResultsThe median age of the 41 patients was 48 years (range, 23–74 years); except for two artisans, all participants were men. The median duration of silica dust exposure and latency period was 96 months (range, 9–244 months) and 132 months (range, 12–257 months), respectively. The median follow-up period of the patients was 72 months (range, 12–122). Most of the patients reported working without a breathing-mask. No sandblasters were still working in occupations with silica dust exposure at the time of the study. However, half of the artisans were active in work environments with silica-dust exposure at the time the study was being conducted. Case characteristics separated according to occupation (sandblasters vs. stone carvers) are presented in Table 1.
Comparison between sandblasters and stone carvers according to the demographic data, severity of dyspnea and pulmonary function parameters.
| Variables | Sandblasters (n=25)Median (interquartile ranges) | Stone carvers (n=16)Median (interquartile ranges) | P-value |
| Demographic characteristics | |||
| Age (years) | 52 (31–58) | 46.4 (38–51) | 0.14 |
| Exposure duration (months) | 42 (9–80) | 193 (132–244) | 0.005 |
| Latency period (months) | 84 (12–144) | 206 (141–257) | 0.007 |
| Severity of dyspnea | |||
| Dyspnea presenta | 23 (92) | 10 (62.5) | 0.03 |
| Grade 0 or 1 dyspneaa | 18 (72) | 14 (87.5) | 0.22 |
| Grade 2 or 3 dyspneaa | 7 (28) | 2 (12.5) | 0.22 |
| Pulmonary function parameters | |||
| FVC (% predicted) | 75 (63–87) | 89 (81.5–97) | 0.11 |
| FEV1 (% predicted) | 72 (58–78) | 79 (72–86.5) | 0.09 |
| FEV1/FVC (%) | 84 (79–93) | 87.5 (81–93) | 0.19 |
| TLC (% predicted) | 77 (65–89) | 83 (72.5–87.5) | 0.18 |
| RV (% predicted) | 85 (69–97) | 89 (76.5–108) | 0.54 |
| RV/TLC (%) | 113 (101–128) | 111 (96–131.5) | 0.74 |
| DLCO (% predicted) | 63 (57–72) | 81 (70–83.5) | 0.02 |
FVC: forced vital capacity; FEV1: forced expiratory volume in one second; TLC: total lung capacity; RV: residual volume; DLCO: carbon monoxide diffusing capacity.
Among the sandblasters, 21 (84%) had ventilatory impairment: restrictive defect was identified in 8 (32%), obstructive in 6 (24%), and mixed in 7 (28%). Among the stone carvers, 11 (68.7%) had ventilatory impairment: restrictive defect was identified in 3 (18.8%), obstructive in 5 (31.2%), and mixed in 3 (18.8%). The carbon monoxide diffusion capacity (DLCO) was at the lower limit of normality in 22 (88%) sandblasters and 7 (43.7%) stone carvers.
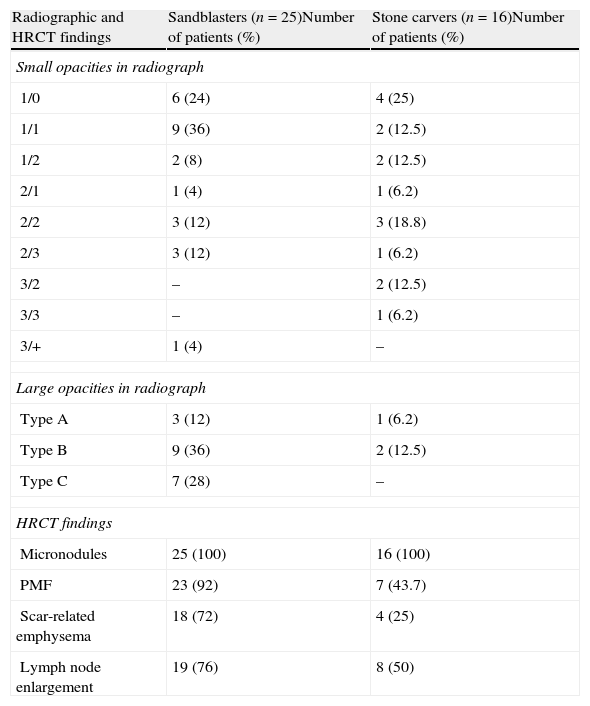
Of the 41 chest radiographs, the inter-reader agreement for small opacity profusion and of the large opacity type revealed kappa coefficients of 0.38 (P<0.001) and 0.72 (P<0.001), respectively. The distribution of sandblasters and stone carvers in the ILO radiological categories and HRCT findings are presented in Table 2.
Radiographic abnormalities and high-resolution computerized tomography findings in sandblasters and stone carvers.
| Radiographic and HRCT findings | Sandblasters (n=25)Number of patients (%) | Stone carvers (n=16)Number of patients (%) |
| Small opacities in radiograph | ||
| 1/0 | 6 (24) | 4 (25) |
| 1/1 | 9 (36) | 2 (12.5) |
| 1/2 | 2 (8) | 2 (12.5) |
| 2/1 | 1 (4) | 1 (6.2) |
| 2/2 | 3 (12) | 3 (18.8) |
| 2/3 | 3 (12) | 1 (6.2) |
| 3/2 | – | 2 (12.5) |
| 3/3 | – | 1 (6.2) |
| 3/+ | 1 (4) | – |
| Large opacities in radiograph | ||
| Type A | 3 (12) | 1 (6.2) |
| Type B | 9 (36) | 2 (12.5) |
| Type C | 7 (28) | – |
| HRCT findings | ||
| Micronodules | 25 (100) | 16 (100) |
| PMF | 23 (92) | 7 (43.7) |
| Scar-related emphysema | 18 (72) | 4 (25) |
| Lymph node enlargement | 19 (76) | 8 (50) |
HRCT: high-resolution computerized tomography; PMF: progressive massive fibrosis.
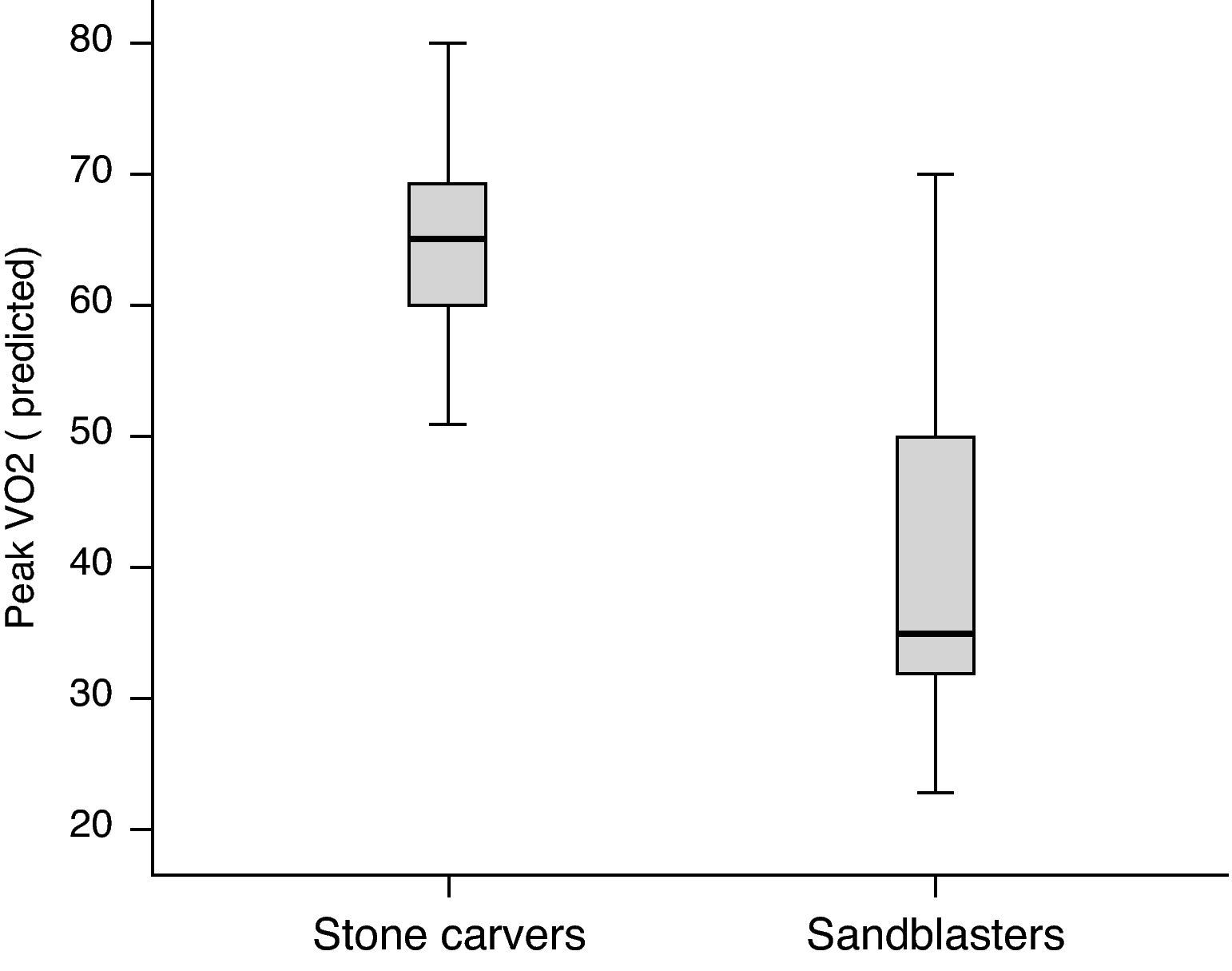
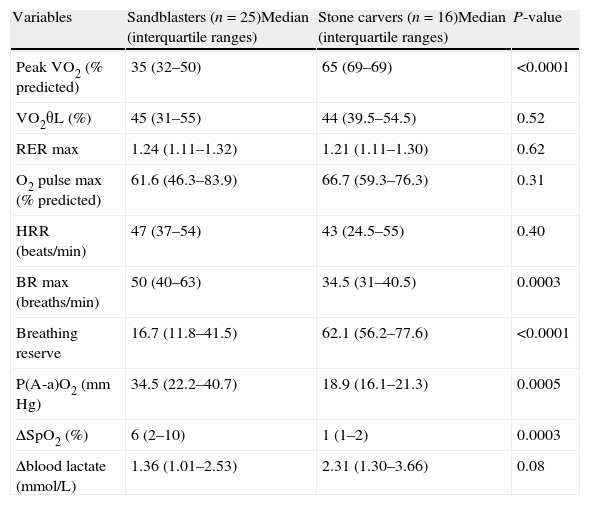
The CPET results for each patient population (sandblasters vs. stone carvers) are summarized in Table 3 and Fig. 1. While 92% of sandblasters failed to reach at least 80% of their predicted peak VO2, this was observed in only 43.7% of stone carvers. A breathing reserve of less than 25% was observed in 40.5% of sandblasters; this was not observed in any stone carver. Additionally, 48% of sandblasters had P(A-a)O2 values greater than 35mmHg; this was not observed for any stone carver.
Comparison between sandblasters and stone carvers according to the cardiopulmonary exercise testing results.
| Variables | Sandblasters (n=25)Median (interquartile ranges) | Stone carvers (n=16)Median (interquartile ranges) | P-value |
| Peak VO2 (% predicted) | 35 (32–50) | 65 (69–69) | <0.0001 |
| VO2θL (%) | 45 (31–55) | 44 (39.5–54.5) | 0.52 |
| RER max | 1.24 (1.11–1.32) | 1.21 (1.11–1.30) | 0.62 |
| O2 pulse max (% predicted) | 61.6 (46.3–83.9) | 66.7 (59.3–76.3) | 0.31 |
| HRR (beats/min) | 47 (37–54) | 43 (24.5–55) | 0.40 |
| BR max (breaths/min) | 50 (40–63) | 34.5 (31–40.5) | 0.0003 |
| Breathing reserve | 16.7 (11.8–41.5) | 62.1 (56.2–77.6) | <0.0001 |
| P(A-a)O2 (mmHg) | 34.5 (22.2–40.7) | 18.9 (16.1–21.3) | 0.0005 |
| ΔSpO2 (%) | 6 (2–10) | 1 (1–2) | 0.0003 |
| Δblood lactate (mmol/L) | 1.36 (1.01–2.53) | 2.31 (1.30–3.66) | 0.08 |
Peak VO2: peak oxygen uptake; VO2θL: peak VO2 at the estimated lactate threshold; RER max: maximum respiratory exchange ratio (VCO2/VO2) at peak exercise; O2 pulse max: maximum oxygen pulse (VO2/heart rate) at peak exercise; HRR: heart rate reserve; BR max: maximum respiratory rate at peak exercise; P(A-a)O2: alveolar-arterial oxygen pressure gradient at peak exercise; ΔSpO2: difference between peak and resting oxygen saturation; Δblood lactate: difference between peak and resting blood lactate.
This study shows that sandblasting causes worse clinical outcomes although sandblasters have less exposure duration and shorter latency period compared to stone carvers. Differences in results can be observed in imaging findings, lung function variables and CPET measurements.
In a study with 49 silicosis patients, Moreira et al.26 showed that the HRCT is more sensitive than the chest radiography in the evaluation of the intrathoracic abnormalities.26 The superiority of HRCT over chest radiograph for the detection of large opacities and emphysema has been well established.2,24–26 As reported by other authors,25,27–29 we demonstrated that HRCT identifies more PMF when compared with chest radiographs. In some patients with silicosis, it is possible that a confluence of nodules on HRCT is viewed only as a background of diffuse pulmonary nodules on chest radiograph.
Interestingly, the present study identified PMF in 25 sandblasters (92%) and only 7 stone carvers (43.7%). Similarly, Antao et al.29 found PMF in 39.1% of stone carvers. Unlike our results, Alper et al.1 observed PMF in half of the cases of silicosis in denim sandblasters. Although both studies showed similar latency periods (median 84 vs. mean 82 months), the exposure durations, ages of the workers, and criteria for the diagnosis of PMF on HRCT were different; this makes it difficult to reach a conclusion about the different frequencies of PMF between the two studies. Despite these considerations, the identification of PMF is important because it is the replacement of aerated lung tissue with a mass of non-functional fibrous tissue; additionally, it is usually associated with impaired lung function, disability, and premature death.30 A significantly increased relative risk of PMF is associated with higher levels of dust exposure30; in our study, this may be a possible explanation for the higher frequency of PMF observed in sandblasters.
In the present study, there were no significant differences on PFT results when sandblasters were compared with stone carvers. However, while DLCO values were only slightly altered in the artisans, pronounced changes were observed in the sandblasters (P=0.02). Interestingly, DLCO has been found to be fairly correlated with gas exchange abnormalities during exercise, and particularly to be the best predictive and sensitive index of a fall in PaO2.31
CPET allows for the objective determination of exercise functional capacity and for the evaluation of the mechanisms underlying exercise limitation.32 In the present study, on comparing the sandblasters to the stone carvers, the CPET response variables exhibited higher significant differences in relation to measurements taken at rest. This is not necessarily surprising because exercise capacity is the result of the response of multiple factors, including gas exchange across the lung, blood oxygen content, and tissue uptake of oxygen.33
The measurement of peak VO2 remains the best available index for the assessment of exercise capacity.32 In the current study, while almost all the sandblasters failed to reach at least 80% of the peak VO2 (% predicted), this occurred in less than half of the stone carvers. Violante et al.10 who evaluated 45 silicosis patients with different occupational fields including foundry work, coal or metal mining and milling, and sandblasting, observed peak VO2 values (% predicted) below 80% in 35 patients.
In the present study, the sandblasters had a lower breathing reserve compared to the stone carvers (P<0.0001). Similarly, Wang et al.33 found low breathing reserve values in silicosis patients who had been engaged in the manufacturing of fire-proof bricks in China. According to these authors, the increase in ventilatory demand was presumably due to the increase in dead space ventilation secondary to ventilation-perfusion mismatching; further, decreased blood oxygen saturation stimulates the peripheral respiratory receptors to impel breathing rates to increase. We hypothesize that the higher frequency of PMF observed in sandblasting-induced silicosis could explain these functional abnormalities.
Some limitations of this study must be addressed. First, the patient groups may not be representative of the entire population of sandblasters and stone carvers of the regions involved. Second, information on the exact type of silica and the concentrations of silica to which subjects were exposed was not available. Finally, suboptimal subject effort alone could account for the reduced peak VO2 readings. However, all patients were actively encouraged during exercise to reach a maximum, and they showed high blood lactate levels and high respiratory exchange ratios.32
In conclusion, the data indicate that imaging findings, lung function variables and CPET results are strongly influenced by the type of silica dust exposure in silicosis patients. In addition, when the sandblasters were compared with stone carvers, CPET abnormalities were more pronounced compared to measurements taken at rest. To our knowledge, this is the first study comparing two different groups of workers exposed to silica dust using CPET analysis.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Lopes AJ, et al. Silicose em jateadores de areia de estaleiro versus silicose em escultores de pedra no Brasil: uma comparação dos achados de imagem, função pulmonar e teste de exercício cardiopulmonar. Rev Port Pneumol. 2012. doi:10.1016/j.rppneu.2012.04.006