Evaluate patients admitted for hemoptysis, its etiology, use of diagnostic tests, treatment and outcome.
Material and methodsA retrospective analysis was done, checking clinical files of patients admitted for hemoptysis, between 1st January 2004 and 31st December 2008.
ResultsTwo hundred and thirty seven patients were included in this study, with a mean age of 57.9 years. In patients under 18 years, the most frequent diagnoses were bronchiectasis and congenital cardiopathy. In adults, pulmonary tuberculosis sequelae and bronchiectasis were the dominant diagnoses (22.2 % and 15.8 %, respectively), followed by lung cancer. Active infection was responsible for bleeding in 51 patients, especially pulmonary tuberculosis, pneumonia and tracheobronchitis. The etiology of hemoptysis was not established in 6.3 %. All patients performed chest X-Ray. Chest CT was performed in 81.4 % of patients and fiberoptic bronchoscopy in 52.7 %, the latter locating the source of bleeding in 38.4 % and establishing a final diagnosis in 17.6 %. In most patients, effective control of bleeding was achieved by medical treatment (90.7 %). During these 5 years, arterial embolization was performed in 11.8 % of patients. The main reason for embolization was recurrence prevention. There were 14 deaths (5.9 %), being identified as poor prognostic factors, hemodynamic instability and malignancy.
ConclusionsHemoptysis is still a frequent symptom, being chronic infection sequelae and lung cancer their main causes. In this study, factors associated with a worse prognosis were hemodynamic instability and malignancy.
Avaliar doentes admitidos por hemoptises quanto à etiologia, meios diagnósticos, tratamento e evolução.
Material e métodosRealizou-se um estudo retrospectivo dos doentes admitidos no Hospital de São João, por hemoptises, entre 1 de janeiro de 2004 e 31 de dezembro de 2008.
ResultadosForam estudados 237 doentes, com idade média de 57,9 anos. Nos doentes com idade inferior a 18 anos, os diagnósticos mais frequentes foram bronquiectasias e cardiopatia congénita. Nos adultos, as sequelas de tuberculose pulmonar e as Bronquiectasias foram os diagnósticos predominantes (22,2 % e 15,8 %, respectivamente), seguidos pela neoplasia pulmonar. A infecção foi responsável pelas perdas hemáticas em 51 doentes, essencialmente tuberculose pulmonar, pneumonia e traqueobronquite. A etiologia ficou por esclarecer em 6,3 %. Todos os doentes realizaram radiografia de tórax. A TAC foi realizada em 81,4 % dos doentes e a broncofibroscopia em 52,7 %, esta última localizando a fonte da hemorragia em 38,4 % e estabelecendo diagnóstico definitivo em 17,6 %. Na maioria dos casos (90,7 %), a hemorragia foi controlada com tratamento médico. Ao longo destes 5 anos, 11,8 % dos doentes foram submetidos a embolização arterial, sendo a prevenção de recidiva o principal motivo da sua realização. Foram registados 14 óbitos (5,9 %), sendo identificados, como factores de mau prognóstico, a instabilidade hemodinâmica e a etiologia neoplásica.
ConclusõesAs hemoptises continuam a ser um sintoma frequente, sendo actualmente as sequelas associadas a infecções crónicas e as neoplasias as principais etiologias. Neste estudo, os factores de pior prognóstico foram a instabilidade hemodinâmica e a etiologia neoplásica.
Hemoptysis is defined as the spitting or coughing up of blood, caused by bleeding of the lungs or from the tracheobronchial tree. It may be a symptom of several diseases, more or less severe, but its appearance induces concern to the patient and requires a full diagnostic investigation.
Bronchiectasis, pulmonary tuberculosis and lung cancer are the main causes of hemoptysis. The frequency of each disease as a cause of hemoptysis varies in different series, according to the geographical area. Pulmonary tuberculosis is an important cause of hemoptysis in developing countries,1–4 whereas, in developed countries, bronchiectasis, lung cancer and bronchitis are the main causes.5–7 In Portugal, pulmonary tuberculosis is still a frequent disease, but it has significantly decreased in recent years.8,9
In children, bronchiectasis (particularly in cystic fibrosis) and congenital cardiopathies are responsible for most cases of hemoptysis. 10,11 Some studies have found pulmonary tuberculosis as an important cause in patients under 18 years old.12,13
Besides a correct anamnesis and a detailed physical exam, diagnostic tests are an important part of the diagnostic evaluation, such as chest X-Ray, chest CT scan and bronchoscopy.6,14–17 Other tests may be important, namely bronchial arteriography and echocardiogram.16 Studies also refer that the demand of the diagnostic investigation should be based on how high or low the probability for a lung cancer diagnostic is.6,15,18–20
Even after an adequate investigation, no cause can be established in 20-30 % of patients.16,21,22
In most patients, control of bleeding is achieved with conservative measures.4,7 However, other therapeutic measures may be necessary, such as bronchoscopic intervention,23 surgery or bronchial artery embolization. Embolization‘s efficacy in the control of bleeding has already been validated, with success rates of 85-99 %, 24–29 even higher than surgery.30 Bronchial artery embolization has also an important role in recurrent chronic hemoptysis, for recurrence prevention. However, it has not yet been considered a definitive therapeutic measure, because of its recurrence rate which is higher than 25 %. 28,31–33
ObjectiveEvaluate patients admitted for hemoptysis, its etiology, use of diagnostic tests, treatment and evolution.
MethodsA retrospective study was performed, analyzing clinical files of patients admitted for hemoptysis, in the Hospital de Sao Joao, Porto, between 1st January of 2004 and 31 December of 2008.
Two hundred and eighty patients were included. Of these, 43 were excluded: 7 for hemorrhage of non-respiratory origin (digestive tract, mouth and otorhinolaryngological); 3 for lack of adequate information; and 33 for repeated admissions (only the 1st admission of each patient was analyzed).
Two hundred and thirty seven clinical files were analyzed. Clinical information was reviewed: age, sex, smoke status, medical history, use of anti-agregant or anticoagulant medication, severity criteria, use of diagnostic tests, definitive diagnosis, treatment and evolution. Due to the lack of information about the volume of blood loss, severity assessment was based on clinical criteria: reduction of hemoglobin concentration > 1g, hemodynamic instability (defined as systolic arterial blood pressure < 90mmHg) and respiratory failure (defined as arterial oxygen partial pressure < 60mmHg).
Tracheobronchitis diagnosis was defined as lower respiratory infection, without associated radiologic image.
Data were analyzed using statistical software Epi Info, version 3.5.1. Exact Fisher Test was used to evaluate statistical significance (a p value less than 0.01 was considered statistically significant).
ResultsPatients’ characterizationTwo hundred and thirty seven patients were studied, 165 male (69.6 %) and 72 female (30.4 %), with an average age of 57.9 years old. Pediatric age (less than 18 years) was found in 6.8 % of patients. Predominant age groups were 50-59 years and 60-69 years, both accounting for 21.1 % of patients.
Most adults (57.9 %) were current or former smokers. Thirty-three patients (13.9 %) were under anticoagulants (warfarin) and 31 (13.1 %) under anti-agregants. Coagulation blood tests were normal in most patients (69.2 %) and showed alterations in 53 (22.4 %). Of these, 14 (26 %) were under anti-agregants and 33 (62.3 %) under oral anticoagulants.
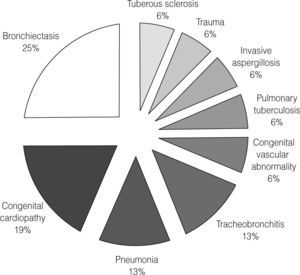
EtiologyIn pediatric age, most frequent diagnoses were bronchiectasis and congenital cardiopathy (25 % and 18.8 %, respectively), as shown in Figure 1.
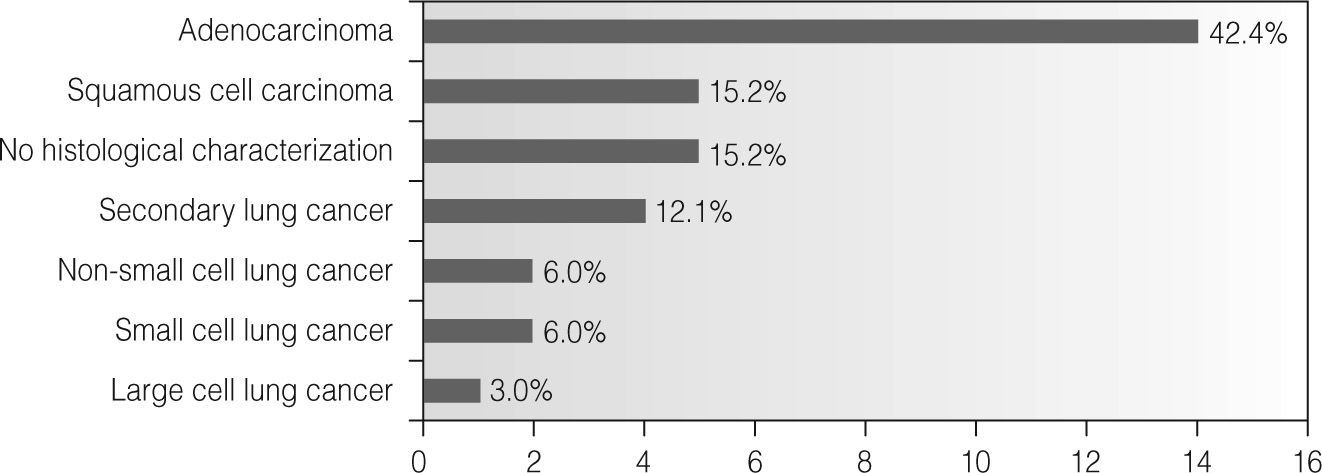
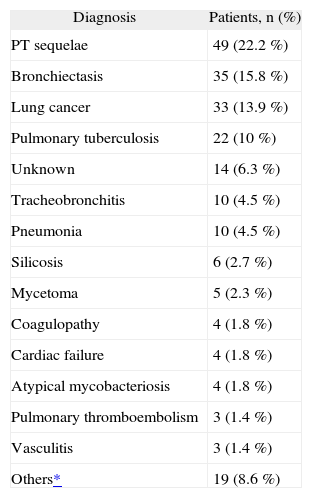
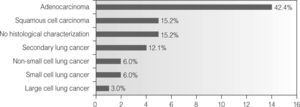
In adults (Table 1), pulmonary tuberculosis (PT) sequelae and bronchiectasis were the main diagnoses found (22.2 % and 15.8 %, respectively). Lung cancer was diagnosed in 33 patients, being the 3rd most frequent diagnosis. Most (87.9 %) were found to have primary lung cancer, and adenocarcinoma was the predominant histological type. Only 4 patients (12.1 %) had secondary lung cancer (Figure 2) - pulmonary metastasis of neoplasm in other location (breast, esophagus and larynx). We would like to acknowledge the large number of patients without a full histological characterization (7 patients - 21.2 % of all patients with lung cancer). In 5 patients, histological characterization was absent of the clinical file and 2 patients were diagnosed with non-small cell lung cancer without further characterization. Infection was responsible for bleeding in 51 patients (23 %), 22 with pulmonary tuberculosis, followed by pneumonia, tracheobronchitis and, less commonly, mycetoma and atypical mycobacteriosis. In 4 patients, hemoptysis’ etiology was coagulopathy; of these, coagulopathy was iatrogenic in 3. They were patients medicated with anticoagulants. No diagnosis was reached in 6.3 % (14 patients).
Hemoptysis’ etiology in adults (n = 221)
| Diagnosis | Patients, n (%) |
| PT sequelae | 49 (22.2 %) |
| Bronchiectasis | 35 (15.8 %) |
| Lung cancer | 33 (13.9 %) |
| Pulmonary tuberculosis | 22 (10 %) |
| Unknown | 14 (6.3 %) |
| Tracheobronchitis | 10 (4.5 %) |
| Pneumonia | 10 (4.5 %) |
| Silicosis | 6 (2.7 %) |
| Mycetoma | 5 (2.3 %) |
| Coagulopathy | 4 (1.8 %) |
| Cardiac failure | 4 (1.8 %) |
| Atypical mycobacteriosis | 4 (1.8 %) |
| Pulmonary thromboembolism | 3 (1.4 %) |
| Vasculitis | 3 (1.4 %) |
| Others* | 19 (8.6 %) |
Arteriovenous fistulae (2), post-lobectomy complication (2), mitral stenosis (2), COPD (2), pulmonary abscess (1), congenital cardiopathy (1), tracheal foreign body (1), post-radiation pulmonary fibrosis (1), foreign body granuloma (1), tracheal invasion for medastinal mass (1), benign endobronchial lesion (1), vascular malformation (1), interstitial pneumonitis (1), radiation pneumonitis (1), aortic aneurysm rupture (1).
By age group, it appears that pulmonary tuberculosis sequelae (PT sequelae) was one of the main diagnoses in all of them. Malignancy had an increasing predominance with the increasing of age, being the main diagnosis in the group of patients of 70-79 years.
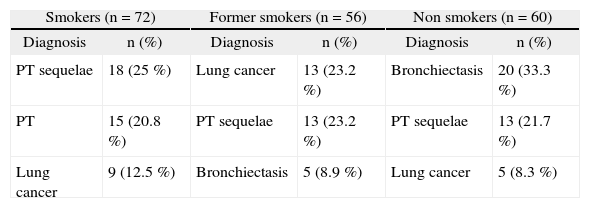
The 3 main diagnoses according to smoking history of adult patients are presented in Table 2. It‘s obvious the greater importance of malignancy in smokers and former smokers. In the patients with a positive smoking history (smokers and former smokers), lung cancer was responsible for 17.2 % of hemoptysis, and for only 8.3 % in non-smokers. No significant differences were found in hemoptysis’ etiology in former smokers whose date of smoking cessation was superior or inferior to 10 years.
Main etiologies of hemoptysis, according to the smoking history of adults (n = 188)
| Smokers (n = 72) | Former smokers (n = 56) | Non smokers (n = 60) | |||
| Diagnosis | n (%) | Diagnosis | n (%) | Diagnosis | n (%) |
| PT sequelae | 18 (25 %) | Lung cancer | 13 (23.2 %) | Bronchiectasis | 20 (33.3 %) |
| PT | 15 (20.8 %) | PT sequelae | 13 (23.2 %) | PT sequelae | 13 (21.7 %) |
| Lung cancer | 9 (12.5 %) | Bronchiectasis | 5 (8.9 %) | Lung cancer | 5 (8.3 %) |
Note: A smoking history was not found in 33 patients (14.9 %).
Sixty-eight percent of patients with pulmonary tuberculosis were current smokers.
In patients medicated with anticoagulants (33), the main diagnosis was lung cancer (18.2 %), predominantly adenocarcinoma.
In 55.7 % (132 patients), this was the first episode of hemoptysis, while 35 % already had previous episodes. In others (9.3 %), no information was obtained. The main diagnoses were not significantly different in patients with or without previous episodes of hemoptysis, with the exception of pulmonary tuberculosis. In fact, this was the first episode in approximately 82 % of patients with pulmonary tuberculosis.
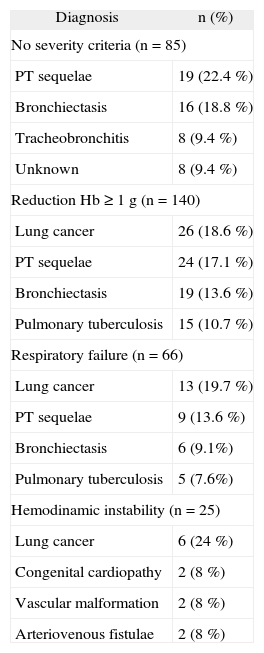
Hemoptysis’ classification based on the amount of bleeding, besides being a non-specific data, was missing in most clinical files. So, severity was based on the magnitude of clinical effect, evaluating some clinical criteria, such as reduction of hemoglobin concentration (superior to 1g), respiratory failure and hemodynamic instability. Table 3 presents the main diagnoses for each severity criteria. When all severity criteria were found (16 patients), malignancy was predominant (80 %).
Hemoptysis’ etiology, according to severity criteria
| Diagnosis | n (%) |
| No severity criteria (n = 85) | |
| PT sequelae | 19 (22.4 %) |
| Bronchiectasis | 16 (18.8 %) |
| Tracheobronchitis | 8 (9.4 %) |
| Unknown | 8 (9.4 %) |
| Reduction Hb ≥ 1g (n = 140) | |
| Lung cancer | 26 (18.6 %) |
| PT sequelae | 24 (17.1 %) |
| Bronchiectasis | 19 (13.6 %) |
| Pulmonary tuberculosis | 15 (10.7 %) |
| Respiratory failure (n = 66) | |
| Lung cancer | 13 (19.7 %) |
| PT sequelae | 9 (13.6 %) |
| Bronchiectasis | 6 (9.1%) |
| Pulmonary tuberculosis | 5 (7.6%) |
| Hemodinamic instability (n = 25) | |
| Lung cancer | 6 (24 %) |
| Congenital cardiopathy | 2 (8 %) |
| Vascular malformation | 2 (8 %) |
| Arteriovenous fistulae | 2 (8 %) |
All patients performed a chest X-Ray, which was described as normal in only 30 (12.7 %). Of these, the main diagnoses were tracheobronchitis (6), bronchiectasis (4), unknown etiology (4) and PT sequelae (3). Among patients with unknown etiology of hemoptysis whose chest X-Ray was normal, chest CT scan was also described as normal in 2 (the other 2 patients had ground glass pattern in chest CT scan) and bronchoscopy didn‘t show abnormalities in the 3 patients who were submitted to it. One patient with pulmonary tuberculosis had a normal chest X-Ray. No malignancy was diagnosed in patients with a normal chest-X-Ray.
Chest CT scan was performed in 193 patients (81.4 %), and abnormalities were found in most of them (187). The predominant pattern was linear retractile opacities (24.1 %), in accordance with the frequency of diagnoses. Among patients with lung cancer, CT scan had a good diagnostic yield, showing abnormalities in all of them. Only 1 patient had CT scan abnormalities that were not suggestive of malignancy. Among patients with a normal chest CT scan (6), the main diagnosis was tracheobronchitis (3 patients) and no diagnosis was found in the rest of them. Four patients with a normal CT scan performed bronchoscopy, and no endobronchial abnormalities were found.
Bronchoscopy was performed in 125 patients (52.7 %). Among patients with a higher probability of malignancy (age > 50 years and a positive smoking history — current or former), excluding those whose malignancy was already known, we found that 67.4 % were submitted to a bronchoscopy. The higher probability of lung cancer was associated with the performance of a bronchoscopy; this association was statistically significant (p < 0.01).
Bronchoscopy was able to localize the source of bleeding in 38.4 % of patients and allowed the establishment of a definitive diagnosis in 17.6 %, mainly pulmonary tuberculosis and lung cancer. In 55 patients (44 %), no endobronchial abnormality was found. Bronchoscopic evaluation was performed by a flexible fiberoptic bronchoscope in almost every patient. Rigid bronchoscopy was performed in only 5 patients, for different reasons: diagnosis (when the amount of bleeding was not compatible with a fiberoptic bronchoscopy), restoration of an adequate airway (in a case of obstruction of the airway by a tumor) and replacement of a tracheal stent.
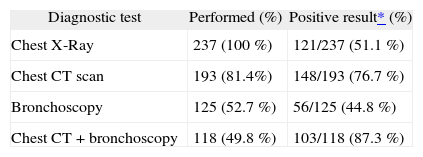
The diagnostic yield of each diagnostic test is presented in Table 4. We did not include angiography as a diagnostic test, because in this group of patients, it was used almost exclusively as a therapeutic method. Three patients were diagnosed with bronchial circulation abnormalities (2 with arteriovenous fistula and 1 with an abnormal origin of bronchial artery).
Diagnostic yield of each diagnostic test performed in the group of patients of this study (n = 237)
| Diagnostic test | Performed (%) | Positive result* (%) |
| Chest X-Ray | 237 (100 %) | 121/237 (51.1 %) |
| Chest CT scan | 193 (81.4%) | 148/193 (76.7 %) |
| Bronchoscopy | 125 (52.7 %) | 56/125 (44.8 %) |
| Chest CT + bronchoscopy | 118 (49.8 %) | 103/118 (87.3 %) |
In 6.3 % (14), no diagnosis was reached. Among these patients, 5 (35.7 %) were transferred, after stabilization, to another hospital (according to the area of residence), which is why they did not complete the diagnostic evaluation in this hospital; 1 patient (7.1 %) died before completing the study. Among the 8 patients that completed the diagnostic evaluation in this hospital, 5 (62.5 %) performed a chest CT scan and a bronchoscopy; chest CT scan was normal in 2 and showed ground-glass pattern in 3 patients; endobronchial abnormalities were not found in any patient. In the other 3 patients, diagnostic evaluation was performed only with a chest CT scan, showing abnormalities in 2 (1 with ground-glass pattern and 1 with a discrete linear opacity).
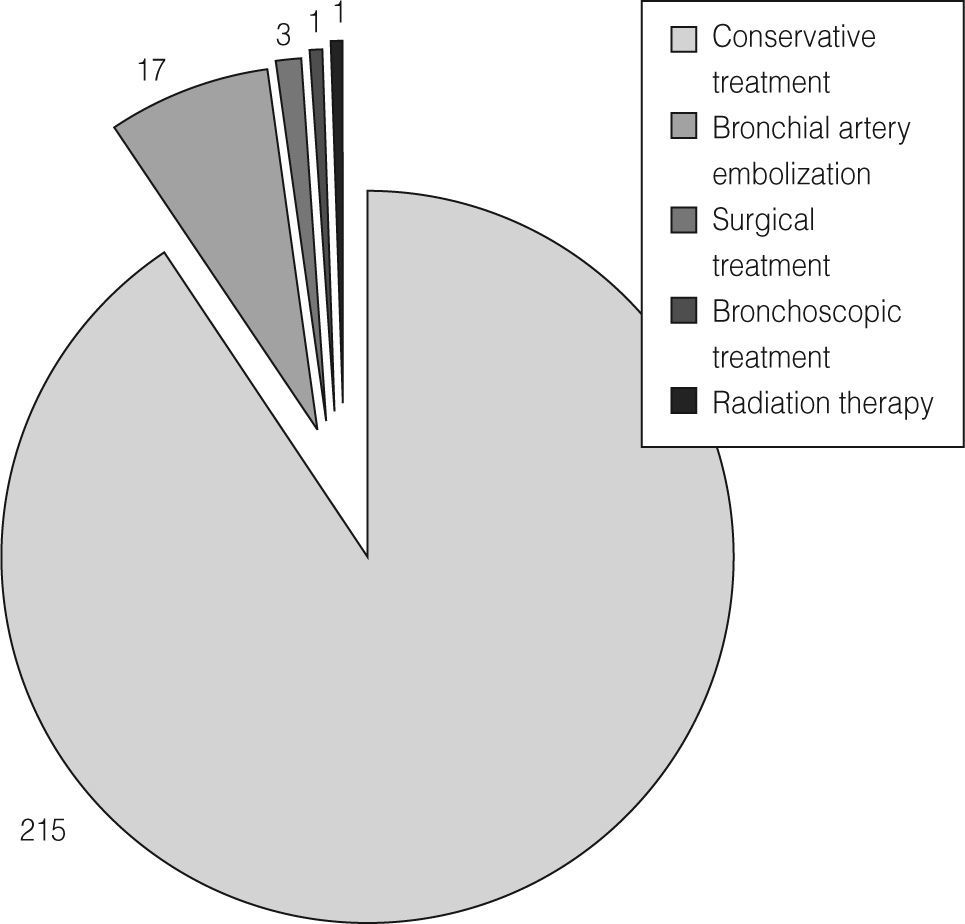
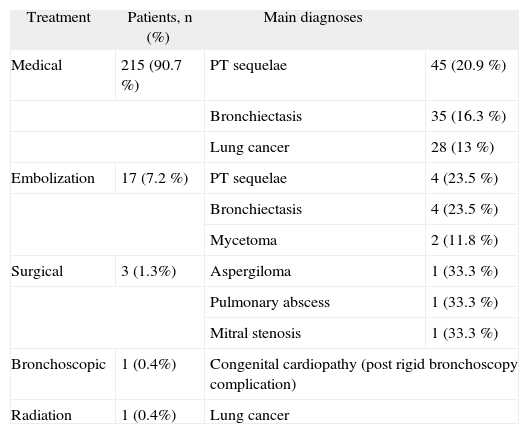
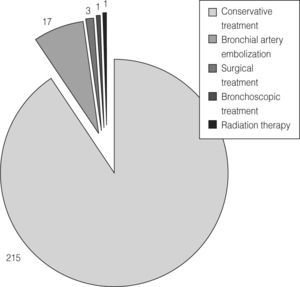
TreatmentMost patients went on medical treatment (90.7 %), as seen on Figure 3. Medical treatment was based, routinely, on the administration of antitussives (codeine) and antifibrinolytics (aminocaproic acid), and also morphine, in cases in which control of bleeding was not possible with medications previously described.
The main diagnoses, according to each therapeutic option, are listed in Table 5.
Main diagnoses found for each therapeutic option (n = 237)
| Treatment | Patients, n (%) | Main diagnoses | |
| Medical | 215 (90.7 %) | PT sequelae | 45 (20.9 %) |
| Bronchiectasis | 35 (16.3 %) | ||
| Lung cancer | 28 (13 %) | ||
| Embolization | 17 (7.2 %) | PT sequelae | 4 (23.5 %) |
| Bronchiectasis | 4 (23.5 %) | ||
| Mycetoma | 2 (11.8 %) | ||
| Surgical | 3 (1.3%) | Aspergiloma | 1 (33.3 %) |
| Pulmonary abscess | 1 (33.3 %) | ||
| Mitral stenosis | 1 (33.3 %) | ||
| Bronchoscopic | 1 (0.4%) | Congenital cardiopathy (post rigid bronchoscopy complication) | |
| Radiation | 1 (0.4%) | Lung cancer | |
Only 1 patient needed a bronchoscopic intervention - a 7-year-old child with a congenital cardiopathy. Control of bleeding was initially possible with medical treatment. However, a rigid bronchoscopy performed for replacement of a tracheal stent (the child also had a tracheal stenosis) was complicated by severe bleeding, which was controlled with tamponade.
Three patients (1.3 %) were submitted to a surgical intervention: lobectomy in a case of a pulmonary abscess; marsupialization of an aspergiloma cavity and replacement of mitral valve in a case of mitral stenosis.
In all 237 admissions, arteriography with bronchial artery embolization was performed in 7.2 %. During these 5 years, considering every admission of each patient, we found that 11.8 % of patients went on bronchial artery embolization. The main diagnoses of these patients were PT sequelae and bronchiectasis, followed by vascular abnormalities and mycetoma. The reasons for embolization were recurrence prevention in 60.7 % and control of bleeding in the others. When embolization was performed for recurrence prevention, the admission was programmed in 64.7 %.
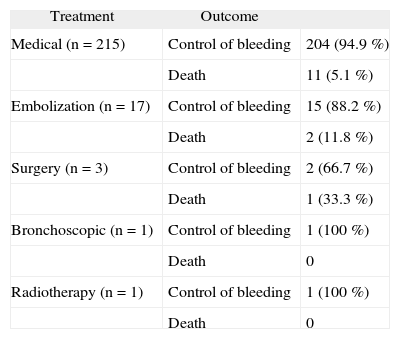
OutcomePatients’ outcome was favorable in 94.1 %, with hospital discharge after control of bleeding. Fourteen patients died (5.9 %). We found a higher mortality rate for all severity criteria (with statistical significance - p < 0.01), mainly hemodynamic instability with a mortality rate of 24 %. The main diagnoses in patients who died were lung cancer (5 patients - 35.7 %), bronchiectasis and pulmonary tuberculosis (2 patients each 14.3 %).
In Table 6 the outcomes for each therapeutic approach are listed.
Patients’ outcome according to each therapeutic option
| Treatment | Outcome | |
| Medical (n = 215) | Control of bleeding | 204 (94.9 %) |
| Death | 11 (5.1 %) | |
| Embolization (n = 17) | Control of bleeding | 15 (88.2 %) |
| Death | 2 (11.8 %) | |
| Surgery (n = 3) | Control of bleeding | 2 (66.7 %) |
| Death | 1 (33.3 %) | |
| Bronchoscopic (n = 1) | Control of bleeding | 1 (100 %) |
| Death | 0 | |
| Radiotherapy (n = 1) | Control of bleeding | 1 (100 %) |
| Death | 0 |
Pulmonary tuberculosis sequelae, bronchiectasis, lung cancer and pulmonary tuberculosis were the main diagnoses in the adult population studied. The importance of tuberculosis, active or previous, as a cause of hemoptysis, was the main difference compared to other studies, in developed countries.5–7 In fact, tuberculosis is still endemic in Portugal, although a significant decrease has occurred in recent years.8,9 Among malignancies, in most series, squamous cell carcinoma is the main responsible for hemoptysis.5,34 This histological type, due to its central localization, is more frequently associated with the occurrence of hemoptysis, compared to adenocarcinoma, which has usually a peripheral localization. However, in this study, adenocarcinoma was the main histological type. Two main reasons can explain this finding: a high number of malignancies without a full histological characterization and the higher prevalence of adenocarcinoma compared to squamous cell carcinoma, nowadays.35,36 In fact, in 5 patients (15.2 % of all patients with lung cancer), histological type was not found in the clinical file and 2 patients (6 %) were diagnosed with non-small cell lung cancer without further characterization.
By age group, it is notorious the increasing frequency of malignancies keeping pace with the increasing of age, in accordance with reviewed literature. 3 Smoking history, being the main established risk factor for lung cancer, is a fundamental clue in patients’ history. In this study, diagnoses of lung cancer in patients with a positive smoking history (current or former smokers) were more than twice as much as those without a smoking history.
Most patients with pulmonary tuberculosis were current smokers. In fact, recent studies have described an association between tobacco smoke and the risk of developing tuberculosis.37,38
In pediatric population, the main etiologies of hemoptysis (bronchiectasis and congenital cardiopathies) are in accordance with other studies.10,11 In Europe, cystic fibrosis is one of the main diseases that is responsible for the occurrence of hemoptysis.12 In this study, 1 child with bronchiectasis was diagnosed with this genetic disease.
Hemoptysis’ severity is classically classified based on the amount of bleeding. In this study, such a classification was not possible, because this type of information was absent in most clinical files. Nevertheless, severity criteria considered are inevitably associated with a higher amount of bleeding. Several authors sustain that hemoptysis’ severity should be based, not in the amount of bleeding, but in the magnitude of the clinical effect - clinical and analytic criteria that reflect a severe bleeding, necessity of transfusion, among others.39,40
In most series, massive hemoptysis constitute 5-23 % of all hemoptyses 4,19,41 and their mortality rate varies, from 23 to 75 %.4,41 In this study, hemodynamic instability occurred in 10.5 % of patients and was associated with a mortality rate of 24 %. Clinical criteria used in this study (reduction of hemoglobin concentration > 1g; respiratory failure and hemodynamic instability) were good indicators of severity, showing a statistically significant association with mortality.
The main diseases responsible for massive hemoptysis vary among series: bronchiectasis, pulmonary tuberculosis, lung cancer, bronchitis, pulmonary abscess, aspergiloma, among others.42 Some studies found that lung cancer was associated with a small bleeding.19,43 However, in this study, this diagnosis was the most frequent for all considered severity criteria.
Chest X-Ray, chest CT scan and bronchoscopy are the main diagnostic tests in etiologic investigation.6,14–16 Their use vary among series, with the exception of the almost universal use of chest X-Ray. It seems consensual that a higher probability of malignancy should be reflected in a more exhaustive diagnostic investigation.6,15,18,19 In this study, the finding of characteristics related to a higher risk of lung cancer was associated with the performance of bronchoscopy, in a statistically significant manner. This association was not found in chest CT scan. The performance of chest CT scan in this group of patients (81.4 %) was below to what was desirable. Several recent studies on the diagnostic impact of diagnostic tests suggest, as a protocol, the performance of chest X-Ray and chest CT scan in all patients with hemoptysis and bronchoscopic evaluation if there are risk factors for lung cancer, such as a smoking history.6,15
Diagnostic evaluation performed in this study is still far from what‘s suggested in such protocol. In fact, there was a low performance of chest CT scan (only 81.4 % of all). Among patients with a higher risk of lung cancer, chest CT scan was performed in 84.7 %, and chest CT scan plus bronchoscopy in only 62.2 %, far below the desirable 100 %. However, some of the patients included in this study had already had previous admissions for hemoptysis, and their diagnosis was already known - so, in these cases, there was a lower use of diagnostic tests.
Chest CT scan was the most sensitive diagnostic test when used alone. However, the combined use of chest CT scan together with a bronchoscopy had the best diagnostic yield. Both these results have already been described.19
In accordance with the experience of several authors,4,7 hemoptysis’ control was possible mainly through conservative measures. Literature validates the importance of bronchial artery embolization, either in the control of bleeding, or in recurrence prevention. The latter was the main reason for its performance in this study. Success rate in the control of bleeding was 72.7 %, below what‘s referred on other studies (85-99 %). 24–28 Some factors may have contributed to this, such as the small amount of patients (11), and their higher severity (54.5 % of patients had already had hemodynamic instability). Another factor that seems to limit the success rate in the control of bleeding is some postponement of embolization‘s performance. In fact, conservative measures are the initial therapeutic options and the advance to other therapies occurs when the first fails. This management may be justified for limited resources, such as trained teams for the procedure.
This study was not able to evaluate success rate of bronchial artery embolization about recurrence prevention.
ConclusionsNowadays, the main diseases responsible for hemoptysis are chronic infections sequelae and malignancies.
Hemodynamic instability and malignancy were associated with a bad prognosis.
Bronchial artery embolization has been used with an increasing frequency, and its efficacy has already been established in the control of bleeding.
This study and the review of literature on this subject highlighted the necessity of a greater uniformization in hemoptysis’ management. So, the elaboration of protocols in order to uniformize, either diagnostic approach, or therapeutic approach is important.
Conflict of interestAuthors state that they don‘t have any conflict of interest.