The assessment of respiratory function in preschool children, which has recently been attracting considerable interest, has several methodological particularities. Whether this is feasible in clinical practice with large groups of patients still needs to be investigated.
AimTo assess the feasibility of pulmonary function testing in preschool children in clinical practice, and report the degree of success achieved according to age.
MethodsRetrospective analysis of lung function tests performed in children from 2 to 6 years old at the respiratory function laboratory of CUF Descobertas Hospital between September 2006 and August 2011. Whole-body pletismography without occlusion for specific airway resistance (sRaw) assessment and animated spirometry were performed using the equipment Jaeger 4.65 (Viasys Healthcare), before and after 400μg of inhaled salbutamol via a spacer device. The research fulfilled international criteria (ATS/ERS) for acceptability and reproducibility.
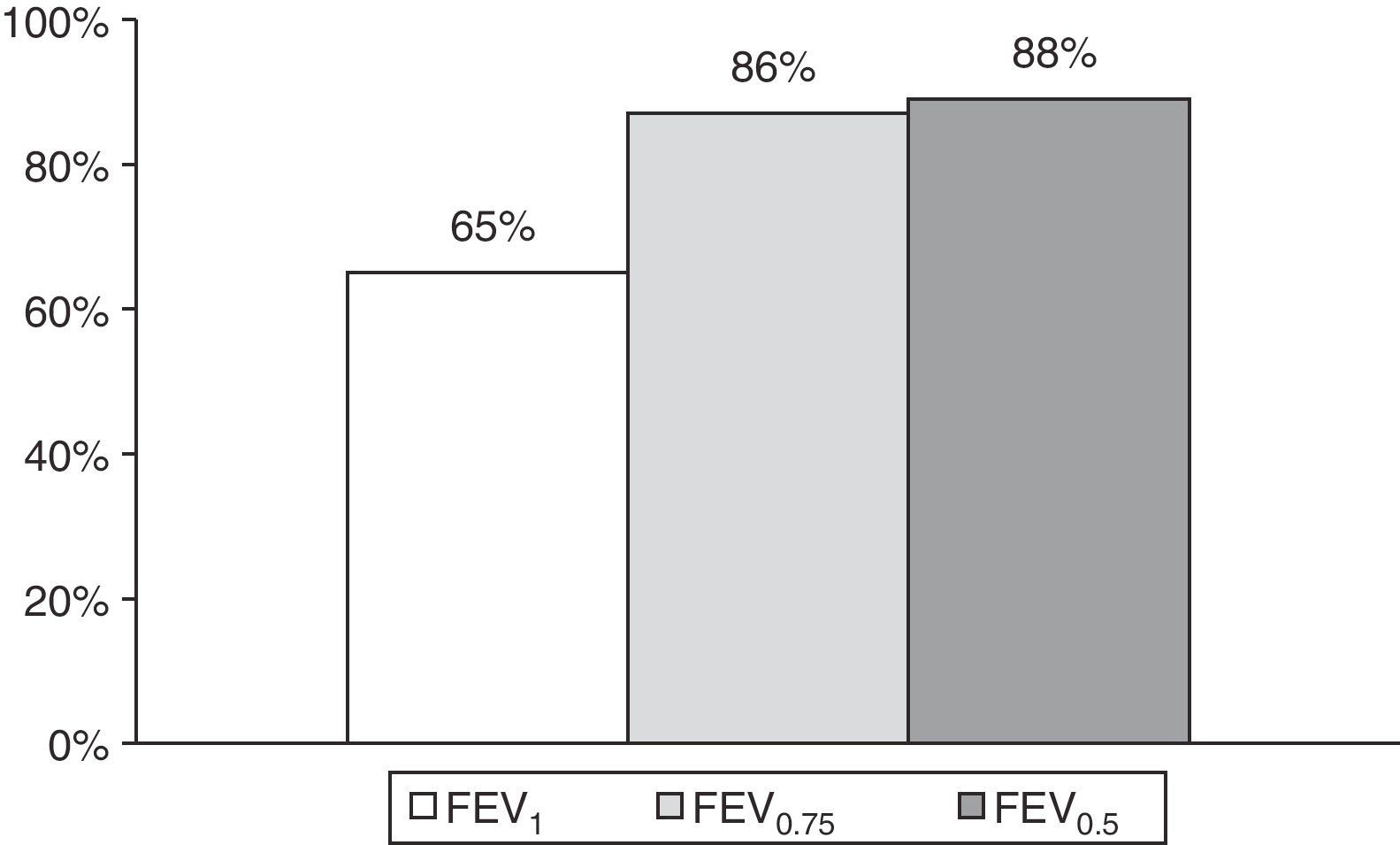
ResultsOf 1,239 lung function tests performed, 1,092 (88%) had acceptable and reproducible criteria for spirometry (children with a mean age of 4.3±0.91 years; 60.7% male), and 979 (79%) for sRaw measurement. We were able to report FEV1 in 801 (65%) tests (children with a mean age of 4.5±0.89 years). In 23 (2%) tests it was only possible to report FEV0.5 (children with a mean age of 3.5±0.67 years) and in 268 (22%) only FEV0.75 (children with a mean age of 4.0±0.89 years).
ConclusionSpirometry and sRaw assessment in preschool children can be used in clinical practice, with an increasing success rate as children get older. Reporting maneuvers of 0.5 or 0.75seconds facilitates spirometric evaluation in a larger number of children.
A avaliação da função respiratória em idade pré-escolar reveste-se de particularidades metodológicas, tendo ganho recentemente um interesse crescente. A sua exequibilidade na prática clínica, em grandes grupos de doentes, continua, no entanto, por investigar.
ObjetivoAvaliar a exequibilidade do estudo funcional respiratório em idade pré-escolar e o grau de sucesso de acordo com a idade.
MétodosAnálise retrospetiva de provas funcionais respiratórias realizadas em crianças com 2 a 6 anos no laboratório de exploração funcional respiratória do Hospital CUF Descobertas entre Setembro de 2006 e Agosto de 2011. Foi efetuada pletismografia corporal sem oclusão para avaliação da resistência específica das vias aéreas (sRaw) e espirometria animada, com equipamento Jaeger4.65 (VIASYS Healthcare) antes e após 400 ug de salbutamol inalado em câmara expansora. Foram cumpridos os critérios internacionais (ATS/ERS) para aceitabilidade e reprodutibilidade.
ResultadosDe 1 239 provas funcionais respiratórias realizadas, 1 092 (88%) tinham uma espirometria com critérios de aceitabilidade e reprodutibilidade (crianças com idade média de 4,3±0,91 anos; 60,7% do sexo masculino), e 979 (79%) sucesso na determinação de sRaw. Foi possível reportar FEV1 em 801 (65%) provas (crianças com idade média 4,5±0,89 anos). Em 23 (2%) das provas apenas foi possível reportar FEV0,5 (crianças com idade média de 3,5±0,67 anos) e em 268 (22%) apenas FEV0,75 (crianças com idade média de 4,0±0,89 anos).
ConclusãoA espirometria e a avaliação de resistências em idade pré-escolar são exequíveis na prática clínica diária, com um aumento do sucesso em crianças mais velhas. O registo de manobras com duração de 0,5 ou 0,75 s permite a avaliação funcional respiratória de um maior número de crianças.
Pulmonary function tests (PFT) are useful tools for objective quantification of pulmonary compromise, diagnosis confirmation, therapy monitoring and prognosis assessment of various respiratory diseases.1
In preschool children, given the difficulties of coordination and cooperation, as well as the inadequacy of adult criteria.2 PFT have previously been restricted to clinical research.
In this age group, it is not possible to measure static lung volumes, because children will not tolerate the valve closing. However, specific airway resistance (sRaw) can be obtained by measuring changes in airflow relative to changes in plethysmographic volume without having to breathe against a closed shutter3 and spirometry can be performed by experienced technicians using animated software in a friendly and comfortable environment, giving increased success rates in older preschool children.4
Recommendations for acceptability and reproducibility criteria in preschool children were published in 2007 by the American Thoracic Society (ATS) and European Respiratory Society (ERS)5, enabling the standardization of methods and practices, with reference equations now already available in this age group for spirometry6 and specific airway resistance (sRaw) evaluation7.
With this study, carried out in a specialized clinic, we aim to determine the feasibility of routine PFT with spirometry and plethysmography without occlusion, both before and after bronchodilation in preschool children, and the degree of success achieved according to age.
MethodsStudy design and populationRetrospective analysis of PFT performed in CUF Descobertas Hospital between September 2006 and August 2011. The children selected were between 2 to 6 years old, were followed at the allergy outpatient clinic due to asthma, recurrent wheezing or chronic cough, and referred by their doctor to the respiratory function laboratory of the same hospital. Children with respiratory infection or exacerbation of their respiratory symptoms in the preceding three weeks were not tested.
Pulmonary function testingPerformed before and 20minutes after administration of 400μg of inhaled salbutamol through a spacer device, using a MasterScreen Body Jaeger spirometer (v.4.65, CareFusion Ltd, Viasys Healthcare, Hoöchberg, Germany), calibrated daily according to manufacturer's instructions. All data was corrected for body temperature, pressure and saturation (BTPS).
The study took place in a friendly and comfortable environment, and was performed by an experienced technician. Results were obtained with the child sitting, using a mouthpiece and, preferentially, a nose clip.
First, sRaw measurements were obtained by body plethysmography without occlusion with the child sitting alone in the plethysmograph, their hands supporting their cheeks and encouraged to adopt a regular breathing rhythm with a respiratory rate between 30 and 45 cycles per minute. Respiratory rate was automatically displayed by the integrated software. The automatic computer selected tangent was used and the median trial of 3 technically acceptable sets of 5 to 10 breaths was reported. Curves were considered acceptable if breaths were super-imposable (i.e. parallel slopes), of similar size and shape, reasonably closed at zero flow and without obvious distortions to the breath (e.g. glottic closure, cough, talking).
Spirometry was performed using animation software, which kept the child motivated through positive reinforcement and training to progressively master the technique of forced expiratory maneuvers. A minimum of three and up to 15 maneuvers were obtained and recorded. The volume-time and flow-volume curves were visually inspected by at least two independent investigators. Only curves fulfilling the criteria for acceptability and reproducibility for preschool children published by the ATS/ERS5 were accepted. Curves obtained after bronchodilation were submitted to the same criteria as baseline curves.
Results were reported only if curves were obtained both before and after bronchodilation, for a maximum expiratory volume at time t (FEVt) with maneuver duration equal or higher than 0.5seconds.
Statistical analysisStatistical analysis was performed using the SPSS version 18.0 for Windows (SPSS, Chicago, IL, USA). The mean was used as a measure of central tendency and standard deviation as a measure of dispersion.
ResultsDuring the period studied, 1,239 PFT were performed.
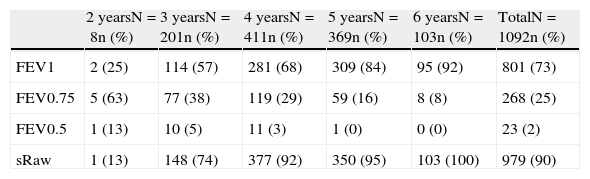
It was possible to obtain curves meeting acceptability and reproducibility criteria for spirometry in 1,092 (88%) tests (1,013 children with mean age of 4.3±0.91 years, of which 615 (60,7%) were male). Seventy nine (7.2%) tests were revaluations performed after a mean of 12.0±8.1 months. FEVt achieved according to children's age is shown in Table 1. In 23 (2%) tests it was only possible to report FEV0.5 and in 268 (22%) FEV0.75, allowing the reporting of spirometric parameters in more 291 (23%) PFT (Fig. 1). Measurements with reported FEV0.5 (children with mean age 3.5±0.67 years old) and FEV0.75 (children with mean age 4.0±0.84 years old), were obtained in younger children comparing to FEV1 (mean age 4.5±0.89 years old).
Feasibility of pulmonary function testing according to children's age.
| 2 yearsN=8n (%) | 3 yearsN=201n (%) | 4 yearsN=411n (%) | 5 yearsN=369n (%) | 6 yearsN=103n (%) | TotalN=1092n (%) | |
| FEV1 | 2 (25) | 114 (57) | 281 (68) | 309 (84) | 95 (92) | 801 (73) |
| FEV0.75 | 5 (63) | 77 (38) | 119 (29) | 59 (16) | 8 (8) | 268 (25) |
| FEV0.5 | 1 (13) | 10 (5) | 11 (3) | 1 (0) | 0 (0) | 23 (2) |
| sRaw | 1 (13) | 148 (74) | 377 (92) | 350 (95) | 103 (100) | 979 (90) |
sRaw: Specific airway resistance; FEVt: Forced expiratory volume in time t.
sRaw was reported in 979 (79%) tests (902 children with mean age of 4.4±0.87 years, of which 549 (60,9%) were male).
For both spirometry and sRaw evauation, there was an increased degree of success in older children (Table 1).
DiscussionPFT were requested in a large number of preschool children and performed with a high success rate.
Previously published papers have shown the feasibility of respiratory function testing in this age group, but were mostly based on tests performed in the context of clinical investigation and with a small number of patients.2,8
This study evaluated the PFT success rate in preschool children, both before and after bronchodilation, which is the daily practice of the respiratory function laboratory.
This was only possible because the physicians were aware of the technical specificities, and the importance of PFT in this age group, and by the fact that tests were performed by an experienced and specialized technician, consistently using the same methodology and equipment.
Studies that focus on this issue have reported success rates in spirometry that can reach 85%.2,8,9 With this study, we prove it is possible to achieve an even higher degree of success. As shown by other authors,2,8,9 reporting forced expiratory volumes of less than one second has considerably increased the number of PFT in which it was possible to obtain lung function parameters, especially in younger children, whereh determining FEV0.75 proved particularly useful.
Regarding to the sRaw evaluation, there have been reported success rates of around 75 to 80%,10 which coincides with our results. The feasibility of the technique has been considered to be age-dependent, which is confirmed in our study by the important decrease of success in sRaw determination in those aged 3 years or younger.
The improvement of spirometry and sRaw reporting in older children in our series is probably not due to learning effect of follow-up repeated measurements, since less than 10% of tests correspond to revaluations.
Thus, the high feasibility of lung function tests in children 2 to 6 years of age may increasingly allow their use in assessing preschool children with respiratory disease.
Studies conducted by Borrego et al11,12 demonstrated the reproducibility of these measurements over time, as well as functional differences depending on the clinical diagnosis in this age group, although more studies are necessary in the future to demonstrate its usefulness, particularly in clinical correlation and prospective follow-up of these children.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Santos, N; Exequibilidade do estudo funcional respiratório em idade pré-escolar na prática clínica. Rev Port Pneumol 2012. http://dx.doi.org/10.1016/j.rppneu.2012.09.004