Tobacco smoke is a risk factor for Chronic Obstructive Pulmonary Disease and a major public health problem. Prenatal maternal smoking and post-natal environmental tobacco smoke (ETS) lead to dose-dependent decrease in lung function and respiratory morbidity. Influence of different socioeconomic indicators and ETS in the home has also been suggested.
MethodsData on 313 children (52 % male) from 4 public schools in Lisbon was analyzed [1st (46 %) and 4th graders]. ETS assessment and respiratory symptoms were based on a self-answered questionnaire. All children performed standard spirometry in the school setting and 54 % were acceptable according to ATS/ERS criteria. Descriptive and bivariate analysis of the most relevant variables was done, followed by multiple logistic regression analysis adjusted to the variables with clinical/statistical relevance.
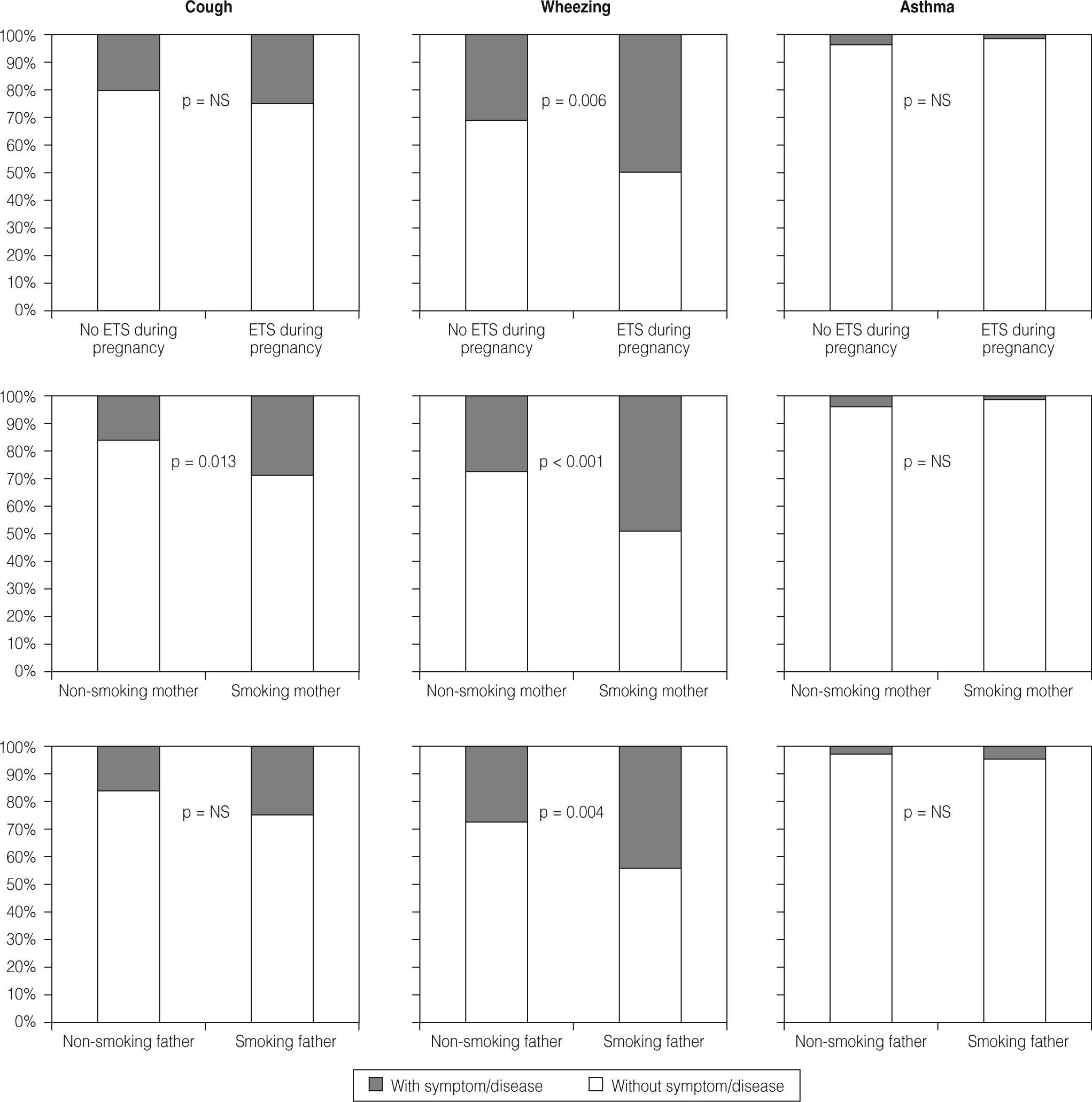
ResultsETS in the home was found in 41 % (maternal smoking during pregnancy 18 %, smoking mother 32 %, smoking father 38 %). Smoking fathers had lower education and less qualified occupation. Cough was more frequent in children with a smoking mother (adjusted OR=2.1; 95 %CI, 1.1–4) and wheezing in children with maternal smoking during pregnancy and smoking parents. All differences were significant (p<0.05). No association was found between parental education and cough/wheeze or ETS and respiratory infections/asthma/decreased spirometric values.
ConclusionsChildren in Lisbon are frequently exposed to ETS which results in significant respiratory morbidity. Targeted interventions must have social conditions in consideration. In this study, field spirometry was not helpful in early detection of lung function disability in children associated with ETS.
A exposição ao fumo do tabaco (EFT) é factor de risco para Doença Pulmonar Obstrutiva Crónica e um problema major de saúde pública. A EFT pré e/ou pós-natal determina redução precoce da função pulmonar e aumento da morbilidade respiratória, dependente da dose. Tem sido sugerido que a EFT domiciliária é influenciada por factores socio-económicos.
MétodosEstudo de rastreio epidemiológico transversal de dados de 313 crianças (52 % rapazes) de 4 Escolas Básicas de Lisboa [1° ano (54 %) e 4° ano]. A EFT e sintomatologia respiratória foram avaliadas a partir de questionário auto-preenchido pelos pais. Todas as crianças efectuaram espirometria na escola e 54 % foram consideradas aceitáveis de acordo com critérios ATS/ERS. Efectuou-se análise descritiva e bivariada das variáveis com maior interesse e análise de regressão logística múltipla ajustada para as variáveis com significado clínico/estatístico.
ResultadosEm 41 % dos casos a criança convivia com fumadores no domicílio (EFT na gravidez 18 %, mãe fumadora 32 %, pai fumador 38 %). Os pais fumadores tinham escolaridade inferior e ocupações menos qualificadas. Tosse foi mais frequente nas crianças com mãe fumadora (OR ajustado=2,1; 95 %CI, 1,1–4) e sibilância nas crianças com EFT na gravidez e com mãe/pai fumadores. Todas as diferenças foram significativas (p<0,05). Não se encontrou associação entre educação parental e sintomatologia respiratória ou ETF e infecções respiratórias/asma/ diminuição de valores espirométricos.
ConclusõesA EFT é frequente em crianças em idade escolar em Lisboa e condiciona morbilidade respiratória significativa. Intervenções dirigidas devem ter em conta condições sociais. Neste estudo a espirometria de campo foi pouco útil na detecção precoce de diminuição da função pulmonar em crianças associada à EFT.
Chronic obstructive pulmonary disease (COPD) remains a major public health problem. Tobacco smoking continues to be a major cause of COPD. A worldwide decline in tobacco smoking would result in substantial health benefits and a decrease in the prevalence of COPD and other smoking-related diseases. 1
Asthma and other wheezing disorders are among the most common childhood diseases. 2 Asthma is the leading cause of childhood morbidity, being the most common chronic disease of childhood 3 and in the last decades its prevalence has increased considerably worldwide, especially in western countries. 3–6 Various longitudinal studies 7–9 have contributed to the identification of risk factors associated with recurrent wheezing and asthma, enlightening the natural history obstructive respiratory diseases. Nevertheless, the relationship between lung function in childhood and asthma or adult COPD remains uncertain. The most relevant implicated factors are viral infections, secondhand tobacco smoke exposure and atopy, all with impact on the children's lung function. 8–10 It is thought, nowadays, that some of the factors responsible for adult COPD might and should be identified and prevented in the paediatric age. 11
In children, pre and postnatal ETS exposure constitutes a determinant factor in respiratory morbidity and early lung function reduction. 12–14 Various studies have demonstrated that ETS exposure adversely affects children's respiratory health diminishing lung growth and increasing the risk of infections and respiratory symptoms, including wheezing and asthma exacerbation. 13–18 It has been shown that, either in utero or postnatal ETS exposure influence the frequency of respiratory symptoms, existing a dose-dependent relationship between the dose of ETS (one or 2 smoking parents), the respiratory symptoms and the spirometric indices. 12,13,19 However, no level of exposure to secondhand smoke is safe. 18,20,21
Regarding the implementation of prevention strategies, smoke-free laws are cost-effective public health interventions that increase the perception of risk of ETS exposure and have the potential to change health behavior. 21 However, the primary source of ETS exposure for infants and children is the home, 20,22,23 and young children are especially vulnerable to ETS exposure. 23 Compared with adults, they have higher relative ventilation rates leading to higher internal exposures to ETS (as measured by urinary cotinine) for the same level of external exposure. 23 Even though we have laws, in Portugal, that protect non-smokers from ETS exposure in public and work places (Law .º37/2007, August 14th - effective from January 1st, 2008) there aren't any measures to protect children in their home, indicating that involuntary secondhand smoke exposure will persist and cause significant morbidity and mortality. The influence of socioeconomic factors on children's ETS exposure in the home, in determining respiratory disease, namely parental education, the social situation of the family (single parenting being a risk factor) and knowledge of the child's health status has been suggested by a number of studies. 17,24,25 A higher ETS exposure will increase the risk for respiratory disease amongst low-income families.
ObjectivesWe examined cross-sectional data from school age children to assess the relationship between ETS exposure (in utero exposure to maternal smoking and postnatal exposure) and parental education and occupation; the frequency of respiratory symptoms and infections; asthma and lung function in school-age children.
Study design, population and methodologyAn observational, cross-sectional study was done.
The population was selected from a group of children attending the 1st and 4th school-grades of 4 public basic schools belonging to the area of the Lumiar's Health Centre (Centro de Saúde do Lumiar). Parents gave written consent to the participation in the study, and the project was approved by the Ethics Committee of the Hospital de Santa Maria, Lisbon.
Clinical questionnaireA respiratory questionnaire in Portuguese was used, answered by the parents, adapted and translated to Portuguese from the American Thoracic Society's questionnaire. 26 The questionnaire includes the socio-economic-cultural history (parental education and occupation) environmental history (ETS exposure) and history of respiratory symptoms from birth. Parental occupation was classified in 9 categories according to a national classification of professions 27 and further grouped into qualified jobs (categories 1-3) and less/non-qualified jobs (categories 4-9). ETS exposure was defined as: smoking mother during pregnancy (ETS during pregnancy), smoking mother/father or ex-smokers after pregnancy (smoking mother/father) and living with smokers in the home (household smokers) including smokers in child's bedroom.
Respiratory disease was defined by the presence of the symptoms cough and wheeze. Pathological cough (symptom cough) was considered if it occurred without respiratory infections, after exercise and while the child played or laughed; and wheezing (symptom wheeze) if it occurred with or without respiratory infections, after exercise and while the child played or laughed and if bronchodilator therapy was used for symptom relief. Asthma was considered if an affirmative answer was given to the following questions: “has any doctor diagnosed your child with asthma?” and “has your son/daughter ever had asthma?”.
Anthropometric determination and lung function indicesWeight and length were measured and a brief physical examination (respiratory rate, pulmonary auscultation and assessment of the pulse oxymetry) of every child was done at the day of the study. For the obesity assessment [body mass index (BMI) > 95th percentile for age and sex] we used the BMI growthcharts built by the National Centre for Health Statistics (NCHS) and Centre for Disease and Control and Prevention in 2000. 28
All children performed standard spirometry 29 in the school setting using an apparatus with a digital volume transducer (MicroLab Spiro V1.34 - Micro Medical Ltd.). For the acceptable curves, the absolute values were selected and a data base was assembled using Excel (MSExcel 2007©). Using the reference values 30 created at UCL, Institute of Child Health, London (www.growinglungs.org.uk), the percentage predicted value (%P) and z-scores of the spirometric indices were automatically calculated (only values of %P were considered in this paper). It was considered normal: %P FEV1 and FVC 80-120 %P, FEV1/FVC ratio > 85 % and %P FEF25-75 ≥ 60 %.
Statistical analysisQuantitative variables were described by mean, median, standard deviation (SD) minimum and maximum. Qualitative variables are summarized through frequency/contingency tables as counts (n) and percentages (%). In cases where the responses had missing values, we classified them as unknown. A descriptive analysis of all the variables relevant to the study was performed, namely socio-demographic characteristics, family history, environmental factors (ETS exposure), past medical history, occurrence of respiratory symptoms (cough and wheezing), asthma diagnosis, physical examination and spirometry results.
A bivariate analysis was performed between some demographic data (gender, age and ethnicity), school, family history, environmental factors, past medical history and physical examination and dependent variables, namely respiratory symptoms (cough and wheezing), asthma and spirometric indices. For this analysis, Chi-Square/Exact Fisher tests (association between categorical variables) and t-Student/Mann-Whitney U tests (to compare a quantitative variable between two independent groups) were performed. In this analysis, the spirometric results (% P FEV1, FEV1/FVC and FEF25-75) were classified as “normal” if the values were within the normal range and “abnormal” if outside that range.
A multiple regression analysis was then performed for the dependent variables related to respiratory symptoms (cough and wheeze) and asthma with the independent variables that showed clinical and/or statistical significant values in the bivariate analysis. The magnitude of the association with the dependent variables was quantified using odds ratios (OR) and 95 % confidence intervals. The multiple regression models were tested by the likelihood ratio, the model goodness of fit was also evaluated using the Hosmer and Lemeshow test and area under the ROC (Receiver Operating Characteristic) curve.
The association of ETS exposure and spirometric indices was also analysed. The spirometric results were considered as categorical and numerical (using the respective units of %P values).
All tests were two-sided considering a significance level of 5 %. The statistical analysis was done using SPSS® (Statistical Package for Social Sciences) version 13.0 for Windows (SPSS Inc., Chicago) (See online supplement for more details on the population and spirometry execution).
ResultsGlobal response rate to the questionnaires was 62 % (313/509 children).
Demographic, social and anthropometric characteristicsOf the children enrolled in the study, 163 (52 %) were male, 143 (46 %) attended 1st grade (ages between 5 to 7 years) and the remainder attended 4th grade (n = 170, 54 %) (8-13 years). In 85 % of the cases (n = 262) the questionnaire was answered by the mother and in 10 % by the father (n = 30). The mother's median (range) age was 37 (23-49) years and the father's 39 (24-58). On average, parents mentioned approximately 12 years of education (for 23 mothers and 50 fathers the answer was unknown), 57 % of the mothers and 58 % of the fathers had a qualified occupation (groups 1-3) (unknown 93 and 94 respectively).
Past history and symptomsAllergy/atopy was present in at least one first degree relative (mother, father, sibling or half-sibling) in 72 children (24 %, unknown 13), rhinitis in 82 (27 %, unknown 11) and asthma in 64 (21 %, unknown 12). Children had on average one sibling and the vast majority attended day-care during infancy (n = 263, 96 %, unknown 39). Only one third of the children had pets at home (n = 99, 32 %), 49 (16 %) had a dog, 20 (7 %) had a cat (unknown 4). In the previous medical history, 43 % (n = 127) reported upper and 32 % (n = 97) lower respiratory infections (unknown 15). Cough during respiratory infections or rhinitis occurred in 222 children (72 %, unknown 6), cough without infections (pathologic cough) occurred in 64 children (21 %) and wheezing in 104 children (33 %) [53 children (18 %) had ≥ 2 wheezing episodes]. Asthma was considered in 11 children (4 %).
Lung functionRegarding the spirograms, 169 were considered acceptable (54 %). Of these, 21 children (12 %) had lower than normal % predicted (%P) FEV1 (average 99.1 %, range 54.5 %-146 %), 21 (12 %) had lower %P FVC (average 99.5 %, range 67.7-146.9 %), 4 (2.4 %) had a low %P FEV1/FVC (average 99 %, range 82.1-110.1 %) and 7 (5 % of 148 acceptable spirografic curves) presented low %P FEF25-75.
ETS exposureWe found 101 children (34 %) exposed to ETS at home and 36 children (12 %) usually exposed to ETS outside their homes (unknown 13-15) (Table 1).
ETS exposure (n = 313)
| ETS exposure | n = 313 | Unknown |
| ETS exposure during pregnancy | 57 (18 %) | 2 |
| Smoking mother | 98 (32 %) | 4 |
| Smoking father | 112 (38 %) | 14 |
| Household smokers | 117 (40 %) | 21 |
| Total number of household smokers | ||
| 1 | 83 (28 %) | 21 |
| 2 | 32 (11%) | |
| ≥ 3 | 2 (0.6%) | |
| Smokers in child's bedroom | 6 (2 %) | 10 |
Figures are shown as absolute numbers and (percentage).
There was no association between parental age or education and the occurrence of respiratory symptoms (cough and wheeze) or asthma in the children.
We found no association between ETS and maternal or paternal age, or maternal education and occupation. However, smoking fathers had lower education level, as assessed by median years of schooling (9 years vs 17 years, p < 0.001) and less qualified occupation, with a larger percentage of fathers with less/non-qualified jobs (categories 4-9) (58.5 % vs 41.3 %, p < 0.001) (Table 2, see online supplementary data in Appendix).
Association between smoking fathers and socioeconomic factors (fathers’ age, education and occupation)
We found an association between ETS exposure and the occurrence of respiratory symptoms and/or asthma: i) the percentage of children with cough was larger in the children whose mothers smoked (29 % vs 17 %, p = 0.013); and ii) the percentage of children with wheezing was bigger in the children exposed to ETS during pregnancy, and in children whose mothers and fathers smoked (51 % vs 31 %, p = 0.006; 49 % vs 28 % p < 0.001; and 45 % vs 28 %, p = 0.004 correspondingly) (Figure 1). In the multiple logistic regression analysis, children whose mothers smoked were 2.1 times more likely to have cough than children with non-smoking mothers (adjusted OR = 2.15; 95 %CI, 1.15-4.03; p = 0.017).
Respiratory infections (acute otitis media and lower respiratory infection) were more frequent in children whose mothers and/or fathers smoked but at a non-significant level. We found no association between ETS exposure and lower lung function (evaluated by %P FEV1 FEV1/FVC and FEF25-75).
Discussion and conclusionsETS exposure is frequent in school-aged children in Lisbon, and is similar to levels described in other countries 17,31,32 and in other regions of Portugal. 33 We found a significant association between ETS exposure and respiratory symptoms (cough and wheeze) but not respiratory infections or asthma diagnosis. Prevalence studies in school-age children suggest that respiratory infections, wheezing and asthma diagnosis are more frequent in children whose parents smoke. 15,16,18 The fact that we did not find a relation between ETS exposure and asthma leads us to speculate that this condition might be under-diagnosed, since one third of the children experienced wheezing (about 20 % had ≥ 2 episodes of wheezing) but only 4 % had an asthma diagnosis.
Concerning ETS exposure and lung function, most studies, but not all, have shown an association between ETS exposure, respiratory symptoms and decreased lung function. 12,16,18,22 The majority revealed diminished lung function associated with ETS exposure during pregnancy (smoking mothers during pregnancy), especially for small airway flows. 14,17,34 In our study, field spirometry was not helpful in the early detection of lung function disability in children associated with ETS exposure. However, only about half of the field spirometry measurements were considered acceptable and in another clinical setting, spirometry has proven not to be sensitive enough for the early detection of small airway compromise. 35
Regarding the percentage of smoking mothers, this was slightly larger than that publicized in a study in the north region of Portugal. 33 Nevertheless, this difference probably reflects the tobacco consumption by the Portuguese population. 36 According to the 2005-2006 National Health Survey, the highest rate of regular smoking in women corresponded to the Lisbon and Tagus Valley region. 36 In our study, smoking fathers had less years of education and less qualified occupation, similarly to what has been described in other studies. 17,25 These findings suggest that parental education is important in the prevention of ETS exposure and its consequences. It has been suggested that health-risk awareness by the parents, regarding potential hazards of childhood ETS exposure, can significantly reduce ETS exposure to children. 17,37
Our study has some limitations. Asthma status was assigned on the basis of parental reports of a physician diagnosis of asthma, and respiratory infections and symptoms based on parental recall. Exposure to tobacco smoke was assessed retrospectively, using questionnaire responses, and was not validated by objective measurements. We were unable to investigate any dose-response relationships because we lacked information on the intensity or duration of exposure.
However, our findings have clinical and public health significance. The long-term effects of exposure to smoking on the growing lungs of children are of particular concern. Since the primary source of childhood ETS exposure is the home, 23 Health Public policies concerning tobacco smoke must not only alert the parents for the increased morbidity caused by childhood ETS exposure but also develop strategies to diminish tobacco smoke in the home environment. ETS awareness and control strategies for the home should also be incorporated into mandatory tobacco education programmes in schools. 23 Other appropriate measures include the elimination of smoking in all forms of transportation used by children and in all public places where children are present. 18 Evaluation and monitoring of these programmes is crucial to any strategy to diminish ETS exposure and self-reported data need to be supplemented by objective monitoring systems. 23
In conclusion, we found that childhood ETS exposure is frequent and is related with parental education level and profession and with respiratory symptoms as assessed by respiratory questionnaires. One of the most important challenges for the future is the development of effective preventive measures that are suitable to different cultures and socio-economic groups. Tobacco consumption prevention strategies, to put into practice in our country, cannot disregard the differences in consumption amongst the diverse regions of Portugal. Population-level tobacco control interventions have the potential to benefit more disadvantaged groups and thereby contribute to reducing health inequalities. 38 Given that children are especially vulnerable to the hazard effects of ETS, pregnant women and parents of young children must be a preferential target for intervention.
Conflict of interestAuthors state that they don't have any conflict of interest.
Dr Cristina Bastardo for her support in the reading and evaluation of the spirograms, Pulmocor for loaning us the spirometer, MSD (Dr Fátima Afonso) for her assistance in photocopying the questionnaires, the Scholar Health team from the Lumiar's Health Centre, children, families, the Schools’ teachers and directors (EB Alto da Faia, EB 57 Telheiras, EB 91 Bairro da Cruz Vermelha, EB31 Prof Lindley Cintra) for their collaboration.
This Clinical Research Project - “Screening of Respiratory Disease in School-age Children” - Carolina Constant, Isabel Sampaio, Ana Margarida Silva, Marisa Salgueiro, Teresa Bandeira, was awarded a scholarship for young practionners in the Hospital de Santa Maria in 2007.
Suplementary data associated with this article can be found in the online version at www.elsevier.org/rpp