The purpose of this study was to evaluate the correlations within pulmonary function, functional capacity, and posture in adult patients with cystic fibrosis (CF). A secondary aim was to evaluate the correlation between patient quality of life and postural assessment variables.
MethodA cross-sectional study was conducted on fourteen patients with CF. Patients were subjected to a postural analysis (postural assessment software) and measurements of pulmonary function (spirometry, whole body plethysmography, and carbon monoxide diffusing capacity) and functional capacity (6-min walking test). All patients completed the Cystic Fibrosis Questionnaire-Revised (CFQ-R).
ResultsMost patients were male (57%), and the median age of the patients was 24.5 (22–34). The forced expiratory volume in one second, the 6-min walking distance, total lung capacity, and airway resistance were significantly correlated with the vertical alignment of the chest (ρ = −0.57, P < 0.05; ρ = −0.65, P < 0.01; ρ = 0.54, P < 0.05; and ρ = 0.67, P < 0.01, respectively). The ‘physical’ domain of the CFQ-R was significantly correlated with the vertical alignment of the chest (ρ = −0.74, P < 0.01), and the ‘limitations’ domain of the CFQ-R was significantly correlated with the angle of the hip (ρ = −0.55, P < 0.05).
ConclusionThe present study shows that abnormalities in pulmonary function and functional capacity are associated with postural changes in adults with CF. However the severity of the postural abnormalities does not negatively influence the CFQ-R domains.
Avaliar as correlações entre função pulmonar, capacidade funcional e postura em pacientes adultos portadores de fibrose quística (FQ). Como segundo objetivo, avaliar a correlação entre a qualidade de vida e as variáveis obtidas na avaliação postural destes pacientes.
MétodosFoi realizado um estudo transversal em que 14 portadores de FQ se submeteram à avaliação da análise postural (software de avaliação postural) e provas de função pulmonar (espirometria, pletismografia de corpo inteiro e medição da capacidade de difusão do CO) e capacidade funcional (teste da caminhada de 6min). Todos os pacientes responderam ao Questionário de Fibrose Quística com Versão Revisada (QFQ-R).
ResultadosA maioria dos pacientes era do sexo masculino (57%), com mediana da idade de 24,5 anos (22-34 anos). Foram observadas correlações significantes de volume expiratório máximo no primeiro segundo, distância da caminhada dos 6 min, capacidade pulmonar total e resistência de vias aéreas com o alinhamento vertical do tronco (ρ = −0,57, p < 0,05; ρ = −0,65, p < 0,01; ρ = 0,54, p < 0,05; e ρ = 0,67, p < 0,01, respetivamente). Foram observadas correlações estatisticamente significantes entre o domínio «físico» do QFQ-R e o alinhamento vertical do tórax (ρ = −0,74, p < 0,01), e entre o domínio «limitações» do QFQ-R e o ângulo do quadril (ρ = −0,55, p < 0,05).
ConclusõesO presente trabalho mostra que as anormalidades na função pulmonar e na capacidade funcional se associam às alterações posturais em adultos portadores de FQ. Entretanto, a gravidade das anormalidades posturais não influenciam negativamente os domínios do QFQ-R.
Cystic fibrosis (CF) is an autosomal recessive disease that affects the functioning of various organ and body systems.1 The median estimated survival age for patients with CF has increased substantially over recent decades and is currently estimated at 38 years in most developing countries.2 Factors including early diagnosis, multidisciplinary management in specialised centres, and access to appropriate therapy have contributed to this change.3
The primary clinical consequences of CF are related to respiratory tract impairment, in which thick infected secretions trigger chronic inflammation. Pulmonary function decreases exponentially as patients get older, which results in significant airway obstruction leading to hyperinflation, and air trapping.4 An estimated 90% of patients die due to the progression of pulmonary disease.5 In addition to pulmonary impairment, CF causes significant changes in other organs and systems that can lead to major physical limitations. Compared to the paediatric population, adults with CF show a higher prevalence of skeletal muscle dysfunction, nutritional depletion, diabetes, and depression. Osteoporosis, bone fractures, and joint impairments are common in this group of patients.3
Posture is defined as the balanced arrangement of body structures and is determined by measuring the positioning of the body segments at a particular moment.6 In normal postural alignment, muscles and joints are expected to be in a state of equilibrium that involves the least amount of effort and overload.7 The postural attitude of the hyperinflated thorax can lead to a series of spinal column, shoulder, and pelvic girdle compensations. Spinal column deformities, such as increased thoracic kyphosis and lumbar lordosis, are common in adults with CF.8,9
The biomechanics of the rib cage influence overall body mechanics. Therefore, any respiratory imbalance will result in altered total body posture and balance.10 As lung disease progresses in CF patients, it is possible that hyperinflation and increased effort of breathing causes a general muscle imbalance because of the altered mechanics of respiration.11 It is therefore possible to assume that these changes culminate in a reduction of functional capacity. As this knowledge could be important for planning the most appropriate mode of therapeutic exercise in CF patients we looked to evaluate the correlations within pulmonary function, functional capacity, and posture in adult patients with CF. A secondary aim was to evaluate the correlation between patients’ quality of life (QL) and postural assessment variables.
MethodsPatientsA cross-sectional study was conducted in outpatients who were diagnosed with CF. The patients originated from the Piquet Carneiro Polyclinic at the State University of Rio de Janeiro and were assessed between September 2011 and February 2012. Adult patients (aged 18 years or older) were included if they had clinical and laboratorial diagnosis of CF (sweat test and/or deoxyribonucleic acid - DNA mutation analysis). Exclusion criteria included: inability to perform the pulmonary function tests or the 6-min walking test (6MWT); neurological, cardiovascular, metabolic, rheumatic or vestibular diseases; acute chest pain, recent history of hemoptysis, pneumothorax at least one year before the study; and respiratory infection in the four weeks preceding the study. Following ethical guidelines, patients were informed of the aims of the study and provided their informed consent before they participated. The protocol was approved by the Research Ethics Committee of the Augusto Motta University under protocol number 010/11.
MeasurementsAll patients completed the Cystic Fibrosis Questionnaire-Revised (CFQ-R).12 This tool was used to assess the following domains: physical, limitations, social, body image, and respiratory. The scores for each domain ranged from 0 to 100, with higher scores indicating a better QL. Scores above 50 are generally considered to reflect a good QL.11
A postural analysis was performed using postural assessment software (PAS) that was developed by researchers at the University of São Paulo and is available free (www.sapo.incubadora.fapesp.br).14 Photographs were taken using coordinates of anatomical points that were marked with passive markers (polystyrene balls with double-sided tape). The following anatomical points were identified: the right and left tragus, the right and left acromion, the right and left anterior superior iliac spine, the greater trochanter of the right and left femurs, the tuberosity of the right and left tibiae, the right and left lateral malleolus, and the spinous process of the seventh cervical vertebra.
Using a Collins Plus Pulmonary Function Testing Systems (Warren E. Collins, Inc., Braintree, MA, USA), the following exams were performed: spirometry, body plethysmography, and measurement of diffusing capacity for carbon monoxide (DLco). The tests followed the American Thoracic Society (ATS) standards.15 Equations described by Pereira (spirometry) and Neder (pulmonary volumes and diffusion) were adopted for the interpretation of the functional parameters.16–18 The 6MWT was performed in the same location in a 30-metre corridor. Each patient's predicted values were calculated using the equations described by Gibbons et al.19 and following the ATS recommendations.20
Data were presented as medians and interquartile ranges (25% and 75% percentiles) or frequencies (percentages). Because the variables formed a non-normal distribution according to the Shapiro-Wilk test, Spearman's test was used to study correlation. The analyses were performed using SAS 6.11 software (SAS Institute, Inc., Cary, NC, USA). Statistical significance was considered for P<0.05.
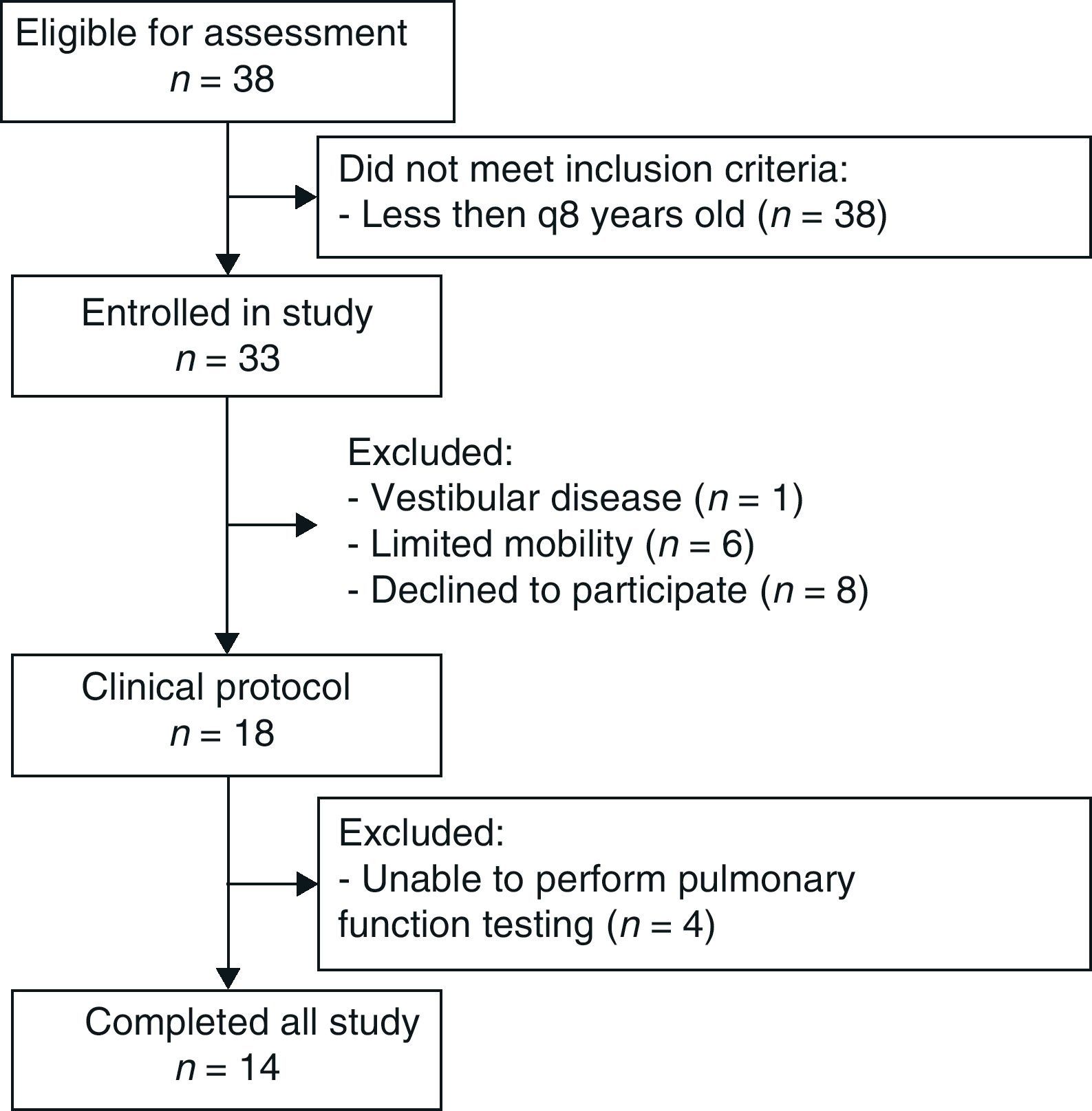
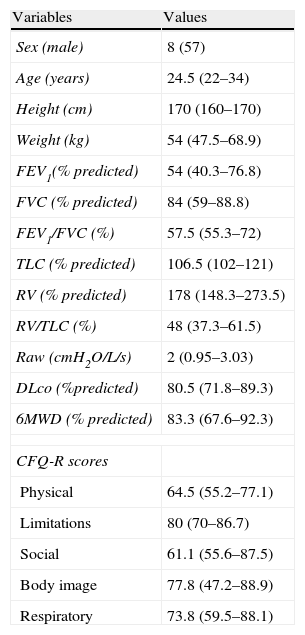
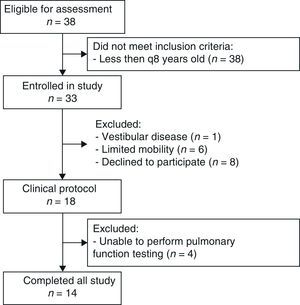
ResultsOf the 38 patients eligible for evaluation, 14 completed the study (Fig. 1). Anthropometric data, pulmonary function, functional capacity, and quality of life questionnaire domains are shown in Table 1. The median distance on the 6MWT was 636.5 m (range: 450–750 m), while the median percentage of Gibbons et al.’s prediction for this distance was 83.3 (67.6–92.3). Data from the postural assessment are presented in Table 2.
Anthropometric data, pulmonary function, functional capacity, and Cystic Fibrosis Questionnaire-Revised domains in patients with cystic fibrosis.
| Variables | Values |
| Sex (male) | 8 (57) |
| Age (years) | 24.5 (22–34) |
| Height (cm) | 170 (160–170) |
| Weight (kg) | 54 (47.5–68.9) |
| FEV1(% predicted) | 54 (40.3–76.8) |
| FVC (% predicted) | 84 (59–88.8) |
| FEV1/FVC (%) | 57.5 (55.3–72) |
| TLC (% predicted) | 106.5 (102–121) |
| RV (% predicted) | 178 (148.3–273.5) |
| RV/TLC (%) | 48 (37.3–61.5) |
| Raw (cmH2O/L/s) | 2 (0.95–3.03) |
| DLco (%predicted) | 80.5 (71.8–89.3) |
| 6MWD (% predicted) | 83.3 (67.6–92.3) |
| CFQ-R scores | |
| Physical | 64.5 (55.2–77.1) |
| Limitations | 80 (70–86.7) |
| Social | 61.1 (55.6–87.5) |
| Body image | 77.8 (47.2–88.9) |
| Respiratory | 73.8 (59.5–88.1) |
Results expressed as median (interquartile range) or number (%).
FEV1: forced expiratory volume in one second; FVC: forced vital capacity; TLC: total lung capacity; RV: residual volume; Raw: airway resistance; DLco: carbon monoxide diffusing capacity; 6MWD: 6-min walking distance; CFQ-R: Cystic Fibrosis Questionnaire Revised.
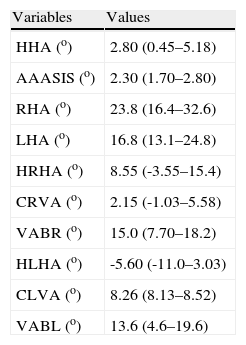
Postural assessment software data on patients with cystic fibrosis.
| Variables | Values |
| HHA (o) | 2.80 (0.45–5.18) |
| AAASIS (o) | 2.30 (1.70–2.80) |
| RHA (o) | 23.8 (16.4–32.6) |
| LHA (o) | 16.8 (13.1–24.8) |
| HRHA (o) | 8.55 (-3.55–15.4) |
| CRVA (o) | 2.15 (-1.03–5.58) |
| VABR (o) | 15.0 (7.70–18.2) |
| HLHA (o) | -5.60 (-11.0–3.03) |
| CLVA (o) | 8.26 (8.13–8.52) |
| VABL (o) | 13.6 (4.6–19.6) |
Results expressed as median (interquartile range).
HHA: head - horizontal alignment; AAASIS: angle between acromion and anterior-superior iliac spine; RHA: right hip - angle; LHA: left hip - angle; HRHA: head (right) - horizontal alignment; CRVA: chest (right) - vertical alignment; VABR: vertical alignment of the body (right); HLHA: head (left) - horizontal alignment; CLVA: chest (left) - vertical alignment; VABL: vertical alignment of the body (left).
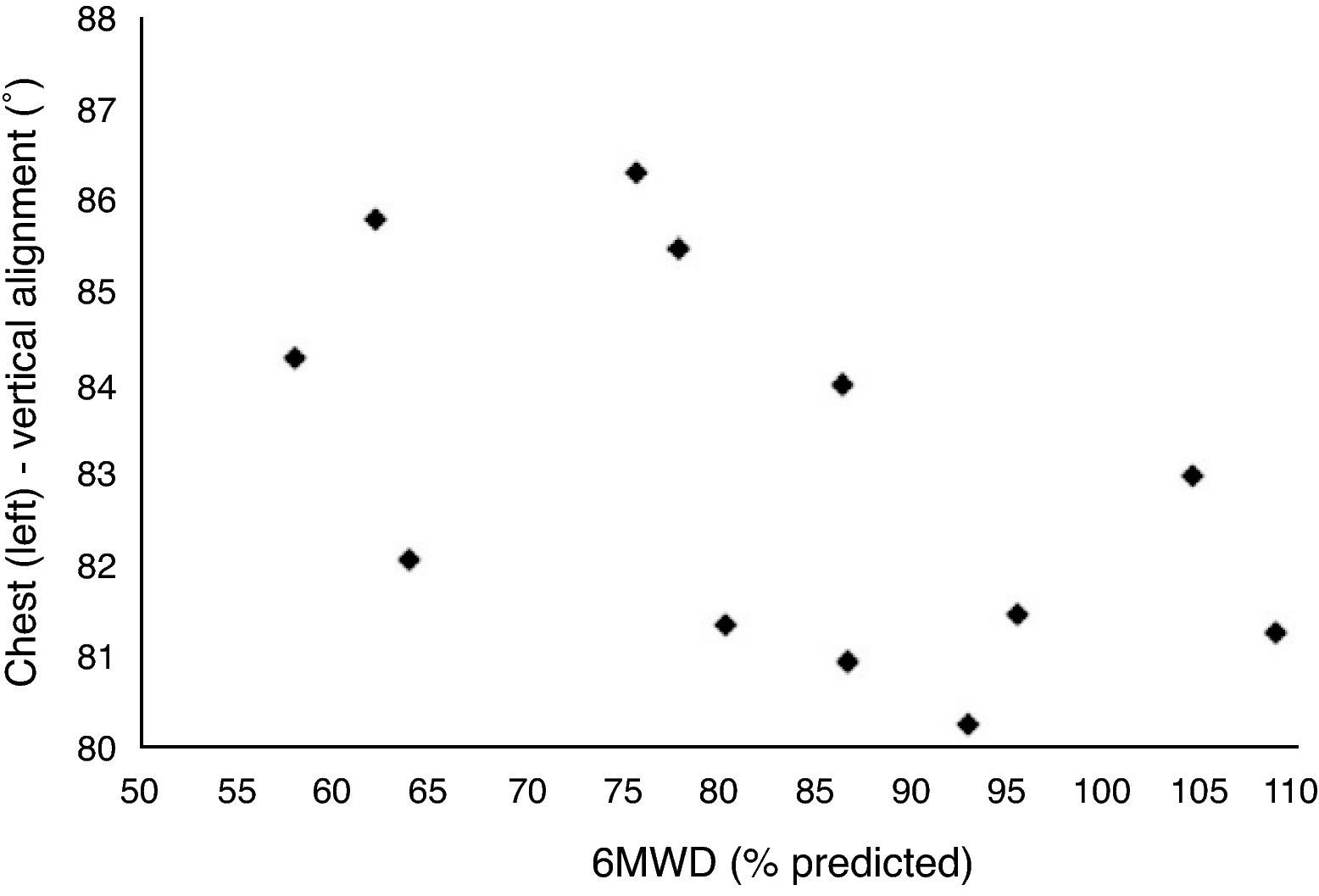
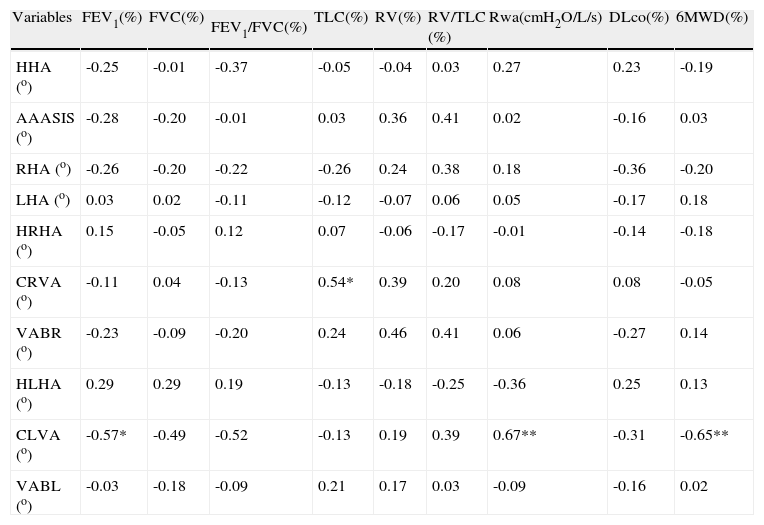
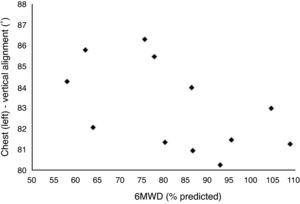
There were only two significant correlations among postural assessment data and the QL questionnaire. These correlations were between the ‘physical’ domain of the CFQ-R and the vertical alignment of the chest (right lateral view) (ρ=-0.74, P<0.01), and between the ‘limitations’ domain of the CFQ-R and the angle of the left hip (ρ=-0.55, P<0.05). Correlations between the postural assessment data and the pulmonary function and functional capacity variables are shown in Table 3 and Fig. 2. The forced expiratory volume in one second (FEV1) and the 6-min walking distance (6MWD) showed statistically significant negative correlations with the vertical alignment of the chest (left lateral view). Statistically significant positive correlations were noted between the total lung capacity (TLC) and the vertical alignment of the chest (right lateral view) and between airway resistance (Raw) and the vertical alignment of the chest (left lateral view).
Spearman's correlation coefficients between postural assessment software data and pulmonary function and functional capacity variables in patients with cystic fibrosis.
| Variables | FEV1(%) | FVC(%) | FEV1/FVC(%) | TLC(%) | RV(%) | RV/TLC (%) | Rwa(cmH2O/L/s) | DLco(%) | 6MWD(%) |
| HHA (o) | -0.25 | -0.01 | -0.37 | -0.05 | -0.04 | 0.03 | 0.27 | 0.23 | -0.19 |
| AAASIS (o) | -0.28 | -0.20 | -0.01 | 0.03 | 0.36 | 0.41 | 0.02 | -0.16 | 0.03 |
| RHA (o) | -0.26 | -0.20 | -0.22 | -0.26 | 0.24 | 0.38 | 0.18 | -0.36 | -0.20 |
| LHA (o) | 0.03 | 0.02 | -0.11 | -0.12 | -0.07 | 0.06 | 0.05 | -0.17 | 0.18 |
| HRHA (o) | 0.15 | -0.05 | 0.12 | 0.07 | -0.06 | -0.17 | -0.01 | -0.14 | -0.18 |
| CRVA (o) | -0.11 | 0.04 | -0.13 | 0.54* | 0.39 | 0.20 | 0.08 | 0.08 | -0.05 |
| VABR (o) | -0.23 | -0.09 | -0.20 | 0.24 | 0.46 | 0.41 | 0.06 | -0.27 | 0.14 |
| HLHA (o) | 0.29 | 0.29 | 0.19 | -0.13 | -0.18 | -0.25 | -0.36 | 0.25 | 0.13 |
| CLVA (o) | -0.57* | -0.49 | -0.52 | -0.13 | 0.19 | 0.39 | 0.67** | -0.31 | -0.65** |
| VABL (o) | -0.03 | -0.18 | -0.09 | 0.21 | 0.17 | 0.03 | -0.09 | -0.16 | 0.02 |
* P<0.05; ** P<0.01.
FEV1: forced expiratory volume in one second; FVC: forced vital capacity; TLC: total lung capacity; RV: residual volume; Raw: airway resistance; DLco: carbon monoxide diffusing capacity; 6MWD: 6-min walking distance; HHA: head - horizontal alignment; AAASIS: angle between acromion and anterior-superior iliac spine; RHA: right hip - angle; LHA: left hip - angle; HRHA: head (right) - horizontal alignment; CRVA: chest (right) - vertical alignment; VABR: vertical alignment of the body (right); HLHA: head (left) - horizontal alignment; CLVA: chest (left) - vertical alignment; VABL: vertical alignment of the body (left).
The posture assessment in a standing position has been increasingly used in clinical practice, as the body alignment observation can be used to plan and monitor physical therapy treatments.
In the present study, seven out of ten angular photographic assessment values from the PAS protocol were inconsistent with the normal values described by Ferreira et al.14 There are several mechanisms, such as lower bone mineralisation, that can justify these postural changes in CF patients. In these patients, bone fractures are relatively common, and respiratory muscles undergo increased stress because of pulmonary hyperinflation.9 Compared to data from patients with chronic obstructive pulmonary disease21, the results of the present study show a similar angular value in the horizontal alignment of the head (2.80 and 2.90, respectively). Despite the age differences of patients, both diseases have a similar basic pathophysiological mechanism (air trapping), which justifies a comparative analysis of the data. The misalignment of the head can be partially explained by the elevation of the ipsilateral acromion, which may be caused by increased tension in the shoulder muscles.22 In obstructive pulmonary diseases, this modification may be caused by changes in pulmonary mechanics.
In the present study, the statistically significant correlations of the pulmonary function variables were observed with the angular value of the vertical alignment of the chest, both in the right and left lateral views. The angular value of the vertical alignment of the chest has the acromion and greater trochanter as bone references. The shortening of the accessory muscles (especially the pectoral and sternocleidomastoid) and abdominal muscles may justify these correlations. Interestingly, Dunk et al.23 observed that the sagittal plane, from which this parameter is extracted, best reflects the postural clinical outcome when the angular sagittal plane values differ from zero; in the frontal plane, the values tend to be zero (symmetry).
When evaluating the static lung volumes and the Raw in CF, the most striking phenomenon is the air trapping that is the consequence of a delayed alveolar emptying. The TLC can also be increased due to the loss of elastic recoil. Another mechanism that can cause the increase in TLC is cutting-off the expiratory time; this causes inspiration begins before air is fully eliminated from the lungs.24 These findings may explain the statistically significant positive correlations among TLC, Raw, and changes in the vertical alignment of the chest.
Another focus was the relationship between functional capacity and body posture. Simpler and less expensive tests such as the 6MWT have been used for assessing exercise tolerance in adult patients with CF, since the distance achieved in the walking test provides an estimate of individual response to maximum incremental exercise.25 Our study showed a significant negative correlation between the 6MWD and the vertical alignment of the chest in the postural assessment. This correlation can be explained by the mechanisms of loss of stability of the chest wall as result of hyperinflation, which in turn leads to a poor functional capacity.
There is evidence that intolerance to exercise in patients with CF is multifactorial, depending on pulmonary function, nutritional state, and adherence to treatment, and other factors.25 In these patients, decreased exercise tolerance limits the performance of daily activities and is associated with lower survival.26 In a study conducted on 88 patients with CF who were at least 10 years old, Ziegler et al.27 found that 15% of the patients presented with oxygen desaturation in the 6MWT. According to our results, it is possible that postural changes may also contribute to poor performance during exercise. Postural deformities cause an imbalance of the muscular system that prevents the normal movement.9 This suggests that conditioning programs along with postural re-education can play a positive role in the limited exercise capacity of CF patients.28,29
Evaluations of QL are important for planning and monitoring treatment and for the identification of predictive factors of QL.30 Regarding the CFQ-R, the results of the present study corroborate those described by Cohen et al.13, who assessed quality of life in patients, including adults, with CF. Both studies showed that the worst domain was the ‘social’ domain, which may be related to the negative perception of patients regarding their performance and social inclusion. In the present study, it is also worth noting that inverses and significant correlations were only observed between two CFQ-R domains (‘physical’ and ‘limitations’) and the postural assessment. The association between functional performance and QL is well established in the literature. Because there was an association between posture and functional performance in our study, the postural abnormalities might have played a direct or indirect role in the health-related quality of life of these individuals. New studies are necessary to evaluate the effects of corrective postural exercises on the QL of patients with CF and in other chronic respiratory diseases.
A critical analysis of the results and their limitations is appropriate. The present study was conducted on a relatively small number of individuals, and no control group was used. Despise these limitations, this is the first study to evaluate the relationship between postural assessment results and lung function parameters in adult patients with CF. Because there are few published studies regarding posture in this group of patients, we believe that our results will make an important contribution to the field. Future studies may reach comprehensive results using more detailed statistical analysis by increasing the number of adult CF patients, control group and longitudinal follow up.
In conclusion, the present study shows that adult patients with CF have significant postural abnormalities. The vertical misalignment of the chest correlates to changes in the lung function, quality of life and functional capacity variables.
Ethic disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Role in the study: Contributions to conception and design, revising the article, and final approval of the version of manuscript.
Please cite this article as: Lopes, A.; Associação entre postura, função pulmonar e capacidade funcional na fibrose quística. Rev Port Pneumol 2013. http://dx.doi.org/10.1016/j.rppneu.2012.07.001.
Role in the study: Analysis and interpretation of data, revising the article, and final approval of the version of manuscript.