Chronic respiratory diseases (CRD) progressively lead to physical inactivity and worsening dyspnoea,1 and cause disability and mortality.2 Strong evidence shows that pulmonary rehabilitation (PR) improves dyspnoea, fatigue, emotional status, exercise capacity and reduces exacerbations.3,4 However, one in two people with CRD referred for PR never attend, and up to one third do not complete the program.5 Others who complete the program have few clinical benefits.6 We recently discussed how urinary symptoms (US), which are frequent in CRD,7 might be a major barrier to participation, completion and response to PR.8 However, our discourse was speculative because no data are available about the relationship between US and PR. A first step to address this question would be to determine its frequency and to characterize the type of symptoms in people with CRD attending PR. Hence, we report the results of a study aimed to assess the frequency and types of US, and their relationship with baseline demographic and cardiorespiratory characteristics, in people with CRD attending PR.
A retrospective chart review of people attending PR between December 2019 and March 2020 was conducted in ADIR Association, Rouen University Hospital, France. Inclusion criteria were adults with CRD (any type) and referral to PR. Ethical approval was granted (E2020-71) and informed consent was not required.
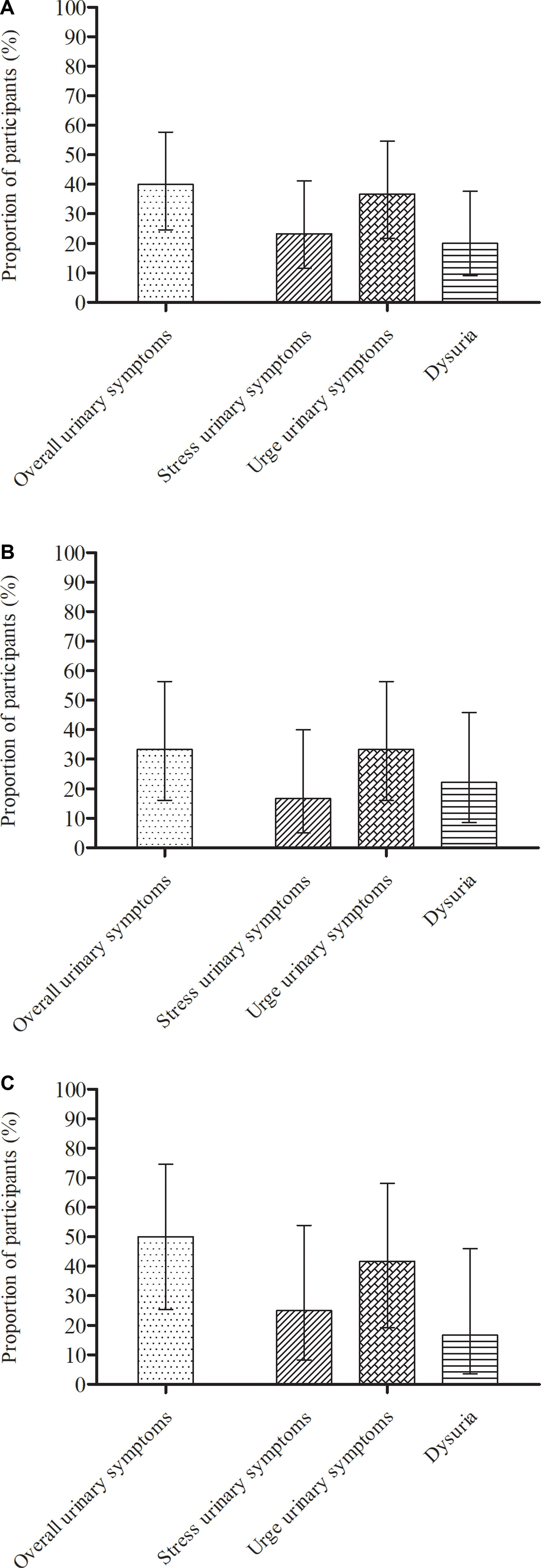
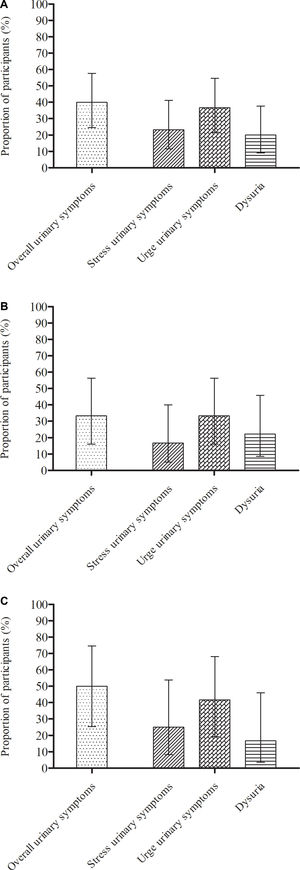
US were assessed during the first PR session using the Urinary Symptom Profile (USP) questionnaire9 which evaluates stress US, urge US and dysuria. No thresholds have been established to define the presence of symptoms, therefore we considered a score above the upper bound of the 95% CI of the mean score for asymptomatic people9 to indicate US. Thus: stress incontinence = score above 1/9, urge incontinence = score above 4/9 and dysuria = score above 1/9.
Continuous data were expressed as means (standard deviation) or medians (25th–75th percentile) and qualitative data as counts and percentages, and their corresponding 95% CI were calculated. The overall rate of US was calculated as the occurrence of at least one type of US. US were also compared between obstructive and non-obstructive CRD using a Fisher test. The relationship between US and demographic or cardiorespiratory characteristics was analysed using a binomial logistic relationship. A p-value <0.05 was considered significant. GraphPad Prism 5.03 and R 3.6.1. software were used.
Thirty people with CRD (43% female, median age 61 years (range 53–67), mean body mass index 26.2 kg/m2 (SD 4.9)) were included. Eighteen (60%) had obstructive CRD, 5 (17%) had lung cancer, 5 (17%) had interstitial lung disease and 2 (7%) had other restrictive CRD. Five (17%) were long term oxygen therapy users. Twelve participants (40%, 95% CI 25–58) experienced at least one type of US; urge US was the most frequent (Fig. 1A). There was no difference in the proportion of participants who experienced at least one type of US between obstructive and non-obstructive CRD (p = 0.26) (Fig. 1B and C). US was not significantly related to demographic or cardiorespiratory characteristics.
The results of this study revealed that US are very frequent in people attending PR. Furthermore, the true rate may be higher since US were assessed on the first day of PR and previous physical inactivity may have masked some symptoms.8 Indeed, PR involves regular and sustained physical exercise, therefore it may both reveal and worsen US, leading participants to reduce their participation or even drop out.8 Since the physiological effects of PR depend on training intensity, lack of adherence considerably reduces the benefits.8,10 In addition, US can worsen the quality of life of people with CRD.11 These results therefore highlight a concerning issue that must be considered in both research and clinical practice.
Importantly, the occurrence of US was similar between participants with obstructive and non-obstructive CRD. It was beyond the scope of this study to evaluate the causes of US, but several risk factors may be common between obstructive and non-obstructive CRD (particularly for tobacco-induced lung cancer). Impaired diaphragm and expiratory muscle biomechanics alter both the stability of the lumbopelvic muscle system and intra-abdominal pressure regulation12 and thus may be a cause of US in people with restrictive CRD or interstitial lung disease.
This study has several limitations. Firstly, the sample size was small and the design was retrospective. The lack of a relationship between US and demographic and cardiorespiratory characteristics may therefore be due to a lack of power. The presence of US was based on threshold scores for the USP that have not been specifically determined9 and may therefore be somewhat inaccurate.
Despite these limitations, the high frequency of US in people with all types of CRD attending PR is concerning. Large, prospective studies are now warranted to evaluate the impact of US on PR adherence and outcomes. Clinicians should screen PR participants for US and provide appropriate treatment to facilitate adherence.
FundingNone.
Ethical approval and consent to participateComité d'Ethique pour la Recherche sur Données Existantes et/ou hors loi Jardé CHU de Rouen (E2020-71).
Conflicts of interestThe authors have no conflicts of interest to declare.
None.