Noninvasive ventilation (NIV) has been increasingly used in acute care setting with various indications1–3,4 but its use in patients with acute hypoxemic respiratory failure (AHRF) is controversial.5,6,7
Although spontaneous patient activity during mechanical ventilation (MV) may reduce the likelihood of ventilation-perfusion mismatch, especially in dependent regions, close to the diaphragm, high transmural vascular and transpulmonary pressure swing may worsen vascular leakage and increase tidal volume (Vt), leading to self-inflicted lung injury (SILI).8 From the clinical side, expiratory Vt of 6mL/kg used in invasive MV during lung protective ventilation1 is almost impossible to achieve in most of the patients receiving NIV for AHRF. This is particularly important in de novo AHRF patients undergoing NIV,1,2 since large expiratory Vt may be generated9,10 in assisted pressure controlled modes by the ventilator pressure and by the respiratory muscles.
In this setting, reliable monitoring of Vt and unintentional leaks is of the utmost importance. When using an intensive care unit (ICU) ventilator driven by high pressures in the double limb configuration, leaks are computed as the difference between inspired and expired Vt. As a consequence, the amount of Vt that the patient gets is usually quantified as expiratory Vt.
However, some points need to be clarified:
- 1)
One characteristic of unintentional leaks is that they are dynamic, which means they can abruptly change during the inspiratory or expiratory phase of the respiratory cycle (even cycle by cycle). Therefore, expiratory Vt measurements using masks may cause concern, because measurements may become unreliable, unstable and difficult to continuously monitor {Carteaux:201dg}, where there may be unintentional expiratory leaks11;
- 2)
Although there is a strong belief that preset Vt is equal to the real delivered Vt, in volume controlled mode using ICU ventilator driven by high pressures, on study found that Vt indicated by the ventilator was lower than the delivered Vt, with a difference that was often greater than 10% of the preset Vt.12 This is also true during pressure controlled mode using NIV, where the direct measurement of flow (and its integration over the time, namely Vt) by the pneumotachograph inside the ventilator, needs to be corrected for the compressible volume. This is the amount of gas which is compressed in the circuit and in the mask (the greater the internal volume of the mask the higher the compressible volume) for each cmH2O of pressure delivered by the ventilator during inspiration. Although most of ICU ventilators are usually equipped with algorithms to calculate and compensate for the compressible volume of the circuit,13 they do not compensate for the mask internal volume or compliance;
Many companies manufacture dedicated turbine driven NIV ventilators (TDV) with a high pressure O2 inlet to preset a given FiO2 and an intentional leak single-limb vented circuit (ILC),11 where Vt is not measured but estimated.14 Although this circuit configuration is extensively used, the accuracy of Vt estimate depends on many factors, including the pressure decrease across the limb, especially where there are high unintentional leaks. This is the reason why some ventilators use a mathematical algorithm to calculate this pressure drop or they still measure pressure close to the mask. Finally, the Vt and leakage estimation in the presence of random leaks remains a challenge when using ILC.1,14 However, Vt estimation has been found to have around 15% when compared to the real measured Vt in restrictive disorders. This means that, when 500ml of volume are generated, estimates may be around ± 75ml, a bias not significantly different from the one measured by many pneumotachographs inside the ventilator.14
They may also allow better patient-ventilator synchrony than ICU pressure driven ventilators, even when coupled with their NIV algorithms.15 Accuracy in estimating leakage is also crucial to improve patient-ventilator synchrony, especially when pneumatic (flow) trigger systems are used. Most of these systems automatically change their sensitivity level according to leakage estimates to avoid trigger asynchronies (autotriggering or ineffective efforts).
Another important concern during NIV in de novo AHRF is that, compared to IMV, it cannot often be used continuously on a daily basis. Although the use of total face mask may increase patient’s tolerance and compliance to NIV and decrease unintentional leaks, the likelihood of maintaining patients under NIV with a mask round the clock for days is remote.
An alternative interface is the helmet, which consists of a transparent hood covering the patient’s whole head with a soft collar neck seal.16 It is kept in place by two armpit belts or by an annular extendable plastic ring positioned under an inflatable cushion that eliminates the need for armpits straps.16 Helmet NIV resulted in higher levels of positive end expiratory pressure (PEEP) and a lower intubation rate in patients with AHRF in a single randomized controlled trial.16 This study suggests that the helmet may allow more time on NIV, at higher PEEP, compared to mask NIV, possibly resulting in a lower rate of endotracheal intubation. However, although interesting in term of comfort and in avoiding skin breakdown, the helmet has restrictions in measuring Vt due to its mechanical properties.16
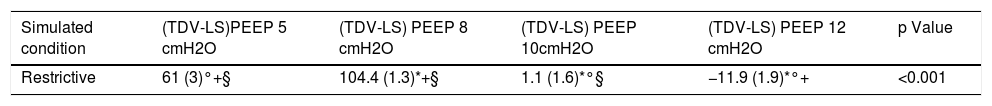
We recently tested the hypothesis17 that TDV coupled with a single limb ILC, setting intentional leak location at the helmet expiratory port,18 would provide patient’s Vt estimates. This configuration allows using the helmet even in continuous positive airway pressure (CPAP) mode without additional rebreathing,18 as in ICU ventilator in double limb configuration.19 Results of the bench simulation in restrictive conditions (Table 117) show that we could potentially use helmet NIV knowing Vt. Besides, differences in Vt between TDV and lung simulator remained stable across different tested leak flows.
Differences in tidal volumes measured by turbine driven ventilator and lung simulator at different levels of PEEP in the bench study.
| Simulated condition | (TDV-LS)PEEP 5 cmH2O | (TDV-LS) PEEP 8 cmH2O | (TDV-LS) PEEP 10cmH2O | (TDV-LS) PEEP 12 cmH2O | p Value |
|---|---|---|---|---|---|
| Restrictive | 61 (3)°+§ | 104.4 (1.3)*+§ | 1.1 (1.6)*°§ | −11.9 (1.9)*°+ | <0.001 |
Data reported from Ref. 17. Data are expressed in ml and reported as mean (±SD). PEEP: positive end expiratory pressure; TDV: turbine driven ventilator; LS: lung simulator; (TDV-LS): difference between VT measurements by turbine driven ventilator and lung simulator. *Different from 5; °different from 8, +different from 10, §different from 12.
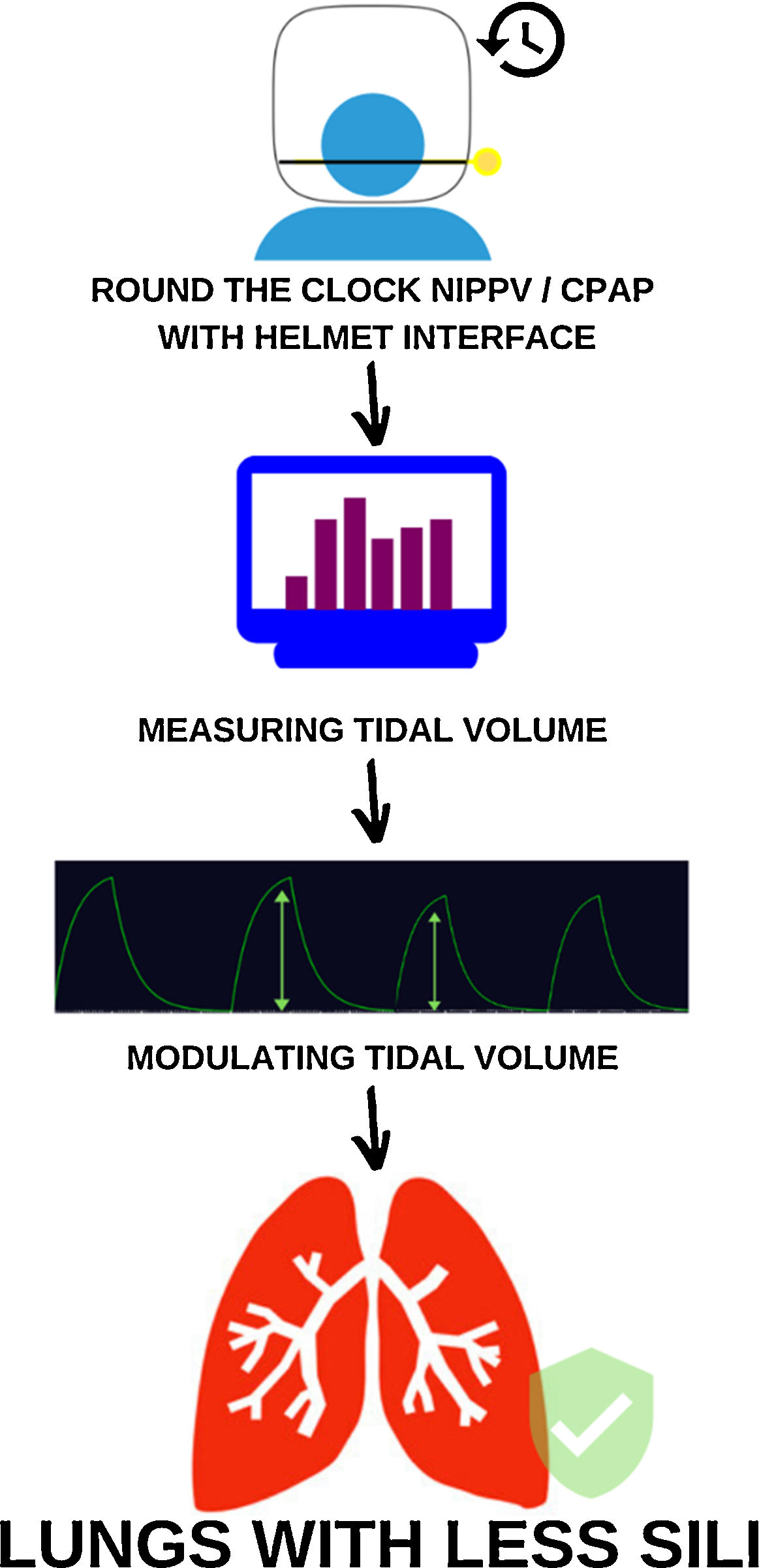
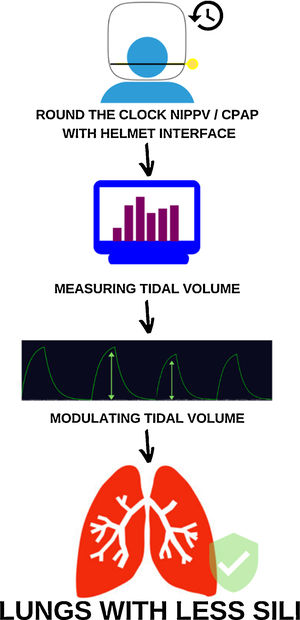
This feasibility bench and human study demonstrated that estimating Vt during helmet NIV seems to be feasible and accurate in restrictive conditions. Although there are now questions about use of NIV in AHRF, the possibility of continuous noninvasive support for patients, knowing Vt, even in CPAP mode, could open new scenarios (Fig. 1), especially in “difficult-to-treat” hypoxemic patients, such as in major burns20 or in the immunocompromised.21 Further clinical studies are required to verify this method.
Modulating tidal volume in NIPPV/CPAP spontaneous breathing patients can reduce SILI.
Mechanism of reducing SILI through measuring and modulating Vt during round the clock cycles of mechanical ventilation with helmet interface.
CPAP: Continuous positive airway pressure; NIPPV: Noninvasive positive pressure ventilation; SILI: Self-induced lung injury.
None.
Authors’ contributionAC, MI, ML, CG conceived the content, wrote the manuscript and approved the last version.
Declarations of interestsAC has a patent pending N° 102019000020532 related to the content of this manuscript; MI declare to have no competing interests; ML received fees for lectures and consultancies from Breas, Philips and Resmed not related to the resent work; CG received fees for lectures or consultancies from Philips, Resmed, Vivisol, Air Liquide not related to the present work, and has a patent pending N° 102019000020532 related to the content of this manuscript.