Non-invasive ventilation (NIV) has been an efficient strategy for ventilatory support and sedation related respiratory failure prevention during endoscopic procedures in high-risk patients. However, there is not enough evidence concerning the ideal pressure setting and choice of interface, mainly in home mechanical ventilated patients that have different interface options.1
We report the use of NIV in a high-risk chronic patient undergoing transoesophageal echocardiography (TEE) under sedation using her own home care vented nasal interface with intentional leaks (Mirage FX™, ResMed, Australia).
The patient was a 31-year-old woman, 45 kg weight, with a previous medical history of cystic fibrosis, chronic respiratory failure and end-stage kidney disease. She was on home mechanical ventilation with high ventilatory dependency (>18 h/day) in spontaneous/timed (ST) bi-level pressure cycled mode [inspiratory positive airway pressure (IPAP) of 17 cmH2O; expiratory positive airway pressure (EPAP) of 4 cmH2O; backup respiratory rate (RR) of 16 cpm], alternating between oro-nasal and nasal interface during sleep and daytime, respectively, continuous oxygen (O2) therapy (2 L/min) and haemodialysis through a catheter placed in the right atrium.
She was hospital admitted due to fluid overload and fever of unknown origin. Aetiological investigation isolated a Methicillin-susceptible Staphylococcus aureus in blood cultures without evidence of respiratory or urinary tract infection. Transthoracic echocardiogram showed a mass in the right atrium in relation to the catheter, requiring TEE characterisation.
Monitoring during TEE included non-invasive blood pressure and pulse oximetry (SpO2). NIV was applied with ST bi-level pressure cycled mode using an acute hospital ventilator with an O2 blender permitting a fraction of inspired oxygen (FiO2) of 100% (Trilogy 202™, Philips Respironics, Pennsylvania, United States). The interface was patient’s home care vented nasal mask. Sedation was performed with intravenous midazolam — intended sedation level of -3 in the Richmond Agitation Sedation Scale (RASS).
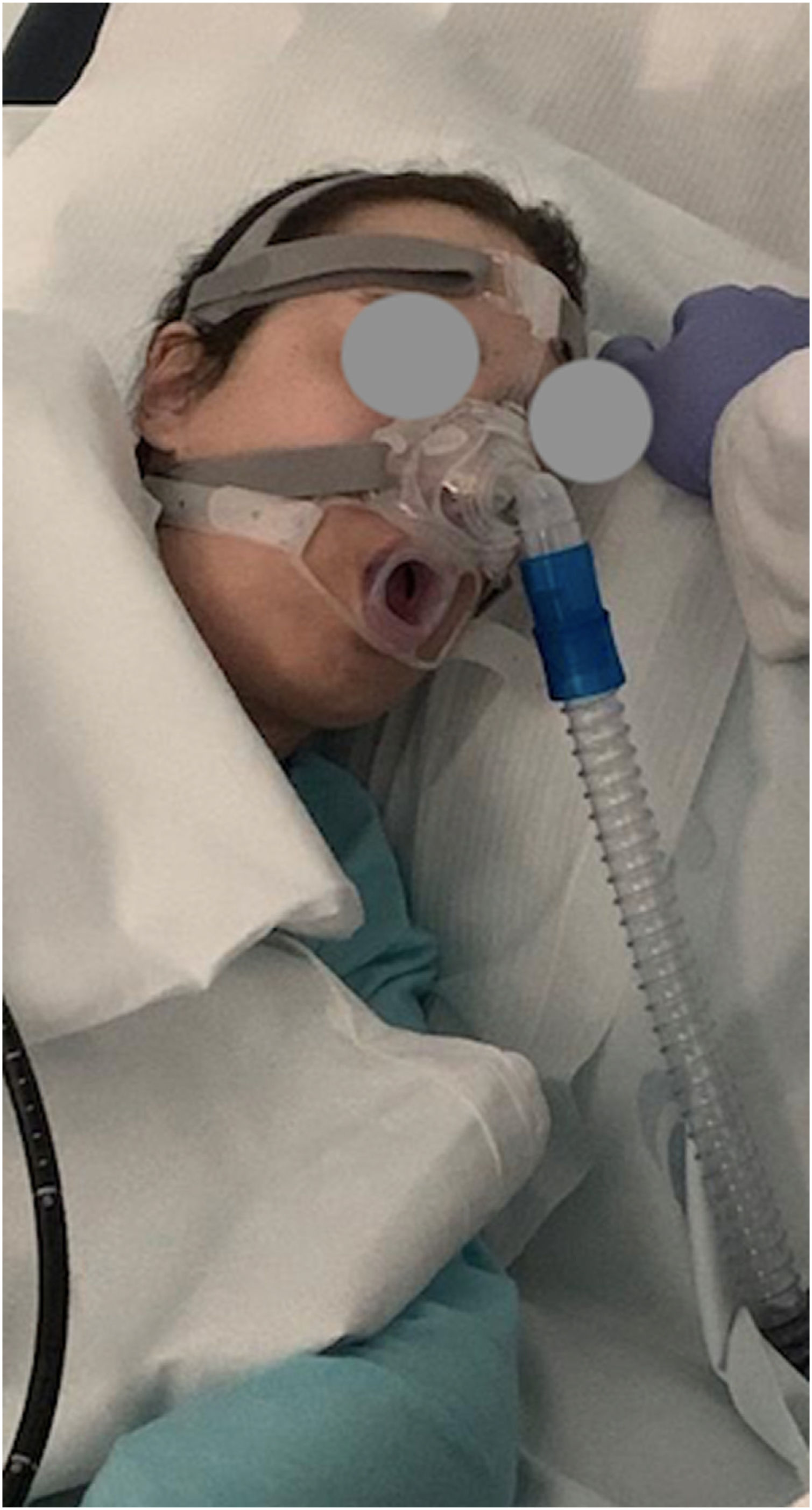
Patient was positioned in lateral decubitus and a mouthpiece was placed for TEE probe insertion (Fig. 1). Initial ventilator settings were set at 22 cmH2O IPAP, 6 cmH2O EPAP and 40% FiO2 to achieve normal RR and SpO2 > 95%. Ventilator settings and FiO2 were adjusted in every episode of SpO2 < 95%.
Incremental doses of 2 mg of midazolam (total 4 mg) were administered to achieve the depth of sedation. Few minutes after initiating the TEE, patient’s SpO2 decreased to 88% and a significant increase of mouth leak (>60 L) was observed. IPAP was incremented to 24 cmH2O and FiO2 was set first at 80% and then 100%, resulting in a SpO2 of 100% and chest excursion throughout, even with persistent mouth leaks. TEE lasted 11 min and operators did not mention any technical difficulty. Patient remained RASS score-3 all procedure, was alert ten minutes post-procedure and tolerated it well with nasal NIV without complaints or complications. TEE revealed a thrombus in the right atrium.
Intravenous sedation is an effective way of achieving patient compliance during TTE. However, it is widely recognized that its use is associated with respiratory depression, desaturation and sometimes with respiratory failure, especially with increased sedative doses2,3 and in chronic respiratory failure patients.3 We describe the use of a home care nasal mask to deliver NIV during TEE in a high-risk patient and proved its effectiveness in preventing sedation induced respiratory failure. No similar report has been found in the English literature.
Air leaks through the mouthpiece were high during the procedure, which in association with the respiratory depression caused by sedation, were responsible for the desaturation episode. Nevertheless, they were effectively compensated with increment of pressure support, resulting in a SpO2 of 100% and chest excursion throughout. When using a single tubing system and with such a large leak, the use of tidal volume (Vte) for ventilatory monitoring may be misleading, since real Vte quantification in this situation is not possible.
The use of NIV as an adjunct to TEE has already been shown to be effective in preventing respiratory failure due to sedation. However, all reports described the use of oronasal or total-face masks.4–6 In those cases, the endoscopic probe had to overcome a mask port before reaching the mouth. The main difficulties reported were in introducing TEE’s probe due to suboptimal gliding through the mask port and excessive image attrition due to difficulties in moving the probe.6 The use of a nasal mask had no interference in TEE probe insertion and handling (Fig. 2). Moreover, the novelty of using the patient’s home care mask is considered to contribute to increased tolerance and cooperation, as she was already trained in its use.
In conclusion, we find two advantages for this approach. First, it is effective in delivering efficient ventilatory support in high-risk patients during TEE avoiding the risk of respiratory failure. Second, the choice of a home care vented nasal mask did not interfere with TEE technique. Monitoring of SpO2 and qualitative clinical signs, such as chest excursion, can be useful for NIV optimization during the procedure.
Conflicts of interestThe authors have no conflicts of interest to declare.