The Brazilian version of Falls Efficacy Scale (FES-BR) used to assess the fear of falling, has not yet been validated in patients with Chronic Obstructive Pulmonary Disease (COPD). The aim of the present study was to investigate the construct validity and reliability of the (FES-BR) in patients with COPD.
MethodsA cross-sectional study involving subjects with COPD, aged between 48 and 83 years. Data were collected by two independent and blind assessors. Construct validity was assessed using the Spearman’s rank correlation coefficient between FES-BR and Berg Balance Scale, Downton fall risk index, Timed Up and Go Test (TUG), hand-grip strength (HGS), Five Times Sit to Stand Test (FTSST) and 6-Minute Walk Test (6MWT). Reliability was measured by the Cronbach’s alpha coefficient, Intraclass Correlation Coefficient (ICC), and Bland-Altman plot.
ResultsThe study included 60 subjects aged 68.3 ± 9.9 years and FEV1 56.0 ± 19.3. The correlations were significantly strong between FES-BR and the Berg Balance Scale (r = −0.66), TUG (r = 0.64), HGS (r = 0.61) and FTSST (r = 0.62); and moderate between FES-BR and the Downton fall risk index (r = 0.38) and the 6MWT (r = −0.48). All correlations had p < 0.001. Intra-rater [ICC = 0.94, (95% CI = 0.91–0.96)] and inter-rater [0.97, (95% CI = 0.97–0.98)] reliability were considered excellent.
ConclusionsThe Brazilian version of FES was valid and reliable in assess fear of falling in subjects with COPD.
Falls are a real risk of multifactorial origin and have been presented as one of the main causes of changes in lifestyle and performance of activities of daily living. According to the World Health Organization 2007,1 approximately 30% of the elderly fall at least once a year. This is also happens to patients with Chronic Obstructive Pulmonary Disease (COPD), recent studies report incidence of between 25% and 46% of falls within this group.2,3,4
Fear of falling, currently defined as low self-efficacy to prevent falls, has been considered not only a consequence but also a determinant of falls,5 since loss of confidence in performing activities of daily living leads to less independence and, consequently, a sedentary lifestyle. This sedentary behavior entails altered balance, reduction of social interaction and depression, which end up generating more fear.6
In this context, the use of instruments that assess fear of falling is relevant, as it may guide prevention and treatment strategies.7 Several instruments are used to assess the risk of falls in COPD8,9,10; however, as far as the authors know, only two scales assess fear of falling. The simplest one to apply in clinical practice is Falls Efficacy Scale International (FES-I).11,12 Its translated and adapted version for the Brazilian Portuguese language presents excellent psychometric properties to assess fear of falling in the elderly, but its validity and reliability in patients with COPD has not yet been verified.
Therefore, the objective of this study was to verify the construct validity and reliability of the Brazilian version of the Falls Efficacy Scale (FES-BR) in subjects with COPD.
MethodsThis was a cross-sectional observational study, carried out from May to August 2018, involving patients in follow-up in the Pulmonary Function Service at the Hospital de Clinicas, Federal University of Paraná (HC/UFPR), in Curitiba, state of Paraná. After approval by the Institutional Ethics Committee (CAAE: 48393915.5.3001.010, Opinion No 1.552.888/2016), patients who met the inclusion criteria were selected to receive telephone contact during which they were invited to participate in the study and to schedule the assessments. They were all informed about the nature and objectives of the study and signed their informed consent.
The study included subjects of both genders, who had COPD diagnosed according to the criteria of the Global Initiative for Chronic Obstructive Lung Disease (GOLD),13 and were clinically stable (no exacerbation of the disease in the previous month), regardless of the staging of the disease. Subjects who had neuromuscular and/or neurodegenerative diseases; arthrodesis and/or prostheses in the lower limbs; severe cardiac arrhythmias or any dysfunction that could hinder their performance in the proposed tests; and subjects who presented any cognitive impairment according to the score by the Mini-Mental State Examination (MMSE)14 were excluded from the test.
Pulmonary function was assessed using a spirometer (Spirobank G, MIR, Italy), following the guidelines of the American Thoracic Society/European Respiratory Society,15 using reference values for the Brazilian population.16 Dyspnea was assessed by the Medical Research Council scale.17
Falls Efficacy Scale, used to assess fear of falling, raises questions about how concerned subjects are about the possibility of falling when performing 16 activities, with scores ranging from 1–4. The total score ranges from 16 (not concerned) to 64 points (extremely concerned), with the score of ≥23 representing high fear of falling.18 Falls Efficacy Scale has already been translated and validated for the Brazilian Portuguese language (FES - BR).11
The validity of the FES-I BR construct was tested to determine its relation with others scales that evaluate the balance (Berg Balance Scale)19 and risk of falling (Downton fall risk index),20 as well as the functional tests. These instruments were used because of the absence of another Portuguese-translated specific instrument for the evaluation of fear of falling, and since functional incapacity is know to be associated with falls.
Balance was assessed by the Berg Balance Scale,19 with scores varying from 0 to 56. High scores indicate better balance. The perception of risk of falls was assessed by the Downton fall risk index,20 which addresses issues such as: known previous falls (yes or no), medications (tranquilizers/sedatives, diuretics, antihypertensives, antiparkinsonian drugs and antidepressants, other medications), sensory deficits (none, visual impairment, hearing impairment, limb impairment), mental state (oriented, cognitively impaired) and gait (normal: safe without walking aids; safe with walking aids; unsafe: with or without walking aids; and unable). Scores of 3 or more indicate a high risk of falls.
The functional tests followed a standard order, with the application of a familiarization test for each one and a rest period of 5 min after each of them. The following functional tests were performed: (1) Timed Up and Go (TUG),21 in which the participant is instructed to stand up from a sitting position, walk 3 m at his normal walking speed and return to the sitting position; (2) Hand-grip strength22 (HGS) assessed using an hydraulic dynamometer (JAMAR Hydraulic Hand Dynamometer - Model PC-5030J1, Fred Sammons, I, 23nc., Burr Ridge, IL: USA), following the protocol recommended by the American Association of Hand Therapists, in which the individual should be seated in a chair, with shoulders in a neutral position, with one hand resting on the thigh while the elbow of the assessed limb is kept in 90 ° of flexion, and the forearm is in neutral position. The dynamometer footprint was individually adjusted for all subjects according to the size of their hands so that the rod closest to the dynamometer body was positioned in the middle phalanges of the index, middle and annular fingers. The test was performed in three attempts for each side, in rotation, starting with the hand the individual considered stronger. The recovery period between measurements was of approximately 30 s. Only the best mark of the three attempts for each hand was used; (3) the Five Times Sit to Stand Test23 that evaluates the lower limbs strength and has a strong correlation with risk of falls, performed in a chair with a 46 cm height and without support for the arms, in which the participants were instructed to remain with their arms crossed over their chest with hands on opposite shoulder. Then, after the initial command, they should sit and stand up 5 times as fast as they were able to. The time was recorded in seconds by means of a digital timer (WTO38 DLK SPORTS); and (4) 6-minute walk test (6MWT),24 which evaluates exercise capacity through the longest of two walks performed during 6 min in a 30-m corridor.
The reproducibility process of FES-BR followed methodological criteria established in the literature25,26 being performed by two independent assessors (assessor 1 and assessor 2), who had received prior and standardized training. They performed the assessments blindly and independently. In an attempt to avoid bias, the score sheets were separated and the assessors did not communicate with each other. In the first assessment, assessor 1 collected data about the characterization of the sample, assessed pulmonary function, and applied the functional tests and scales. After 30 min, assessor 2 reapplied FES-I BR.11 During the application of the scale, the assessor would read the questions and mark the answer indicated by the subject. After 7 days, having preserved the same place and time, FES-I BR was applied again by assessor 1. In addition, the duration of the application was recorded in the two interviews.
Statistical analysisThe sample size followed the methodology proposed by Terwee25 that recommends a sample of at least 50 subjects to assess the validity and reliability of an instrument. For data analysis, the Statistical Package for the Social Sciences (SPSS) software (version 22) was used. The normality and homogeneity of the data were evaluated by the Shapiro–Wilk test and the results are presented in mean and standard deviation or frequency, depending on the type of variable and on the data distribution. The test-retest reproducibility was evaluated by the intraclass correlation coefficient (ICC) and its 95% confidence interval. ICC values between 0.61 and 0.80 and 0.81 and 1.00, respectively, were considered to indicate good and high reliability. The internal consistency of the scale was also verified by Cronbach’s alpha coefficient, which evaluates the magnitude by which the items of an instrument are correlated, where values of α > 0.70 indicate high consistency. The correlation between the test and the retest was also evaluated using the graphical representation of Bland-Altman plot (Medcalc Statistics Software, version 18), in which it was expected that all values of the intra and inter-rater differences would be arranged in parallel around the horizontal axis of zero and within the limits of correlation. The Spearman test was used to examine the degree of association between FES-BR and dyspnea, perceived risk of falls, and all of the above functional tests. The magnitude scale proposed by Hopkins27 was used to interpret the correlation coefficients: <0.1, trivial; between 0.1–0.29, small; 0.30–0.49, moderate; 0.50–0.69, high; 0.70–0.90, very high; >0.90, almost perfect. Differences between groups were investigated by Mann–Whitney and Qui-Square test. The multiple linear regression analisys was performed to determine whether the independent variables with values of p < 0.05 in Table 3, gender, dyspnea, TUG, HGS, FTSST, 6MWT, Berg’s Balance Scale and Downton fall risk index could explain the variability in fear of falling. A stepwise insertion regression approach was used to construct the multivariate models. The established level of significance was p ≤ 0.05.
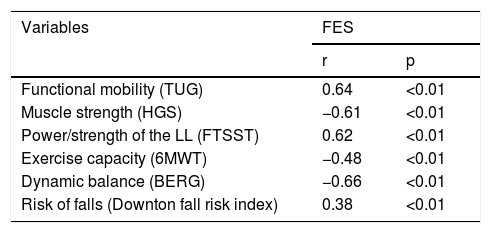
Spearman’s correlations between FES-BR and physical-functional capacity, balance and risk of falls.
| Variables | FES | |
|---|---|---|
| r | p | |
| Functional mobility (TUG) | 0.64 | <0.01 |
| Muscle strength (HGS) | −0.61 | <0.01 |
| Power/strength of the LL (FTSST) | 0.62 | <0.01 |
| Exercise capacity (6MWT) | −0.48 | <0.01 |
| Dynamic balance (BERG) | −0.66 | <0.01 |
| Risk of falls (Downton fall risk index) | 0.38 | <0.01 |
TUG: Timed up and go test; HGS: Hand-Grip Strength; LL: lower limbs; FTSST: Five Times Sit to Stand Test; 6MWT: 6-minute walk test.
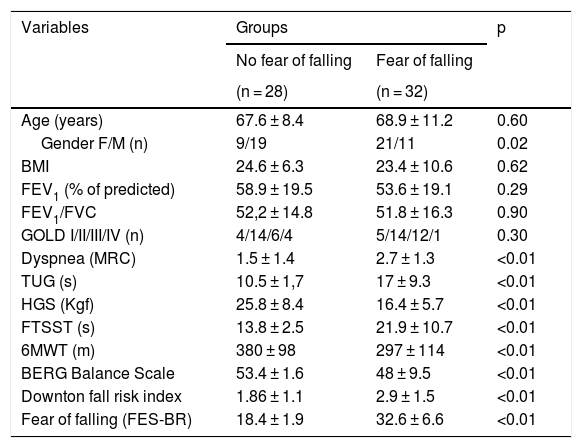
Comparison between groups classified according to fear of falling (FES-I Brazil ≥ 23 points).
| Variables | Groups | p | |
|---|---|---|---|
| No fear of falling | Fear of falling | ||
| (n = 28) | (n = 32) | ||
| Age (years) | 67.6 ± 8.4 | 68.9 ± 11.2 | 0.60 |
| Gender F/M (n) | 9/19 | 21/11 | 0.02 |
| BMI | 24.6 ± 6.3 | 23.4 ± 10.6 | 0.62 |
| FEV1 (% of predicted) | 58.9 ± 19.5 | 53.6 ± 19.1 | 0.29 |
| FEV1/FVC | 52,2 ± 14.8 | 51.8 ± 16.3 | 0.90 |
| GOLD I/II/III/IV (n) | 4/14/6/4 | 5/14/12/1 | 0.30 |
| Dyspnea (MRC) | 1.5 ± 1.4 | 2.7 ± 1.3 | <0.01 |
| TUG (s) | 10.5 ± 1,7 | 17 ± 9.3 | <0.01 |
| HGS (Kgf) | 25.8 ± 8.4 | 16.4 ± 5.7 | <0.01 |
| FTSST (s) | 13.8 ± 2.5 | 21.9 ± 10.7 | <0.01 |
| 6MWT (m) | 380 ± 98 | 297 ± 114 | <0.01 |
| BERG Balance Scale | 53.4 ± 1.6 | 48 ± 9.5 | <0.01 |
| Downton fall risk index | 1.86 ± 1.1 | 2.9 ± 1.5 | <0.01 |
| Fear of falling (FES-BR) | 18.4 ± 1.9 | 32.6 ± 6.6 | <0.01 |
Values are expressed as mean ± SD; Mann-Whitney and Qui-Square for differences between groups; F: female; M: male; BMI: Body Mass Index; FEV1: forced expiratory Volume in the 1st second; FVC: Forced Vital Capacity; GOLD: Global Initiative for Chronic Obstructive Lung Disease; MRC: Medical Research Council; TUG: Timed Up and Go test; HGS: Hand-Grip Strength; FTSST: Five Times Sit to Stand Test; 6MWT: 6-minute walk test; FES-BR: Falls Efficacy Scale Brazil.
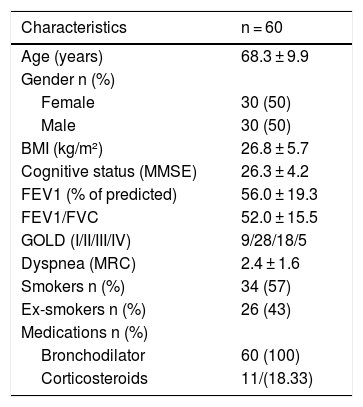
60 patients were included in this study. Most of them were diagnosed with moderate obstruction.13 Demographic, anthropometric and clinical data are presented in Table 1.
Sample characterization.
| Characteristics | n = 60 |
|---|---|
| Age (years) | 68.3 ± 9.9 |
| Gender n (%) | |
| Female | 30 (50) |
| Male | 30 (50) |
| BMI (kg/m²) | 26.8 ± 5.7 |
| Cognitive status (MMSE) | 26.3 ± 4.2 |
| FEV1 (% of predicted) | 56.0 ± 19.3 |
| FEV1/FVC | 52.0 ± 15.5 |
| GOLD (I/II/III/IV) | 9/28/18/5 |
| Dyspnea (MRC) | 2.4 ± 1.6 |
| Smokers n (%) | 34 (57) |
| Ex-smokers n (%) | 26 (43) |
| Medications n (%) | |
| Bronchodilator | 60 (100) |
| Corticosteroids | 11/(18.33) |
Values are expressed as mean ± SD, absolute (n) and relative (%); BMI: Body Mass Index; MMSE: Mini-Mental State Examination; FEV1: Forced Expiratory Volume in the 1 st second; FVC: Forced Vital Capacity; GOLD: Global Initiative for Chronic Obstructive Lung Disease; MRC: Medical Research Council.
A high association was observed between the Falls Efficacy Scale (FES-BR) and the tests that evaluated physical-functional capacity such as Timed Up and Go (TUG), Hand-grip strength (HGS), Five Times Sit to Stand Test (FTSST), and balance (Berg’s Balance Scale). Moreover, moderate association was found between the FES-BR and the Downton Scale, and the 6-minute walk test (6MWT) (Table 2).
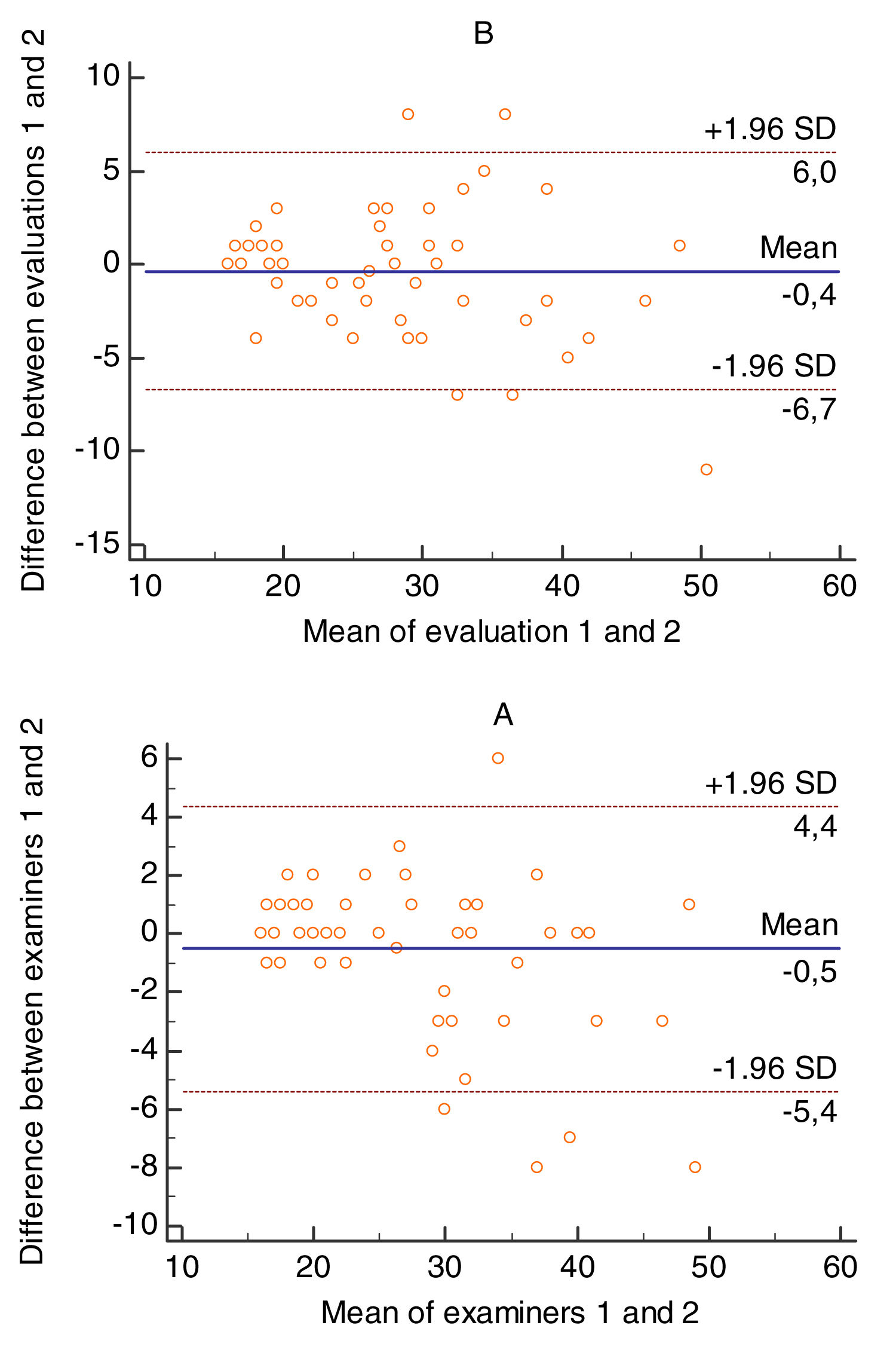
FES-BR reliabilityThere was no difference between the evaluators 1 and 2 regarding the time of application of the scale (17.67 vs 17 min., p = 0.09). The intra-rater ICC was 0.94, (95% CI = 0.91–0.96), p < 0.01 and the ICC inter-rater 0.97, (95% CI = 0.97–0.98), p < 0.01, representing high intra and inter-rater reliability. In addition, the high value of Cronbach's alpha coefficient for the two raters (α de Cronbach = 0,90) supports these results.
Intra and inter-rater agreement is illustrated by the graphical representations of Bland-Altman plot (Fig. 1), where the existence of low bias intra [−0.4 (limit of correlation between 5.9 and −6.6)] and inter-rater [−0.5 (limit of correlation between 4.3 and −5.4] appear.
Thirty-two patients (53%) presented fear of falling (FES-BR score ≥23), consequently, it was possible to divide the sample into two groups: with (n = 32) and without (n = 28) fear of falling. When compared, the groups presented significant differences regarding gender, dyspnea, TUG, HGS, FTSST, 6MWT, balance (Berg’s Balance Scale), fall risk index (Downton) and fear of falling (FES-BR) (Table 3).
In addition, multiple linear regression with the stepwise insertion method analisys showed that the independent variables TUG, HGS, FTSST together explained approximately 55% (r2 = p < 0.01) the variability of FOF in the study population: TUG (ß = 0.465; t = 4.634; p < 0.01), HGS (ß = −0.303; t = −2.999; p < 0.01) and FTSST (ß = 0.210; t = 2.283; p = 0.026).
DiscussionIn order to properly use an instrument, it is necessary to evaluate its psychometric properties. This evaluation is done, therefore, by analyzing the validity and reliability of the test. This study demonstrated that the Brazilian version of Falls Efficacy Scale (FES-BR) presented high construct validity and excellent reliability in patients with chronic obstructive pulmonary disease (COPD). In addition, patients classified with fear of falling have worse clinical, physical-functional, and balance profiles, besides the greater risk of falls, whereas lower functional mobility, poor peripheral muscle strength and power and strength of the lower limbs reliably predicted fear of falling.
The construct validity of the FES-BR was demonstrated by its high association with the physical-functional capacity and dynamic balance, and moderate relation with the perceived risk of falls and the exercise capacity, suggesting that the scale score also reflects the limitations presented by patients with COPD. Patients with COPD with lower physical capacity and poor dynamic balance have a considerable increase in fear of falling. Such functional tests were used because they are reliable, valid and responsive28,29,30 in COPD. Besides, these procedures are commonly performed in most health services because they reflect the patients’ physical-functional limitation. Similarly, Berg’s and Downton scales were used because they involved constructs related with the individual’s exposure to different situations which generate postural imbalance and fear of falling.
The relation between increased fear of falling and impairment of physical-functional capacity also been demonstrated in other studies. In Greek,31 Turkish,32 Persian,33 Hungarian34 and Arabic35 version, FES was compared with the TUG in community-dwelling older persons and showed a high corrrelation (0.64 < r < 0.74, p < 0.01 for all). Similarly in the Portuguese version,36 FES was highly correlated with TUG (r = 0.50; p < 0.01) and FTSST (r = 0.54; p < 0.01).
The high reliability of the FES-BR presented in this study was demonstrated by the excellent internal consistency as demonstrated by the Cronbach’s alpha coefficient, which measures the existence of a correlation between the responses given by the subjects, close to 1.00, as well as by the high value of ICC intra and inter-raters, demonstrating that the scores on the scale were similar between the assessments. In addition, the high correlation demonstrated by the graphical representation of Bland-Altman plot in the test-re-test, whose variability of intra and inter-rater differences were within the 95% of concordance limits, validated the aforementioned results. Moreover, recent studies have corroborated our results.31–33
Therefore, our results confirm that fear of falling is a common feature among patients with COPD, affecting 53% of the subjects in this study. Patients with fear of falling presented lower functional mobility, peripheral muscle strength, power and strength of the lower limbs, greater risk of falls, walked a shorter distance in 6 min and had worse balance when compared to those without fear of falling. Moreover, they are mostly female and clinically presented greater dyspnea during Activities of Daily Living (ADL). This relationship was already expected, since the fear of falling restricts the patient in their ADL, and, consequently, worsens their functional performance and their symptoms. This is the first study to demonstrate differences in these functional variables between COPD’ patients with and without fear of falling. This result can be explained by the fact that COPD is considered a systemic disease that leads to musculoskeletal disorders13 increasing the proportion of people with a higher fear of falling.
In addition, the regression analisys showed that lower functional mobility, poor peripheral muscle strength and power and strength of the lower limbs together explain more than half of the fear of falling variability. The influence of reduced physical function on the fear of falling is clinically relevant, as there is evidence that fear of falling is an independent predictor of future falls in older adults.37 The results of this study strengthens the inclusion of the fear of falling assessment in a pulmonary rehabilitation program. Similar associations have also been demonstrated in other studies where increased fear of falling was particularly related to lower quadriceps muscle strength and impaired balance.5,38
Finally, some limitations of the study should be considered: (1) it was not possible to evaluate the FES-BR responsiveness, because even with psychometric evidence of reliability and validity, an instrument must be responsive. That is, it should detect change after an intervention; (2) the reduced sample size, since it is a unicentric study; (3) the average FEV1 of the sample was 56% predicted, indicating a sample with predominantly moderate disease, and (4) the identification of clear causal relationship between fear of falling and the physical function capacity was limited by the cross-sectional study design.
The results presented in this study indicate the need to introduce the assessment of fear of falling in the treatment of the patient with COPD. This addition can make the patient aware of the risk factors which cause falls and, consequently, provide effective measures to prevent them. Following this principle, the authors emphasize that, at the end of each evaluation, the patients that were subjects to this study received an educational booklet with guidelines related to the risk of falls and how to prevent them.
In summary, the conclusion is that the Brazilian version of FES can be used in patients with COPD as an important tool to assess the fear of falling.
FundingThis work was supported by the CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior) [grant number 40001016012P1]
Conflict of interestNo conflicts of interest.
We would like to thank Mary Tinetti for the permission to use the FES-I and the Pulmonary Function Service staff at the Clinical Hospital in Curitiba, Brazil.



![Bland & Altman’s graphical comparisons results in the intra [1A] inter-rater [1B]. Bland & Altman’s graphical comparisons results in the intra [1A] inter-rater [1B].](https://static.elsevier.es/multimedia/25310437/0000002600000005/v1_202009020805/S2531043720300301/v1_202009020805/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9znTMwFdb/TnkS0koegILxs=)



