Amyotrophic lateral sclerosis (ALS) is a degenerative neurological disorder that affects motor neurons. Involvement of respiratory muscles causes the failure of the ventilator pump with more or less significant bulbar troubles. ALS course is highly variable but, in most cases, this disease entails a very significant burden for patients and caregivers, especially in the end-of-life period.
In order to analyze the characteristics of ALS patients who die at home (DH) and in hospital (DHosp) and to study the variability of clinical practice, a retrospective medical records analysis was performed (n=77 from five hospitals). Variables: time elapsed since the onset of symptoms and the beginning of ventilation, characteristics of ventilation (device, mask and hours/day), and support devices and procedures.
ResultsIn all, 14% of patients were ventilated by tracheotomy. From the analysis, 57% of patients were of DH. Mean time since the onset of symptoms was 35.93±25.89 months, significantly shorter in patients who DHosp (29.28±19.69 months) than DH (41.12±29.04) (p=0.044). The percentage of patients with facial ventilation is higher in DHosp (11.4% vs 39.4%, p<0.005).
DH or not is related to a set of elements in which health resources, physician attitudes and support resources in the community play a role in the decision-making process. There is great variability between countries and between hospitals in the same country. Given the variability of circumstances in each territory, the place of death in ALS might not be the most important element; more important are the conditions under which the process unfolds.
A esclerose lateral amiotrófica (ELA) é uma perturbação neurológica degenerativa que afeta os neurónios motores. O envolvimento dos músculos respiratórios causa a falha da bomba ventilatória, com problemas bulbares mais ou menos significativos. A evolução da ELA é bastante variável, mas, na maioria dos casos, esta doença implica um peso muito significativo para doentes e prestadores de cuidados, em particular no período terminal.
Para analisar as características dos doentes com ELA que morrem em casa (DH) e no hospital (DHosp), para além da avaliação da variabilidade das práticas clínicas, foi realizada uma análise retrospetiva dos registos médicos (n=77 de 5 hospitais). Variáveis: tempo decorrido desde o aparecimento dos sintomas e o início da ventilação, características da ventilação (dispositivo, máscara e horas/dia) e dispositivos e procedimentos de apoio.
ResultadosCatorze por cento dos doentes foram tratados por traqueotomia. Cinquenta e sete por cento dos doentes morreu em casa (DH). O tempo médio desde o aparecimento dos sintomas foi de 35,93 ± 25,89 meses, significativamente inferior em doentes que morrem no hospital (DHosp) (29,28 ± 19,69 meses) comparativamente com os que morrem em casa (DH) (41,12 ± 29,04) (p=0,044). A percentagem de doentes com ventilação facial foi superior nos DHosp (11,4% vs 39.4%, p<0,005).
DH ou não, está relacionado a um conjunto de factores em que os recursos de saúde, as atitudes dos médicos e o apoio na comunicação desempenham um papel importante na tomada de decisão. Existe uma grande variabilidade entre países e entre hospitais no mesmo país. Dada a variabilidade de circunstâncias em cada território, o local do óbito na ELA poderá não ser o elemento mais importante, sendo provavelmente mais relevantes as condições em que o processo se desenrola.
Amyotrophic lateral sclerosis (ALS) is a degenerative neurological disorder that affects motor neurons, causing progressive and irregular loss of muscle strength. ALS progressively affects ventilatory pump with more or less significant bulbar involvement. The course of the disease is highly variable, and although lung function has prognostic value,1 it has no predictive value since the loss of respiratory muscle function can occur abruptly.
This disease entails a very significant burden for caregivers,2 both from the perspective of care and from the economic and emotional aspects. In recent years there has been a change of attitude toward tackling the disease. Initially the clinicians’ position was more pessimistic about the treatment, citing the poor short-term prognosis. However, the introduction of noninvasive ventilation, percutaneous gastrostomy and mechanical aids for cough augmentation3 improved the quality of life of patients and, possibly, even their survival. One of the challenges facing most health systems is to respond to the needs of these complex patients in the final stages of life.
Previous studies have shown the main issues for patients and caregivers for coping with the disease, especially during the end-of-life period: overall, ALS patients were aware of their prognosis and disease severity, having been kept well informed by their doctors. Caregivers reported control of symptoms in their relatives but the relief of the respiratory symptoms was not easily achieved despite the use of drugs and sedatives. Family burden and hospitalization access were high. Deaths were equally distributed between home and hospital, and NIV use and diagnosis influenced familial reporting.4
The aim of this study was to analyze the characteristics of ALS patients who die at home and in hospital and to study the degree of variability of clinical practice. Moreover, it aimed at identifying the elements that can improve care in the final stages of life in order to design care projects capable of responding to patients’ real needs.
MethodsThis retrospective study was conducted in five hospitals from the north of Italy and Catalonia (Spain) by analyzing medical records of ALS patients treated at the hospital and who died of the disease. Four hospitals were public hospitals with beds dedicated to acute care and fifth was a private center (Fondazione S. Maugeri IRCCS) involved in rehabilitation/long-term needs and research for chronic diseases, but in all cases patients do not have to pay any money at the time of care.
In 2010 all cases of patients diagnosed with ALS in every hospital who had died in the previous twelve months whether at the hospital or in a health care facility or at home were analyzed.
The variables considered in each patient were age (years) and gender (male/female), time elapsed since the onset of symptoms (months) (TEOS), time elapsed since the beginning of ventilation (months) (TEBV), type of ventilation prescription (elective/acute), characteristics of the ventilation in the last week of life (pressure, volumetric), type of mask used (nasal/facial), number of hours of ventilation in the last week (measured according to the data of the medical record), management of secretions (use of cough assist, bag or manual in the medical record), presence of percutaneous endoscopic gastrostomy (PEG), and drug consumption (morphine, benzodiazepine, other). The definition of the type of ALS (spinal/bulbar) was defined according to the clinical information, with or without objective data.
Statistical analysisPatient population was classified into two subgroups according the place of death: home or hospital. Statistical analysis was performed using SPSS 13.2 software (SPSS Inc., Chicago, IL, USA). A descriptive analysis of variables derived by medical record was performed (expressed as %). Binary logistic regression was performed using “place of death” as dependent variable. A two-sided p-value<0.05 was considered to be statistically significant.
ResultsThe medical record of 77 patients (women: 44.2%, mean age: 66.3±11.9yrs) was analyzed. There were no differences regarding age related to the place of death.
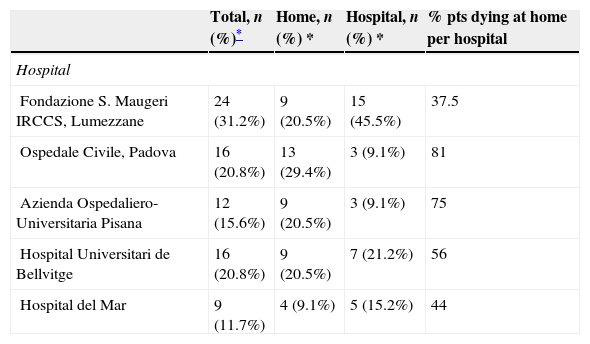
Hospital distributionIn all, 57% of patients died at home. The probability of dying at home is significantly related to the hospital where the patient is cared for. The percentage of patients who died in hospital ranged from 18.7% to 62.5% (p=0.045). Table 1 shows the distribution of the five hospitals of the patients according to the place of death.
Hospital distribution.
| Total, n (%)* | Home, n (%) * | Hospital, n (%) * | % pts dying at home per hospital | |
|---|---|---|---|---|
| Hospital | ||||
| Fondazione S. Maugeri IRCCS, Lumezzane | 24 (31.2%) | 9 (20.5%) | 15 (45.5%) | 37.5 |
| Ospedale Civile, Padova | 16 (20.8%) | 13 (29.4%) | 3 (9.1%) | 81 |
| Azienda Ospedaliero-Universitaria Pisana | 12 (15.6%) | 9 (20.5%) | 3 (9.1%) | 75 |
| Hospital Universitari de Bellvitge | 16 (20.8%) | 9 (20.5%) | 7 (21.2%) | 56 |
| Hospital del Mar | 9 (11.7%) | 4 (9.1%) | 5 (15.2%) | 44 |
P value: 0.045.
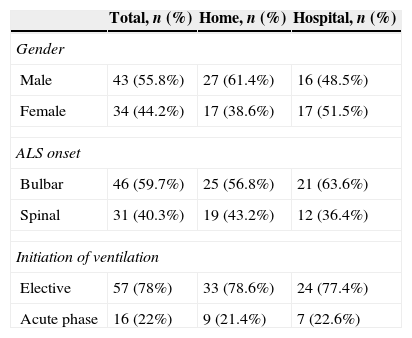
There are no differences regarding age, gender, characteristics of the onset of the disease (bulbar or spinal) or type of ventilation prescription (elective or acute) (Table 2).
Patient characteristics and onset of the disease.
| Total, n (%) | Home, n (%) | Hospital, n (%) | |
|---|---|---|---|
| Gender | |||
| Male | 43 (55.8%) | 27 (61.4%) | 16 (48.5%) |
| Female | 34 (44.2%) | 17 (38.6%) | 17 (51.5%) |
| ALS onset | |||
| Bulbar | 46 (59.7%) | 25 (56.8%) | 21 (63.6%) |
| Spinal | 31 (40.3%) | 19 (43.2%) | 12 (36.4%) |
| Initiation of ventilation | |||
| Elective | 57 (78%) | 33 (78.6%) | 24 (77.4%) |
| Acute phase | 16 (22%) | 9 (21.4%) | 7 (22.6%) |
Gender: p value=0.186.
ALS onset: p value=0.357.
Initiation of ventilation: p value=0.95.
Mean time elapsed since the onset of symptoms (months) (TEOS) was 35.93±25.89 months, significantly shorter in patients who died in hospital (29.28±19.69 months) than at home (41.12±29.04) (p=0.044).
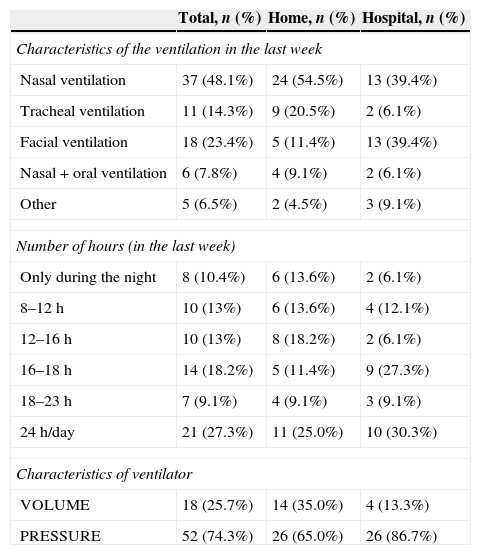
Variables related to ventilation during the last weekThe variables related to ventilation during last week are shown in Table 3.
Variables related to ventilation.
| Total, n (%) | Home, n (%) | Hospital, n (%) | |
|---|---|---|---|
| Characteristics of the ventilation in the last week | |||
| Nasal ventilation | 37 (48.1%) | 24 (54.5%) | 13 (39.4%) |
| Tracheal ventilation | 11 (14.3%) | 9 (20.5%) | 2 (6.1%) |
| Facial ventilation | 18 (23.4%) | 5 (11.4%) | 13 (39.4%) |
| Nasal+oral ventilation | 6 (7.8%) | 4 (9.1%) | 2 (6.1%) |
| Other | 5 (6.5%) | 2 (4.5%) | 3 (9.1%) |
| Number of hours (in the last week) | |||
| Only during the night | 8 (10.4%) | 6 (13.6%) | 2 (6.1%) |
| 8–12h | 10 (13%) | 6 (13.6%) | 4 (12.1%) |
| 12–16h | 10 (13%) | 8 (18.2%) | 2 (6.1%) |
| 16–18h | 14 (18.2%) | 5 (11.4%) | 9 (27.3%) |
| 18–23h | 7 (9.1%) | 4 (9.1%) | 3 (9.1%) |
| 24h/day | 21 (27.3%) | 11 (25.0%) | 10 (30.3%) |
| Characteristics of ventilator | |||
| VOLUME | 18 (25.7%) | 14 (35.0%) | 4 (13.3%) |
| PRESSURE | 52 (74.3%) | 26 (65.0%) | 26 (86.7%) |
Ventilation in the last week p value=0.029.
Number of hours p value=0.43.
Characteristics of ventilator p value=0.036.
The place of death is significantly related to the characteristics of ventilation during the last week, specifically related to the airway interface (p=0.029): % of patients with facial ventilation is higher in the hospital group (11.4% vs 39.4%, p<0.005), and also to the type of ventilator: the percentage of patients using volume ventilator is significantly higher among those who die at home (p<0.036).
The percentage of patients who are ventilated by tracheotomy in the study group is 14% (17% in patients with bulbar involvement and 9% in patients without bulbar involvement). There are no significant differences regarding the invasive access to the airway (namely tracheo or not) related to the place of death.
Variables related to care during the last weekThere were no significant differences in drug consumption (amitriptyline, baclofen, benzodiazepines, lithium carbonate, morphine or riluzole) during the last week of life, except in the case of omeprazole, the use of which was significantly higher in hospital (p<0.044).
There were no significant differences in access to devices or methods for managing secretions among patients who die in hospital or at home or in the use of PEG.
DiscussionIn our retrospective study the place of death is significantly related to the hospital, the time elapsed since the onset of symptoms and the type of airway access in the last week.
There are limitations to the interpretation of our findings, especially in relation to the sample size and the number of hospitals studied. However, these preliminary data suggest that the organization of health care and some aspects of the disease may play a role.
We found significant differences in the percentage of patients who die at home according to the hospital. The possibility of dying at home or not is related to a set of elements in which health resources, physician attitudes and support resources in the community play a role in the decision-making process.
In France only 36% of patients died outside medical facilities (mainly at home).5 Most French patients die in acute hospitals and only 12% out of the total die in hospices or long-term care facilities.
The variability within the same country is very high, as we can see in the results of the three Italian hospitals. In one region of Italy over 85% of patients die at home.6 However, these data should be interpreted with caution, since in many cases they refer to hospital records and not to population analysis. In order to understand the patients’ preferences it might be interesting to analyze the role of reference centers.
It seems logical to think that a reference center improves outcomes because it focuses on the knowledge and skills needed to manage complex patients as in the case of ALS. However, the benefits are more related to the intensity of interventions than to the concentration of patients. Zoccolella et al.7 showed that multidisciplinary clinics did not improve survival. In this study the rate of interventions in both the groups (multidisciplinary clinic and general neurology clinic) was very low: only 2.5% of patients used NIV in both groups and 6% of patients in multidisciplinary clinic used PEG.
Another bias in the analysis of the benefits of reference centers is in recruitment. Some evidence suggest that proactive and aggressive therapy improves survival.8 Hutchison et al.9 suggested that the ALS clinic treated a group of fitter ALS patients and the general neurologists saw all patients (especially patients living further from ALS clinic, more disabled or older). Chiò et al.10 confirm this approach. Patients treated in specialized clinics are four years younger than those treated at non-specialized neurology clinics, they receive more aggressive treatments (PEG and NIV), they have fewer hospital admissions, and most of the hospital admissions are planned.
There are doubts about the benefits of a living will11 to help physicians make clinical decisions at the end of life, mainly with respect to the decision to perform a tracheotomy or for the patient to die at home or in hospital. The most important factor is the doctor's communication skills.
A diverse but interrelated set of factors influence patient choices and attitudes about living and dying with ALS. There are specific circumstances that change attitudes about death and the place of death. In the Netherlands, in 2000–2005 16.8% of ALS patients chose the option of euthanasia or physician-assisted suicide (PAS), and 14.8% died during continuous deep sedation (CDS).12 This attitude is not uniform across countries, and ethical issues emerge as a main element of care plan throughout the course of the disease.13 The increase in interventions in the end-of-life period is likely to increase admissions to hospitals or health care facilities.
The time elapsed since the onset of symptoms is an important prognostic factor. As Kaufmann et al.14 showed, symptom duration at baseline visit was a significant predictor of survival: shorter duration means higher mortality.
The patients’ preferences regarding treatment choices change over time. Patients who found the interventions acceptable (PEG, NIV or tracheo) for life-extending were more likely to be recently diagnosed.15 One possible explanation for the fact that patients who die in hospital had a shorter course of the disease could be a positive attitude toward more aggressive treatments. In our study, the disease course is a year longer in patients who die at home. Another possible explanation could be that adaptation to a disease as serious as ALS takes time.
Over 60% of patients using facial mask in the last week die in hospital. A total face mask is a possible option for patients in acute respiratory failure with leaks or nose bridge skin problems.16 There are no objective reasons for the increased use of face mask ventilation in patients who die in the hospital. But it seems clear that it is more difficult to care for patients with a facial mask compared with those who only need a nasal mask.
There is no specific reason for the greater chance of dying in hospital for the patients who use a face mask. Perhaps these patients have worsened and do not want tracheotomy, so the facial mask is an alternative, or perhaps the use of a facial mask is an overload for the caregiver because with facial mask fluid intake and communication is much more difficult.
Tracheotomy does not prevent discharging severe ALS patients home. Lo Coco et al. showed that 92% of ALS patients with tracheotomy could go back home, with a median survival time of 37 months,17 and Vianello et al.18 showed that 87% of patients die at home. In our survey, 80% of patients with a tracheotomy die at home, a similar percentage to that described by Lo Coco and Vianello. Although it may seem paradoxical, patients with tracheotomy might represent less of a burden for the caregiver in ensuring effective ventilation. Suctioning is also easier through the tracheostomy.
In our study no differences were observed regarding the place of death in relation to the presence or absence of bulbar involvement. Further studies are needed to examine the relationship between bulbar involvement and place of death in patients with ALS. The percentage of patients who are ventilated by tracheotomy in the study group is 14%. This percentage is slightly higher in the group with bulbar involvement (17%). Perhaps this small difference in favor of the tracheotomy minimizes the impact of bulbar involvement as a determinant of place of death.
The accessibility of drugs and devices for secretion management is the same for both the groups of patients. This fact emphasizes that death at home does not mean undertreatment.
The analysis of the place of death in ALS should not be restricted to discussion of the hospital or at home. As Servera et al.19 pointed out, the care of patients with ALS should be evaluated comprehensively. The therapy “package” should include devices or techniques for respiratory support or nutrition, but the therapy “package” must also include the organization of care in the community and easy communication with expert teams. Telemedicine20 plays a crucial role in an integrated care model. Hospice or health care facilities could be useful for patients dependent on a ventilator who lack family support.21
It is very difficult to establish the criteria for the best place to meet the needs of the end-of-life stages in patients with ALS. It is necessary to establish care plans to meet the needs of each patient, according to the resources that are locally available.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank Ms. Jordina Capella for her help in statistical analysis and Ms Elena Torrente for her help in the edition.