It is not known what the magnitude of non‐identified TB contacts is in our country, or the reasons why contacts at risk are not identified.
ObjectiveThe purpose of this study was to analyze the determinants associated with non‐identification of contacts.
DesignThis cross‐sectional study included all cases of pulmonary tuberculosis diagnosed and treated in the Chest Disease Centre of Vila Nova de Gaia and their contacts, from 1st January to 31st December 2010. It included information collected from patients related to the identification of contacts in risk, and the information collected by the Public Health Unit during home, work and social places visits.
ResultsDuring the period of study, 61 cases of pulmonary TB were diagnosed: 41 cases (67.2%) identified all their contacts and 20 cases (32.8%) did not. 646 contacts were identified: 154 (23.8%) were identified only by the Public Health Unit (mean age of 40.67), and 492 (76.2%) were identified by the index cases (mean age of 33.25), (p=0.001). A mean of 10.59 contacts were identified per index case, of which, 83 (19.3%) screened positive. From those identified by the Public Health Unit, 10 (9.8%) had LTBI and 5 (4.9%) had active TB, and by the index case 61 (18.6%) had LTBI and 7 (2.1%) had active TB (crude OR=1.52; CI=0.83–2.79). The multivariate analysis showed that employment (adjusted OR=4.82; 95%CI=1.71–13.54) was associated to non‐identification of contacts and patients preferably tended to identify relatives and co‐habitants (adjusted OR=0.22; 95%CI=0.10–0.47).
ConclusionTB patients tend to identify relatives and co‐habitant contacts; contact at place of employment was found to be an independent risk factor for not being identified.
Não é conhecida a magnitude dos contactos de TB não identificados no nosso país, nem os motivos porque os contactos em risco não são identificados.
ObjetivoO objetivo deste estudo foi analisar as determinantes associadas à não‐identificação dos contactos.
Materiais e MétodosEste estudo transversal incluiu todos os casos de tuberculose pulmonar diagnosticados e tratados no Centro de Doenças Pulmonares de Vila Nova de Gaia e os seus contactos, de 1 de janeiro a 31 de dezembro de 2010. Incluiu a informação recolhida de doentes relacionada com a identificação dos contactos em risco e a informação recolhida pela Unidade de Saúde Pública durante as visitas ao domicílio, ao trabalho e a espaços sociais.
ResultadosDurante o período de estudo, foram diagnosticados 61 casos de TB pulmonar: 41 casos (67,2%) identificaram todos os seus contactos e 20 casos (32,8%) não o fizeram. Foram identificados 646 contactos: 154 (23,8%) foram identificados apenas pela Unidade de Saúde Pública (idade média de 40,67 anos) e 492 (76,2%) foram identificados pelos casos índice (idade média de 33,25, p=0,001). Foram identificados uma média de 10,59 contactos por Caso Índice, dos quais 83 (19,3%) rastreados como positivos. Dos identificados pela Unidade de Saúde Pública, 10 (9,8%) tinham uma LTBI (infeção tuberculosa latente) e 5 (4,9%) TB ativa, e pelo Caso Índice, 61 (18,6%) tinham LTBI e 7 (2,1%) TB ativa, (OR bruto=1,52; CI=0,83–2,79). A análise multivariada mostrou que o emprego (OR ajustado=4,82; 95% CI=1,71–13,54) estava associado à não identificação de contactos e os doentes tinham tendência, preferencialmente, a identificar familiares e coabitantes (OR ajustado=0,22; 95% CI=0,10–0,47).
ConclusãoOs doentes com TB tendem a identificar os contactos de familiares e coabitantes; os contactos no local de trabalho foram considerados um fator de risco independente para não ser identificado.
Contact screening is one of the most widely discussed public health strategies for reducing tuberculosis (TB) and the risk of transmission.1,2 Not all contacts at risk are identified by the index case and in some studies, a high proportion (53%) of patients who developed active TB had had a previous, contact with a TB case which had not been notified.3–5
In previous studies, many factors have been associated with lack of identification of contacts at risk. A low level of education, fear of stigma, lack of advice, lack of collaboration, not knowing contacts’ names, and reluctance to visit health care services have all contributed to some contacts not being screened.6,7
In Portugal, 2559 cases of TB were diagnosed in 2010 (incidence of 22.3 per 100.000 residents).8 Vila Nova de Gaia has a population of approximately 302.092 people9 and an incidence of TB of 30.8 per 100.000 residents in 2010.10 According to national guidelines, contact tracing is triggered whenever a case of pulmonary TB is diagnosed.11 Patients with confirmed diagnosis of infectious TB are interviewed and asked to report the names of contacts in the different contexts of daily activities at home, at work and socially.
In Vila Nova de Gaia, a complementary strategy was added in January 2004: after diagnosis, all cases are reported to the Public Health Units (PHU), who will screen contacts at risk already identified by the index case (IC). After the interview, the PHU begins conducting routine visits to households, workplaces, congregate settings, homeless shelters, hospitals and prisons, identifying more at‐risk.10
It is not known what the magnitude of the number of non‐identified TB contacts in our country is or the reasons for not identifying contacts at risk. The purpose of this study was to analyze determinants associated with this non‐identification of contacts by the patients with confirmed diagnosis of infectious TB, during the period between January 1st, 2010 and December 31st, 2010 at the Chest Disease Centre of Vila Nova de Gaia.
Ethical approvalScreening of at‐risk populations is endorsed by the National Tuberculosis Program Guidelines of the National Health Department in “Programa Nacional de Luta contra a Tuberculose” published in the Portuguese Official Government Gazette [(The Republic Daily/Diário da República) II series, n° 218] on September 20th, 1997. Naturally, patient anonymity is preserved throughout the data analysis.
MethodsThis population‐based cross‐sectional study included all cases of pulmonary TB diagnosed and treated in the Chest Disease Centre of Vila Nova de Gaia and their contacts between 1st January and 31st December 2010. Data collection was processed after reviewing clinical and nursing records.
The following variables were selected for this study: gender, age, country of origin, place of residence (households, congregate settings and homeless shelters), professional status, symptomatology, co‐morbidities, HIV infection, drug users, previous history of TB, contact type, contact time and screening result. This information was collected from all cases and their contacts.
Due to the change in strategy, two groups were designed: Public Health Unit (PHU) vs. index case (IC). The variables associated were analyzed to determine the non‐identification of contacts.
Definitions- •
Case of pulmonary TB: sputum or bronchial lavage culture positive for Mycobacterium tuberculosis.3
- •
Latent tuberculosis infection (LTBI): asymptomatic individuals with a normal chest radiography and positive tuberculin skin test or interferon gamma assay (IGRA) positive.3
- •
Contact: individual with a history of exposure to a case during the infectivity period.3
- •
Frequent contacts: individuals exposed to TB case for more than 8h a day or more than 40 cumulative hours during the infectivity period.3
- •
Sporadic contacts: individuals exposed to TB case for less than 8h a day or less than 40 cumulative hours during the infectivity period.3
- •
Positive screening: result of contacts that were diagnosed positive to TB or LTBI.
Unconditional logistic regression was used to measure the magnitude of associations between the outcome and the covariates. A multivariable analysis using logistic regression was conducted with all variables that were associated with the outcome in the univariate analysis. Results were reported as odds ratios (OR) and their respective 95% confidence intervals (95%CI). The significant level was fixed at 0.05. Statistical analyses were performed using the software SPSS 19.
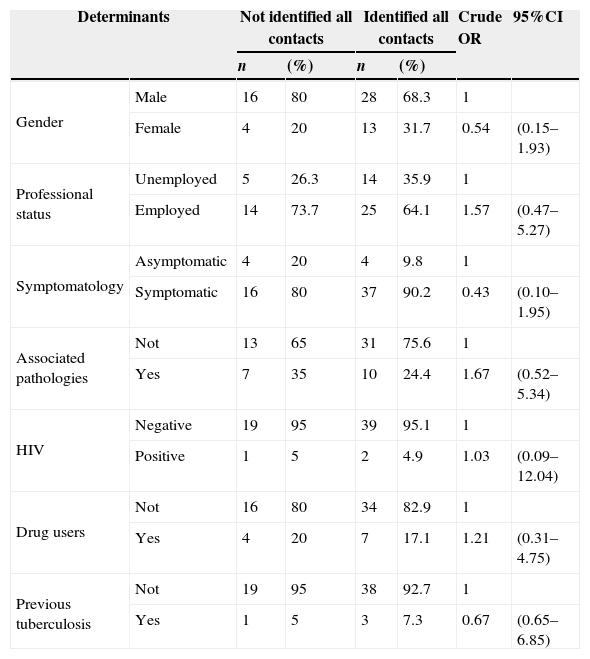
ResultsIn the period studied, 61 cases of pulmonary TB were reported, of which 41 cases (67.2%) identified all their contacts and 20 cases (32.8%) did not. No determinant associated to lack of identification of contact was found (Table 1).
Determinants for the identification of contacts by the index cases.
| Determinants | Not identified all contacts | Identified all contacts | Crude OR | 95%CI | |||
|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | ||||
| Gender | Male | 16 | 80 | 28 | 68.3 | 1 | |
| Female | 4 | 20 | 13 | 31.7 | 0.54 | (0.15–1.93) | |
| Professional status | Unemployed | 5 | 26.3 | 14 | 35.9 | 1 | |
| Employed | 14 | 73.7 | 25 | 64.1 | 1.57 | (0.47–5.27) | |
| Symptomatology | Asymptomatic | 4 | 20 | 4 | 9.8 | 1 | |
| Symptomatic | 16 | 80 | 37 | 90.2 | 0.43 | (0.10–1.95) | |
| Associated pathologies | Not | 13 | 65 | 31 | 75.6 | 1 | |
| Yes | 7 | 35 | 10 | 24.4 | 1.67 | (0.52–5.34) | |
| HIV | Negative | 19 | 95 | 39 | 95.1 | 1 | |
| Positive | 1 | 5 | 2 | 4.9 | 1.03 | (0.09–12.04) | |
| Drug users | Not | 16 | 80 | 34 | 82.9 | 1 | |
| Yes | 4 | 20 | 7 | 17.1 | 1.21 | (0.31–4.75) | |
| Previous tuberculosis | Not | 19 | 95 | 38 | 92.7 | 1 | |
| Yes | 1 | 5 | 3 | 7.3 | 0.67 | (0.65–6.85) | |
Possible association of the main variables that might present determinants factors that prevented index cases identified their contacts.
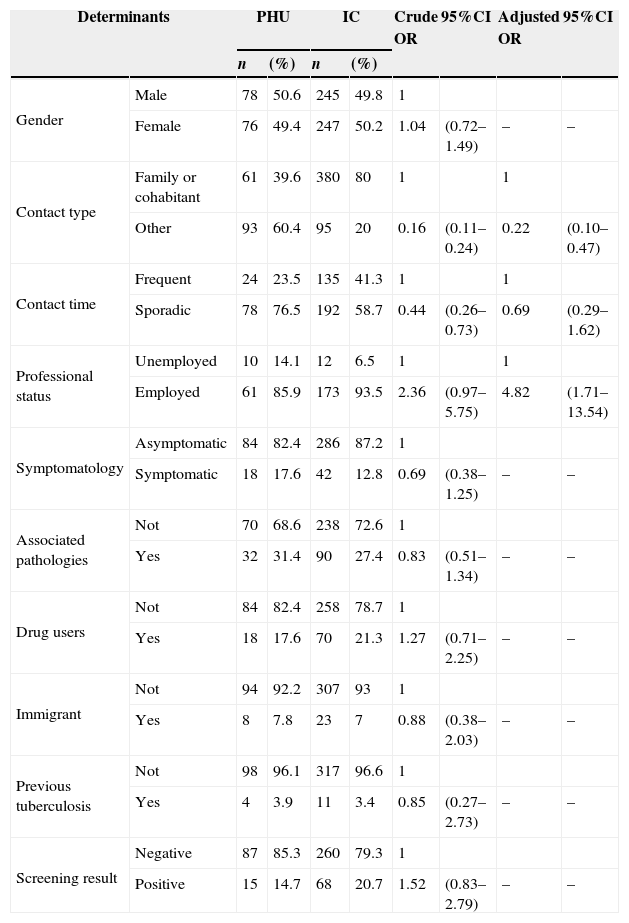
Both strategies succeeded in identifying 646 contacts, of which 154 (23.8%) were identified by the PHU and 492 (76.2%) identified by the IC (Table 2). Being employed (adjusted OR=4.82; 95%CI=1.71–13.54) and not being a relative or a co‐habitant (adjusted OR=0.22; 95%CI=0.10–0.47) were independent risk factors for not being identified and proposed for screening by the IC (Table 2).
Determinants for the identification of contacts by the PHU vs. IC.
| Determinants | PHU | IC | Crude OR | 95%CI | Adjusted OR | 95%CI | |||
|---|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | ||||||
| Gender | Male | 78 | 50.6 | 245 | 49.8 | 1 | |||
| Female | 76 | 49.4 | 247 | 50.2 | 1.04 | (0.72–1.49) | – | – | |
| Contact type | Family or cohabitant | 61 | 39.6 | 380 | 80 | 1 | 1 | ||
| Other | 93 | 60.4 | 95 | 20 | 0.16 | (0.11–0.24) | 0.22 | (0.10–0.47) | |
| Contact time | Frequent | 24 | 23.5 | 135 | 41.3 | 1 | 1 | ||
| Sporadic | 78 | 76.5 | 192 | 58.7 | 0.44 | (0.26–0.73) | 0.69 | (0.29–1.62) | |
| Professional status | Unemployed | 10 | 14.1 | 12 | 6.5 | 1 | 1 | ||
| Employed | 61 | 85.9 | 173 | 93.5 | 2.36 | (0.97–5.75) | 4.82 | (1.71–13.54) | |
| Symptomatology | Asymptomatic | 84 | 82.4 | 286 | 87.2 | 1 | |||
| Symptomatic | 18 | 17.6 | 42 | 12.8 | 0.69 | (0.38–1.25) | – | – | |
| Associated pathologies | Not | 70 | 68.6 | 238 | 72.6 | 1 | |||
| Yes | 32 | 31.4 | 90 | 27.4 | 0.83 | (0.51–1.34) | – | – | |
| Drug users | Not | 84 | 82.4 | 258 | 78.7 | 1 | |||
| Yes | 18 | 17.6 | 70 | 21.3 | 1.27 | (0.71–2.25) | – | – | |
| Immigrant | Not | 94 | 92.2 | 307 | 93 | 1 | |||
| Yes | 8 | 7.8 | 23 | 7 | 0.88 | (0.38–2.03) | – | – | |
| Previous tuberculosis | Not | 98 | 96.1 | 317 | 96.6 | 1 | |||
| Yes | 4 | 3.9 | 11 | 3.4 | 0.85 | (0.27–2.73) | – | – | |
| Screening result | Negative | 87 | 85.3 | 260 | 79.3 | 1 | |||
| Positive | 15 | 14.7 | 68 | 20.7 | 1.52 | (0.83–2.79) | – | – | |
Intended to assess possible associations for the main variables that could present determinants among the contacts that prevent them from identifying by PHU vs. IC.
Overall, a mean of 10.59 contacts were identified per index case, of which, 19.3% screened positive. Among all contacts identified by the PHU, 10 (9.8%) had LTBI and 5 (4.9%) active TB. Among all contacts identified by the IC, 61 (18.6%) had LTBI and 7 (2.1%) TB.
Contacts identified by the PHU were older (mean age of 40.67) than the contacts identified by the IC (mean age of 33.25), (p=0.001).
DiscussionIn our study, being employed (adjusted OR=4.82; 95%CI=1.71–13.54) and not being a relative or a co‐habitant of the index case (adjusted OR=0.22; 95%CI=0.10–0.47) were associated with not being identified by the IC. Likewise being older was a risk factor for not being identified by the IC (p=0.001). This finding is consistent with other studies12–15 that found the mean age of the contacts with TB to be of approximately 35 years.
We found a strong association between the employment status of the contacts and identification for screening. The contacts that were employed were almost five times more likely not to be identified by the IC compared to the unemployed. It is possible that cases do not know the names of all co‐workers with whom they had significant contact, or that they feared discrimination among their colleagues and losing their jobs.7,16,17
In this study, relatives and co‐habitants had 78% more chances of being identified by the IC for screening than other contacts. Other studies5,7 identified the quality of the interview as a cause for lack of contact identification – cases may not understand what is meant by “contacts”. In others12 homeless index cases were more likely to be unable to identify contacts whom they could name.
Some drug users have shown a significant reluctance to provide names of their contacts, mainly due to the fear that their privacy and their contacts’ privacy might be invaded.7,18 In this study, being a drug user was not a risk factor for not being identified as a risk contact. This may be explained by the fact that the city of Vila Nova de Gaia in 2004 established a partnerships with support Centres for drug users, with street shelters and with teams responsible for looking after drug users in the community, aiming to improve detection of TB cases among drug users and to facilitate the access to health care services.6,10
There were 10 (9.8%) LTBI and 5 (4.9%) active TB cases among the contacts identified by the PHU. This implies that special efforts should be made during the investigation of contacts by the IC to identify all contacts at risk. Likewise, it is effective for public health workers to visit households, workplaces, congregate settings, homeless shelters, hospitals and prisons to identify contacts.10,19,20
This study concluded that TB patients tend to identify relatives and co‐habitants contacts, and their employment contacts were an independent risk factor for not being identified.
The strengths of this study lie in the setting and design. The study was a population‐based cross‐sectional study with the contacts identified by PHU – and contacts identified by IC – matched group. Official statistics software was used to analyze the determinants associated with non‐identification of contacts. The use of data from only one Chest Disease Centre reduced the possible confounding effect of differences in the identification of contacts between Chest Disease Centres.
The first limitation of this study is the sample size and the restriction of data to one Chest Disease Centre only, which limited generalization of the results. Secondly, no contact identified by PHU in this study was known to be HIV positive, limiting our ability to analyze this group. The analysis allowed the study of only a few variables, when there might be many others. The analysis of clinical and nursing records was done by the author, and some degree of subjectivity is hence inevitable.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work Centre on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe Authors declares that there is no conflict of interest.