Obstructive Sleep Apnea (OSA) is characterized by recurrent episodes of apnea and hypopnea, secondary to collapse of the upper airways during sleep. OSA is frequently associated to cardiovascular complications. In Portugal, its magnitude is unknown.
MethodsIn 2014 a cross-sectional study was performed using the Portuguese General Practitioner (GP) Sentinel Network (Rede Médicos Sentinela). Participants GP reported all OSA cases diagnosed and registered in their lists of users on the 31 December 2013.
Frequency of OSA has been estimated by sex and age. OSA patients were also characterized by method of diagnosis, treatment, and underlying conditions.
Association between risk factors and severe OSA (odds ratio) was calculated using a logistic regression model adjusting confounding.
ResultsPrevalence of OSA on the population aged 25 years or more was 0.89% (95 CI: 0.80–1.00%); it was higher in males 1.47% (95 CI: 1.30–1.67%) and in those aged between 65 and 74 (2.35%). Most had severe OSA (48.4%). Hypertension (75.9%), obesity (74.2%) and diabetes mellitus (34.1%) were the most frequent comorbidities. Being a male (OR: 2.6; 95 CI: 1.2–5.8) and having obesity (OR: 4.0; 95 CI: 1.8–8.6) were associated with an increased risk of severe OSA.
ConclusionFound frequency of OSA was lower than other countries estimates, which may be explained by differences on case definition but can also suggest underdiagnosis of this condition as reported by other authors.
The Obstructive Sleep Apnea (OSA) is characterized by recurrent episodes of apnea or hypopnea secondary to a collapse of the upper airways during sleep.
A wide variability in OSA prevalence is found between studies due to important differences in cases definition and study population.1
It is estimated that the prevalence of OSA (defined by the presence of episodes of hypopnea and apnea and frequent daytime sleepiness) in adult men vary between 1% and 5%.1 Considering OSA definition currently used (occurrence of more than 5 episodes of apnea and hypopnea per hour), prevalence of OSA, accordingly sex and age group, can vary between 2% and 28%, half of which is classified as moderate or severe.2,3 Prevalence of undiagnosed OSA may range between 0.3% and 5%.4
As OSA affects mainly middle-aged and obese males,5 it is recognized that the increase in obesity may contribute to an increase in OSA prevalence.
In addition to its high magnitude, the clinical importance of OSA comes from its cardiovascular effects, consequences on morbidity and mortality6,7 and also neuropsychological changes that increase the occurrence of occupational and traffic accidents.8 OSA is a risk factor for hypertension and it is also known that high blood pressure risk increases with severity of OSA.9 In fact, given the high frequency of OSA within individuals with hypertension,10 the latest standard for hypertension diagnostic approach recommends performing OSA diagnosis in cases of high blood pressure which are resistant to treatment and have a non-dipper pattern on 24h records of blood pressure.11,12 It is also known that prevalence of sleep-disordered breathing among patients who had strokes is high, ranging between 44% and 74%,13 emphasizing that the presence of OSA in these patients is associated with an increased risk of premature mortality.14
The association between Diabetes and OSA has recently been described and there is emerging evidence that OSA constitutes a risk factor for development of resistance to insulin15 independently of obesity, which may be involved in metabolic syndrome development.16
Another aspect that reinforces the importance of the diagnosis of OSA is linked to the efficacy of nasal Continuous Positive Airway Pressure (CPAP) therapy in reversing neuropsychological disorders and reducing cardiovascular events.17 As a consequence of CPAP treatment, reduction of excessive daytime sleepiness contributes to quality of life improvement and accident risk reduction but also the occurrence of high blood pressure is clearly lower in the short and long term.18
Although Portuguese prevalence of OSA is unknown, considering the high prevalence of adult obesity in Portugal19 a high prevalence of OSA can be expected in the adult Portuguese population. Neither is the patient profile with OSA known, especially in terms of severity, treatment, comorbidities and use of health services.
As it is not currently feasible to implement a population based survey to estimate the Portuguese prevalence of OSA, the first approach to the subject is to estimate the frequency of OSA known within the population under observation of the General Practitioner (GP) Sentinel Network and to characterize OSA patients.
Material and methodsA cross sectional study was performed within the GP Sentinel Network (known as Rede Médicos Sentinela), which has national distribution and 117 GP in 2013.
At the beginning of the study all Sentinel GP included in the Rede Médicos Sentinela in 2013 and also GPs that joined the network in the first trimester of 2014 (a total of 7) were invited to participate. Invitation was sent by email and renewed by phone call. The study protocol, questionnaire forms and detailed study instructions were sent to all doctors that accepted to take part in the study.
GP participation consisted in filling in a questionnaire for each and all of their patients diagnosed with OSA at 31st of December of 2013, using existing recorded information data to collect following data:
- 1.
Sex and age.
- 2.
Diagnostic, including: diagnostic date, overnight polysomnography or overnight respiratory polygraphy performance, apnea–hypopnea index, respiratory disturb index.
- 3.
Comorbidities: diabetes, high blood pressure, obesity, coronary disease, stroke, acute myocardial infarction, arrhythmia, heart failure, occurrence of traffic accident (as driver).
- 4.
Treatment: CPAP, specialized sleep medical appointment.
An OSA case was defined as someone having a previous diagnosis of OSA performed by a specialist and known by the patient's family doctor.
A Severe OSA was defined as someone having an apnea–hypopnea index or respiratory disturb index equal or higher than 30.
Proportion of OSA was estimated by sex and age group using the sum of users aged 25 years and more followed by each participating GP as denominator (total of 34,909 individuals that comprises the study sample).
95 Confidence intervals (95 CI) were computed using Wilson method.20 No estimates were presented for age groups with less than 5 cases.
Mean (and 95 CI) and median were computed for numeric variables; proportions (and 95 CI) for categorical variables.
¿2 test was used to identify variables associated to severe OSA and a logistic regression model, using all variables in which ¿2 significant level was <0.20, was performed to estimate adjusted Odds Ratio (and 95 CI) of having severe OSA among all OSA patients.
Model assumptions of the final regression model were checked by residual analysis. Hosmer and Lemeshow test was used to check the goodness of the final regression model.
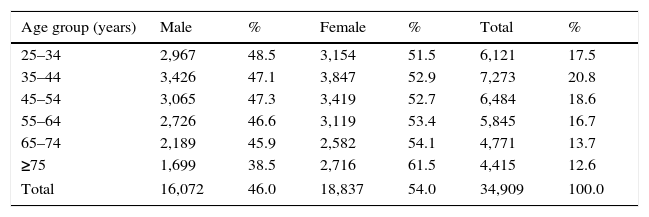
Results29 (of 124) GP agreed to participate, giving a population under observation of 34,909 individuals (Table 1). All the GP that accepted participating in the study sent information relating to OSA cases, which corresponds to a 100% participation rate. In relation to sex and age distribution, no differences were found between the study population and the Portuguese population (Supplementary material).
Study population by sex and age group.
| Age group (years) | Male | % | Female | % | Total | % |
|---|---|---|---|---|---|---|
| 25–34 | 2,967 | 48.5 | 3,154 | 51.5 | 6,121 | 17.5 |
| 35–44 | 3,426 | 47.1 | 3,847 | 52.9 | 7,273 | 20.8 |
| 45–54 | 3,065 | 47.3 | 3,419 | 52.7 | 6,484 | 18.6 |
| 55–64 | 2,726 | 46.6 | 3,119 | 53.4 | 5,845 | 16.7 |
| 65–74 | 2,189 | 45.9 | 2,582 | 54.1 | 4,771 | 13.7 |
| ≥75 | 1,699 | 38.5 | 2,716 | 61.5 | 4,415 | 12.6 |
| Total | 16,072 | 46.0 | 18,837 | 54.0 | 34,909 | 100.0 |
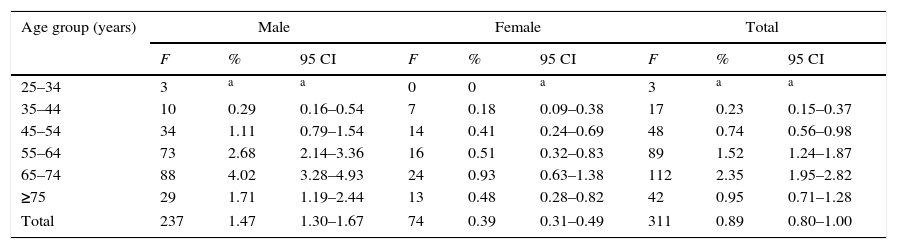
311 cases of OSA were identified in that population; the average age was 62.8 years (95 CI: 61.6–64.1) and no age difference was found between sexes.
Proportion of cases aged 25 years and more has been 0.89% (95 CI: 0.80–1.00). A higher proportion of OSA was found in males, namely between 65 and 74 years (4.02%; 95 CI: 3.28–4.93) (see Table 2).
Distribution of Obstructive Sleep Apnea by sex and age.
| Age group (years) | Male | Female | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| F | % | 95 CI | F | % | 95 CI | F | % | 95 CI | |
| 25–34 | 3 | a | a | 0 | 0 | a | 3 | a | a |
| 35–44 | 10 | 0.29 | 0.16–0.54 | 7 | 0.18 | 0.09–0.38 | 17 | 0.23 | 0.15–0.37 |
| 45–54 | 34 | 1.11 | 0.79–1.54 | 14 | 0.41 | 0.24–0.69 | 48 | 0.74 | 0.56–0.98 |
| 55–64 | 73 | 2.68 | 2.14–3.36 | 16 | 0.51 | 0.32–0.83 | 89 | 1.52 | 1.24–1.87 |
| 65–74 | 88 | 4.02 | 3.28–4.93 | 24 | 0.93 | 0.63–1.38 | 112 | 2.35 | 1.95–2.82 |
| ≥75 | 29 | 1.71 | 1.19–2.44 | 13 | 0.48 | 0.28–0.82 | 42 | 0.95 | 0.71–1.28 |
| Total | 237 | 1.47 | 1.30–1.67 | 74 | 0.39 | 0.31–0.49 | 311 | 0.89 | 0.80–1.00 |
Note: F – frequency, 95 CI – 95% confidence interval.
97.3% (95 CI: 94.5–98.7) of all cases had undergone sleep study and of those 56.2% had undergone polysomnography. 48.4% (95 CI: 40.8–56.1) had a severe disease (AHI or RDI≥30) and only 17.6% (95 CI: 12.5–24.3) had a mild disease [5≤(AHI or RDI)<15].
More than half of the cases (59.5%; 95 CI: 53.8–65.0) were followed through specialized medical appointments. Continuous positive airway pressure treatment was prescribed to 89.6% of all patients (95 CI: 85.7–92.6), being this proportion higher (96.1%) for those who had a severe clinical condition.
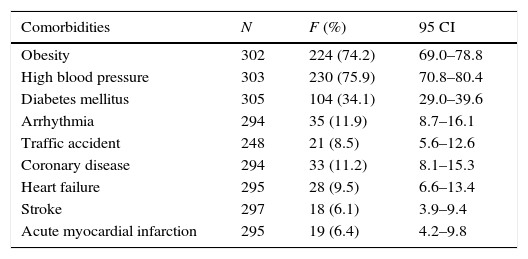
High blood pressure (75.9%), obesity (74.2%) and diabetes mellitus (34.1%) were the most frequent comorbidities in OSA patients (Table 3).
Comorbidities.
| Comorbidities | N | F (%) | 95 CI |
|---|---|---|---|
| Obesity | 302 | 224 (74.2) | 69.0–78.8 |
| High blood pressure | 303 | 230 (75.9) | 70.8–80.4 |
| Diabetes mellitus | 305 | 104 (34.1) | 29.0–39.6 |
| Arrhythmia | 294 | 35 (11.9) | 8.7–16.1 |
| Traffic accident | 248 | 21 (8.5) | 5.6–12.6 |
| Coronary disease | 294 | 33 (11.2) | 8.1–15.3 |
| Heart failure | 295 | 28 (9.5) | 6.6–13.4 |
| Stroke | 297 | 18 (6.1) | 3.9–9.4 |
| Acute myocardial infarction | 295 | 19 (6.4) | 4.2–9.8 |
Note: N – number of valid observations, F – frequency, 95 CI – 95% confidence interval.
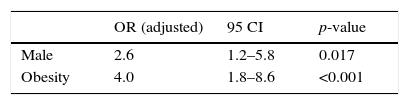
In relation to OSA severity, it was found that being male (OR: 2.6; 95 CI: 1.2–5.8) and obese (OR: 4.0; 95 CI: 1.8–8.6) showed an association to a higher risk of having severe disease among all OSA patients (Table 4).
DiscussionPrevalence of Obstructive Sleep ApneaAlthough this study focused only on diagnosed OSA cases by family doctors, the low prevalence of OSA (0.89%) found suggests that like other studies2–4,8,21 this clinical condition is actually underdiagnosed. Nevertheless, as case identification was performed using medical registries that use the second version of the International Classification for Primary Care (ICPC2) we cannot exclude the effect of the registries’ characteristics during the case identification process.
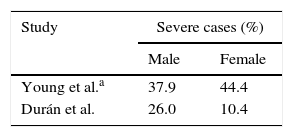
On the other hand, compared to other countries2,3 (Table 5) a higher proportion of severe cases was found on our study (48.4%), which suggests that OSA patients known in primary health care setting are those with a severe clinical presentation. The legal requirement for a treatment prescription performed by a medical doctor within the National Health System is probably favors a better knowledge of severe cases.
Proportion of severe cases.
| Study | Severe cases (%) | |
|---|---|---|
| Male | Female | |
| Young et al.a | 37.9 | 44.4 |
| Durán et al. | 26.0 | 10.4 |
Note: Proportions computed from prevalence values of OSA.
Considering the hypothesis of underdiagonis and accepting the fact that severe cases represents 20% of all OSA cases (a similar value was found in Spain3), OSA prevalence at population level (aged 25 years and more) could be around 2.2%, which is still lower than that found in USA2 (4% male, 2% female) and Spain3 (26.2% male, 28.0% female). Several methodological differences between studies were found (namely in sampling framework, age groups, case selection and case definition1–3,21) that limit data comparability. Nevertheless, as case definition used in Young et al. study2 includes the presence of symptoms of OSA and an AHI≥5, we considered that it can be closer to the case definition used in this study than that used by Durán et al.3 However, given our case definition (previous diagnosis performed by a specialist and known by the patient's family doctor), a selection bias cannot be excluded if OSA diagnosis had been more frequently made in male patients, which may explain a higher sex ratio estimate (3.8 male:1.0 female) than that observed by Young et al.2 (3:1).
The highest prevalence of OSA for both sexes found between 65 and 74 years of age can indicate a late diagnose of OSA when compared to other study which show that the highest prevalence in men was observed between the 5th and 6th decades of life.22 These results highlight the hypothesis of underdiagnosis of OSA, namely among young and less health care consumer population.
ComorbiditiesThe underlying conditions observed in our OSA patients were those frequently associated to OSA as risk factors (obesity) or as complications (DM and high blood pressure).3,8,10,15,23–25 As expected, the proportion of OSA patients suffering high blood pressure (75.9%) is higher than the prevalence of high blood pressure observed in the adult Portuguese population (42%).26 Nevertheless, contrary to what has been suggested by other studies,10,23,24 no association between high blood pressure and OSA severity was found which can be explained by the high proportion of cases with high blood pressure and the reduced number of cases (n=311). Also the high proportion of obesity in our sample27 and the old age of the participants could contribute to this null association as high blood pressure is less associated to severe OSA within older and obese patients.8
The association of male sex, obesity and severe OSA found is compatible with the role of these factors in the pathogenesis of the disease described elsewhere.2
LimitationsAs a limitation, it is important to mention that the study setting and case definition used only permitted us to estimate the proportion of users of primary care suffering from OSA instead of an estimate of the real prevalence of OSA. Despite the large sample size used and its similar demographic structure, when compared to the Portuguese population, the distribution of participating GP does not guarantee a national representativeness of the sample.
ConclusionsAs far as we know, this was the first approach to working out the burden of this disease on the Portuguese population. Our research found a low prevalence of OSA within the Portuguese population aged 25 years and more, which may indicate an underdiagnosis of this health condition.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data. All data analyzed by the research team are anonymized and did not permit to identify any patient.
Right to privacy and informed consentAs only secondary data used in this research, it was not possible to collect write informed consent. Only anonymized data were used and no individual patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
To all the Primary Health Care doctors that participated on this survey.
To Inês Batista for the administrative support needed to realize this study.