I am writing you this letter to present the case of a lady affected by Excessive Dynamic Airway Collapse (EDAC) who subsequently felt better when treated with the simple tool which is explained as follows.
EDAC is defined as the pathological collapse and narrowing of the airway lumen by 50% or more in the sagittal diameter; which is entirely due to the laxity of the posterior wall membrane with structurally intact airway cartilage.1,2
EDAC is usually asymptomatic; when severe, it can cause refractory cough, dyspnea, inability to clear secretions, pneumonia, respiratory failure, and wheezing resistant to drugs.1 A variety of treatment options has been suggested for EDAC, but large controlled studies are needed to confirm their efficacy.2,3
This is the case of a non-smoker 86-year-old woman (JAT) who signed an informed consent form. JAT is a housewife, has no risk factors for respiratory diseases but several comorbidities including anxiety and depression in treatment.
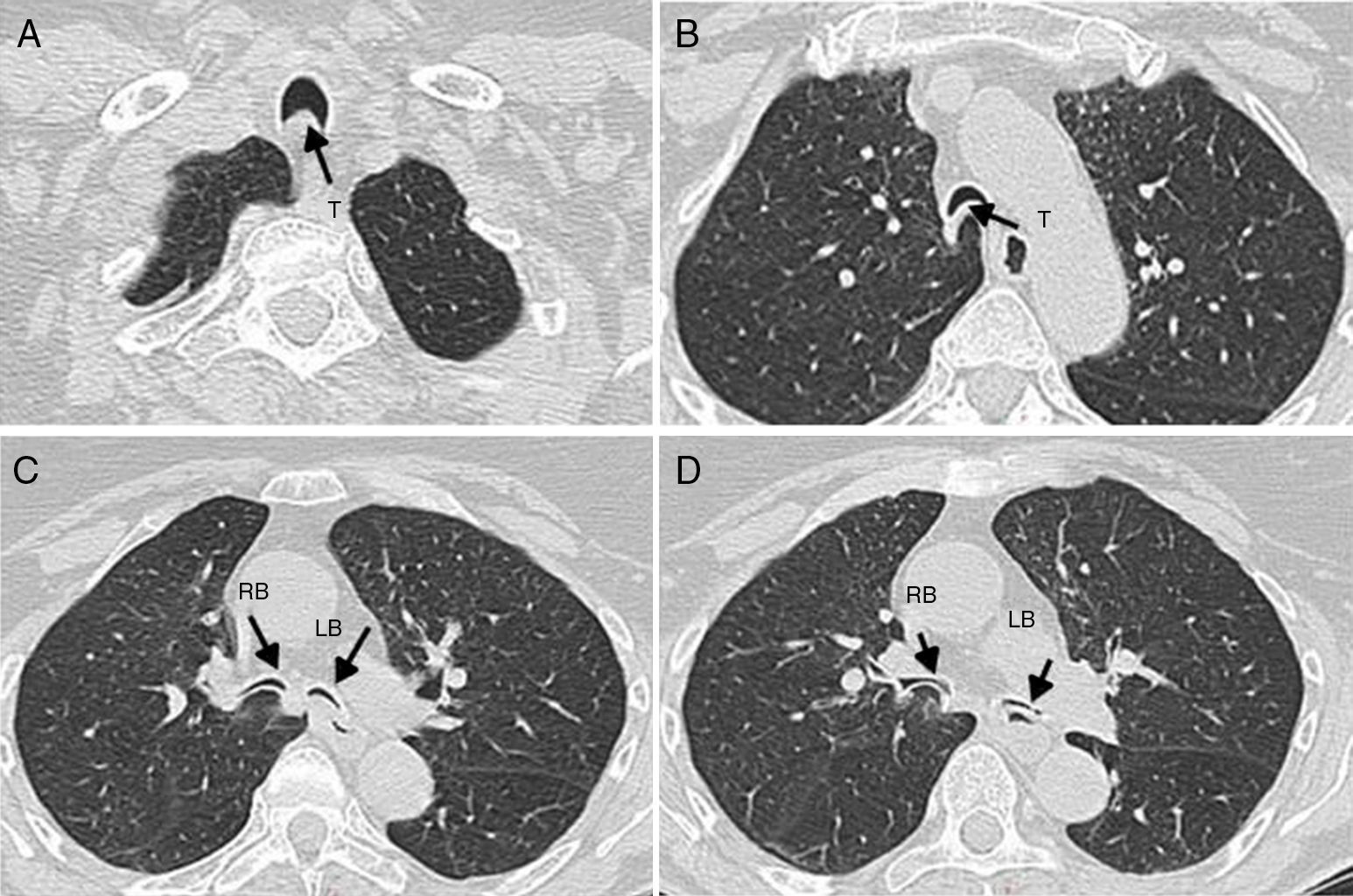
In 2004 she started having dyspnea at rest and orthopnoea, which were attributed to anxiety. At the beginning of 2007 severe EDAC was diagnosed by bronchoscopy (Figs. 1A and 2A–D). The spirometry showed reduction of forced expiratory flow at low lung volumes: Forced Expiratory flow at 25–75% of vital capacity (FEF25-75) was 40% of predicted and complete intrathoracic expiratory flow-limitation during tidal breathing. After Albuterole 400μg forced expiratory flow at low lung volume improved (FEF 25–75 was 49% of predicted value). She started therapy with Formoterol/Fluticasone 6/100μg.
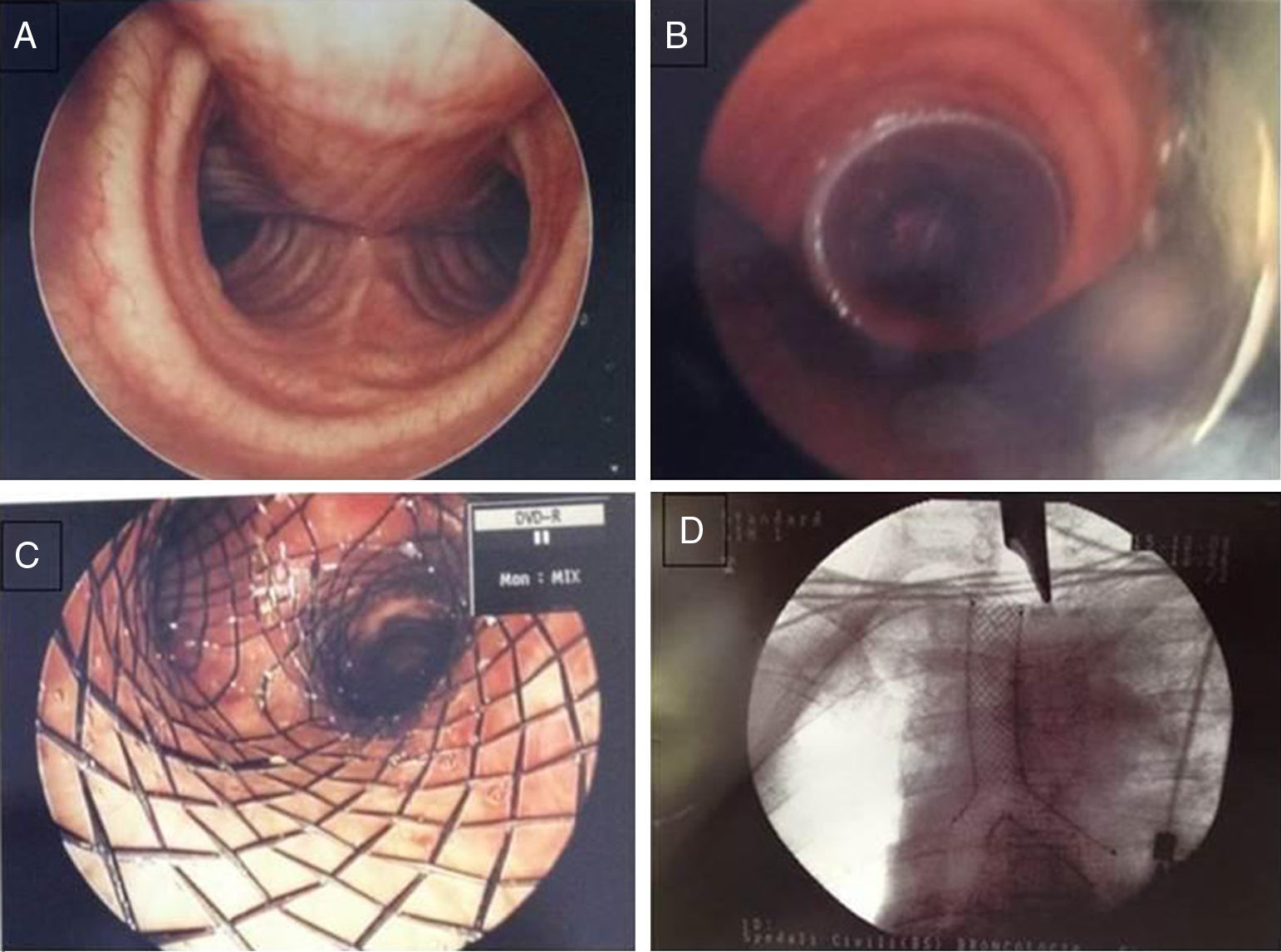
Bronchoscopic images. Panel A: Invagination of tracheal posterior wall membrane during spontaneous breathing in the studied patient with narrowing of tracheal lumen. Panel B: Positioning of endoluminal y silicon stent (Dumon type) in trachea of the studied patient. Panels C and D: Fully covered metal stent (Leufen) placed in trachea of the studied patient.
As it was suggested that nocturnal and intermittent daytime use of CPAP kept the airway opened and improved sputum production in EDAC patients,2,3 nocturnal CPAP (11cmH2O) with facial mask (she could not tolerate nasal mask) was used: sleep quality and orthopnoea improved.
In December 2007 JAT underwent endoscopic laser treatment with poor results and in September 2008 an endoluminal silicone y-stent (Dumon type) was inserted (Fig. 1B), but it was not successful probably because of the migration of the obstruction point toward the periphery of the airways tree.3,5
The following December it was replaced by a fully covered metal stent (Leufen) (Fig. 1C and D), which was removed in February 2009 because of granulation tissue growth and viscous secretion.
The severity of EDAC accordingly to Murgu classification system4 was: F3, E3, S3, M: crescent type, O: idiopathic.
From 2007 to 2009 JAT underwent several bronchoscopies to clear secretions (at least 15); her quality of life (mean EQ-5D score 50) was very poor.
In March 2010 she was admitted to the pulmonary rehabilitation department for respiratory care with:
- –
one daily gym group-session
- –
Joint mobilization/limb training with “unloaded” arm/leg exercise
- –
Airways clearance with threshold-Positive Expiratory Pressure (tPEP), set at 8cmH2O.
CPAP improved sleep quality, but during bike training it was not helpful and severe dyspnea occurred. We then tried to training the arm bike with the application of non-invasive ventilation (NIV) using BPAP Synchrony S/T with inspiratory positive airway pressure 16 and expiratory positive airway pressure 8, with humidification included and facial mask (F&P HC 431). Although there is no evidence that NIV can improve exercise training in EDAC patients, we tried this tool which is commonly used with COPD patients8 to unload respiratory muscles and increase exercise tolerance.
JAT also continued airways clearance exercises (t-PEP) with modest results and in June, she was readmitted to the Pulmonary Rehabilitation department.
We were aware that airway clearance was the major goal to achieve. To the best of our knowledge there are no data on the use of clearing secretions techniques in EDAC. Only positive expiratory pressure is accepted.3
As EDAC is a condition in which airways collapse during forced expiration and cough, treatment modalities for airway clearance that increase inspiratory volume or expiratory flow rate should not be considered.
We tried High Frequency Chest Wall Oscillator (HFCWO – Vest® System, Model 105 – Home Care, HillRom), an inflatable jacket (Vest) worn over the chest connected to an air pulse generator which rapidly inflates and deflates the vest producing oscillations to the chest wall.
The air pulse generator was set at pressure level 2 and frequency 14.
HCFWO alone caused worsening of dyspnea probably because it decreases End Expiratory Lung Volume below the Residual Functional Capacity6 increasing airway resistance. Thus, as suggested by Perry et al.7, we added a positive expiratory pressure using tPEP set at 8cmH2O to maintain airway opened during the oscillations.
While Perry7 used a pressure-cycled ventilator to add a PEEP, we used a tPEP with a mouthpiece to make the treatment easier and more feasible at home for the patient and to facilitate secretions expulsion (which can be difficult when wearing a facial mask). This made the HFCWO very effective and JAT continued the treatment 3 times per day 15min/sessions, achieving stable airway cleaning and improvement of dyspnea.
During the airway clearance program SpO2 was monitored: it did not change from the basal values (i.e. 96–98%).
At discharge The Borg scale of dyspnea improved from 8 to 4 and she declared: “I feel my lungs free of secretion, during the treatment I feel secretions moving upward” The Quality of Life score (EQ-5D) improved from 50 to 85.
No modifications were observed in lung function. HFCWO and tPEP were prescribed at home 3 times per day every day. She kept to the treatment and after 48-month follow-up was still improved. JAT had no side effect from treatment, no more admissions for respiratory symptoms and no need for bronchoscopy.
Even if this tool is not a treatment for the disease, it ensured the patient kept her lungs clear from secretions and improved her dyspnea and quality of life.
We did not study the effects of HFCWO on respiratory system mechanics of this patient and, as EDAC is a rare disease, we could not conduct a randomized trial. Other studies and more patients are needed to verify the effectiveness of this intervention in EDAC.
However, we think that the association of HFCWO and tPEP should be taken into consideration when any other treatment fails with an EDAC patient. This is, in fact, a non-invasive and safe intervention that can be used at home in a self-care regime.
Conflicts of interestThe authors have no conflict of interest to declare.
The Authors acknowledged Michela Bezzi and Flavio Milesi for their clinical contribution and Maria Elena Mino Zabala and Severiana Noguera Borja for their help in the Portuguese translation.