Inspiratory muscular training (IMT) increases the respiratory muscle strength, however, there is no data demonstrating its superiority over the incentive spirometry (IS) in doing so. Values of muscle strength after IMT (Threshold IMT®) and by the IS (Voldyne®) in healthy females was compared. Subjects (n = 40) were randomly divided into control group (CG, n = 14), IS group (ISG, n = 13) and threshold group (TG, n = 13). PImax was measured before (pre-IMT), at 15 and 30 days of IMT. There was an increase in PImax of the TG at 15 days (p < 0.001) and 30 days of IMT (p < 0.001). The same occurred with the ISG, which increased the PImax at 15 days (p < 0.001) and 30 days of training (p < 0.001). After 30 days of IMT, the TG presented a PImax which was significantly higher than ISG and the CG (p = 0.045 and p < 0.001, respectively). It can be concluded that IMT by threshold was more effective in increasing muscle strength than the Voldyne.
The ability to generate inspiratory pressure can be increased by the formation of a pressure threshold. This threshold can be produced by respiratory muscular training (RMT), which increases resistance to muscular fatigue, improves the respiratory function and increases the blood flow redistribution to the muscles.1, 2, 3
The increment in respiratory muscular strength increases the lung capacity in order to offset the increased respiratory load.2, 4 However, there are some points about the RMT which are not clear, such as the mechanisms through which this kind of training improves the performance in the maximal incremental exercise,1 as well as the devices which result in more efficiency.
Among the most commonly used devices for inspiratory muscular training (IMT), Threshold IMT® stands out5, 6, 7, 8: it has been widely used in the implementation of IMT in several clinical situations, with the aim of increasing exercise capacity in chronic obstructive pulmonary disease (COPD),6 in postoperative coronary artery bypass surgery,9 preoperative correction of scoliosis in children with Duchenne muscular dystrophy,10 in post-bariatric surgery11 and weaning from mechanical ventilation.12 In addition, some studies have reported the use of incentive spirometer Voldyne® for purposes of IMT,13, 14 although this feature is based on the supply of non-linear pressure load. It is worth noting, however, there are not many studies that compare the effectiveness of Threshold IMT® compared with Voldyne® as a resource for RMT.13
Authors on this subject consider that the ideal protocol for evaluating the real effectiveness of the IMT has still not been established.15, 16 There is a great diversity in suggested training times and in devices used for such purposes.7, 17, 18, 19 For this reason, the present study aimed to compare the effect of IMT on inspiratory muscle strength (IMS) using the Threshold IMT® device and the Voldyne® in healthy and sedentary subjects.
MethodsThis is a randomized clinical trial, comprised of sedentary and healthy subjects (females) aged between 18 and 40 years, with body mass index (BMI) of less than 25 kg/m2 and normal lung function. Active smokers were excluded, as were subjects that took regular physical activity. The study was approved by the Ethics Committee of the University of Santa Cruz do Sul, RS, Brazil. All the subjects read and signed an informed consent form.
The subjects were allocated from a list of random numbers generated by computer (Random Number Generator – Pro v2.00, Segobit, USA). The randomization sequence was done by a researcher who was directly not involved in the study and the subjects were randomly divided into control group (CG), threshold group (TG) and incentive spirometry group (ISG). Afterwards, the lung volumes were measured by a spirometer (EasyOne®, model 2001, Zurich, Switzerland) for the analysis of forced vital capacity (FVC), forced expiratory volume in the first second (FEV1) and peak expiratory flow (PEF).20 The best curve was compared with the predicted values in the literature.21 The anthropometric characteristics of the subjects were also assessed.
The PImax was evaluated with a digital pressure manometer (MDI® model MVD300, Porto Alegre, Brazil) having been obtained with the individual breathing in from residual volume (RV) to total lung capacity and effort was made against the occluded valve, with the measurements carried out in the sitting position.22 The figure considered for data analysis was the highest value among the three maneuvers, if it did not differ more than 10% from the second highest value in descending order.22 To evaluate the effect of the IMT, the PImax was measured at pre-training (pre-IMT), after 15 days and after 30 days.
The IMT was performed with the Threshold IMT® (Respironics New Jersey, Inc., USA) and with an incentive spirometry (IS) with a volume-oriented device (Voldyne 5000®, Sherwood Medical, St. Louis, USA). CG performed breathing exercises twice.23 Blinding was strictly maintained; the team that carried out the review was not informed about which type of device was being used by the participants not were the participants informed about the device or the form of training used by the other group.
Inspiratory muscle training protocol with Threshold IMT®The TG participants were instructed to perform IMT with the Threshold® twice a day, three times a week on non-consecutive days during the 30-day period. There was a series of six repetitions with an initial resistive load of 40% of the PImax. Evaluations of the PImax were not carried out in the first week of IMT to ensure the subjects were familiarized with the established protocol. After this period the PImax measurements were performed weekly with the aim of increasing the resistive inspiratory pressure so as to achieve the training effect. The incremental load was 10% of the PImax per week or enough to reach the maximum resistive value of the Threshold IMT®, which is 41 cmH2O.4, 13
Inspiratory muscle training protocol with Voldyne®The subjects of the ISG were instructed to perform maximal inspiration from RV to TLC with Voldyne® in the sitting position.24 The expiration was performed at functional residual capacity in order to avoid possible hyperventilation; there were intervals of 60 s between respiratory maneuvers.25 All subjects received verbal commands as to exactly when to start a new inspiration. The Voldyne® was used for 20 min (20 repetitions or one repetition per minute). The total time of this program was 30 days, twice a day, three times per week on nonconsecutive days.
Breathing exercises protocolThe breathing exercise performed by GC was performed 02 times per day with 03 sets of 20 repetitions with a pause of 02 min between each set, 03 times a week for 30 non-consecutive days. In this breathing exercise the individual performs diaphragmatic inspiration from functional residual capacity to maximum inspiratory lung volume with 02 consecutive breaks, while maintaining a ratio of 02 to 01 breaths.23
Statistical analysisThe SPSS (version 20.0, USA) was used for the analysis of the results which were presented as mean and standard deviation and the normal distribution observed by Shapiro–Wilk test. The data referring to anthropometric variables and to pulmonary function were compared between groups by one-way ANOVA followed by Tukey post hoc. The behavior of the PImax in the different groups with two-way ANOVA followed by Bonferroni multiple comparison and the interaction of the FEV1 with the PImax by ANCOVA were also observed. Statistical significance of p < 0.05 was used.
ResultsThe subjects were distributed into CG (n = 14), TG (n = 13) and ISG (n = 13) and their characteristics (baseline) are presented in Table 1. The sample being studied was found to be homogeneous, except for the FEV1, however, all subjects had values which were close to those predicted.
Table 1. Baseline characteristics of the participants from groups studied.
| Groups | p-Value | |||
| Control (n = 14) | Threshold (n = 13) | Incentive spirometry (n = 13) | ||
| Antropometrics | ||||
| Age (years) | 23.86 ± 3.32 | 22.92 ± 2.06 | 21.92 ± 1.44 | 0.101 |
| Weight (kg) | 58.07 ± 9.13 | 60.15 ± 8.65 | 58.69 ± 7.76 | 0.813 |
| Height (m) | 1.66 ± 0.06 | 1.68 ± 0.06 | 1.68 ± 0.08 | 0.860 |
| BMI (kg/m2) | 20.29 ± 2.36 | 20.85 ± 1.72 | 20.31 ± 2.05 | 0.736 |
| Lung function | ||||
| FVC (%pred) | 95.14 ± 8.95 | 102.77 ± 11.86 | 93.77 ± 12.34 | 0.096 |
| FEV1 (%pred) | 97.50 ± 9.82 | 104.77 ± 11.24 | 94.31 ± 10.33 | 0.048 † |
| PEF (%pred) | 94.14 ± 16.62 | 102.23 ± 17.60 | 90.69 ± 18.79 | 0.146 |
| Respiratory muscular strength | ||||
| PImax (%pred) | 102.00 ± 6.13 | 101.62 ± 8.46 | 100.62 ± 6.94 | 0.878 |
BMI: body mass index; FVC: forced vital capacity; FEV1: forced expiratory volume in the first second; PEF: peak expiratory flow.
† Significant difference between threshold group and incentive spirometry group (p = 0.042).ANOVA test with Tukey post hoc. Significance was accepted at p < 0.05.
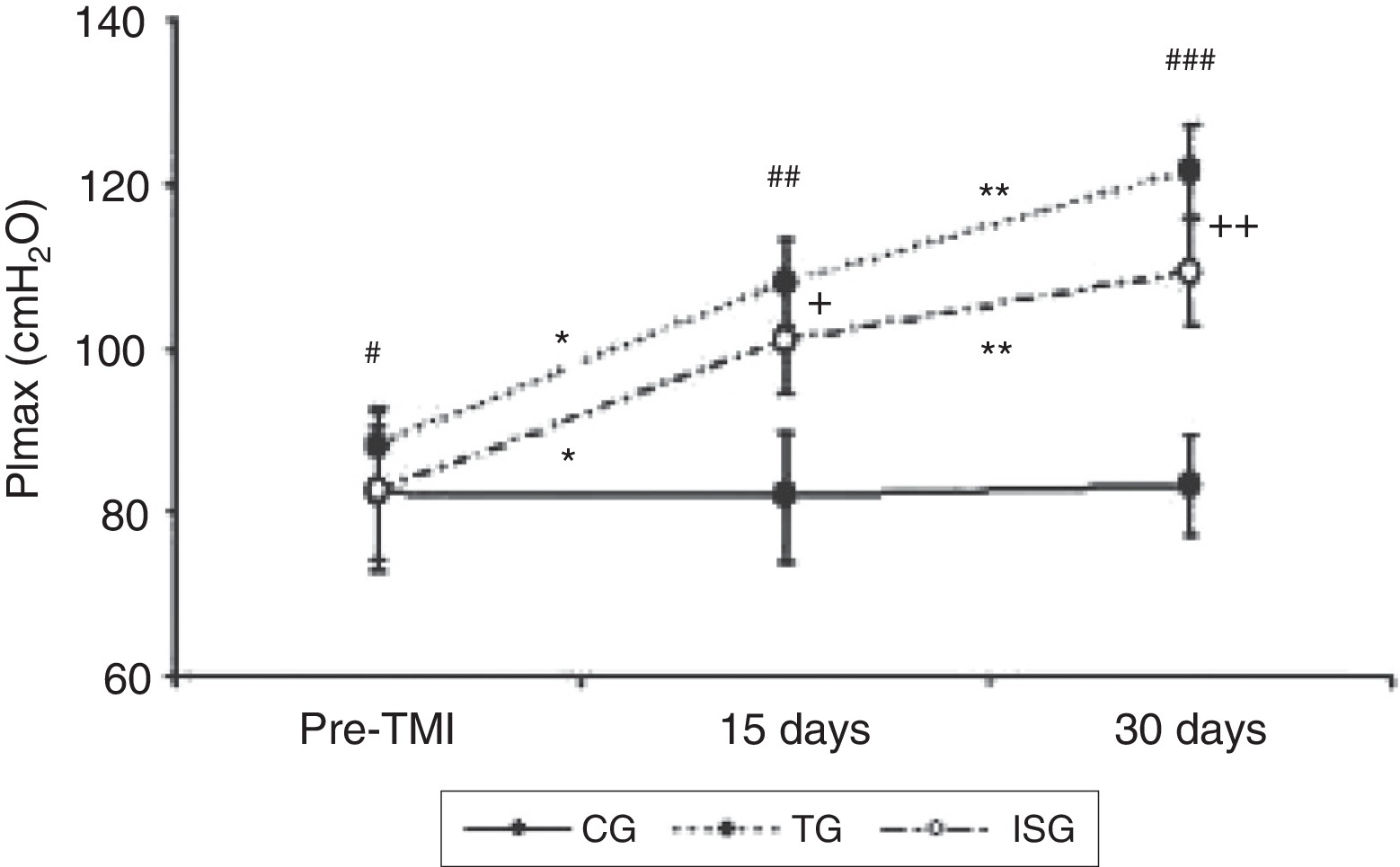
In relation to IMT, there was a significant increase in the PImax in both TG and ISG at 15 days (p < 0.001 and p < 0.001, respectively) and at 30 days (p < 0.001 and p < 0.001, respectively) compared to the pre-IMT. When comparing the effect of IMT between ISG and TG, it was observed that it was only at 30 days was there a higher gain of the PImax by the subjects of the TG in comparison to the subjects of the ISG (p = 0.045) (Figure 1). There was no increase in PImax at 15 (p = 0.988) or 30 days (p = 0.942) for CG compared to the pre-IMT. In addition, no interaction was observed between the FEV1 (p = 0.208) and the PImax.
Figure 1. Effects of inspiratory muscular training in groups studied. Comparison between pre-IMT at 15 days in threshold group – TG (*p < 0.001) and incentive spirometry group – ISG (*p < 0.001), and at 30 days in TG (**p < 0.001) and ISG (**p < 0.001). Comparison between the three groups in pre-IMT (#p = 0.494), 15 days (##p < 0.001) and 30 days (###p < 0.001) conditions. Difference between the TG and ISG at 15 days (+p = 0.328) and at 30 days (++p = 0.045). CG: control group; TG: threshold group; ISG: incentive spirometry group. ANOVA two-way test followed by Bonferroni multiple comparison. Significance was accepted at p < 0.05.
DiscussionOur findings showed an increase in the PImax caused training by Voldyne® and Threshold IMT®, although the latter device was more effective in increasing the IMS after 30 days of IMT. Traditionally the Threshold IMT® is the device used for respiratory muscle training as it provides linear pressure load with the possibility of gradual increments.26
Due to the visual feedback the IS with a volume-oriented device encourages the following; the performance of the subject, the realization of sustained maximal inspiration and hyperpneia aiming to gain pulmonary volume.27 It is known that maximum inspiration causes the increase of the transpulmonary pressure and the increase of the pulmonary volume. Furthermore, resting at the end of inspiration keeps up the increase of the transpulmonary pressure and ensures the alveolar stability.28
The literature provides for the use of specific inspiratory incentive guidelines in accordance with the norms of the American Association for Respiratory Care; its use is prioritized as part of prophylactic regimens routine and therapeutic respiratory care.29 However, it should be noted that such devices are rarely used for IMT, which means a lack of empirical standardization.
This research showed that the IMT instituted through the Threshold IMT® caused an increase in the PImax after 15 and 30 days of training. Our findings are confirmed by other studies which suggest the effectiveness of Threshold IMT® in promoting gains in the IMS.6, 30 Volianitis et al. used IMT for 11 weeks in females rowing athletes and noted an increase in the PImax and in performance during exercise. They have demonstrated that the applicability of the Threshold IMT® is useful not only in clinical approaches but also in improving physical performance.31 Likewise, Gosselink et al. have highlighted that the effects of IMT includes delay in respiratory muscle fatigue, redistribution of the blood flow to the respiratory and locomotor muscles and reduction of the perception of discomfort of the respiratory muscles. However, the mechanisms associated with such effects are not very clear.32
Regarding to the use of Voldyne® was found an increase of PImax in the end of 15 and 30 days of training. Reinforcing our findings, some studies show that the use of this type of IS increases the IMS due to the increased recruitment of the motor units, resulting in greater respiratory muscle strength.33, 34 However, it should be noted that in clinical practice, this feature is not used for IMT, but as a resource for obtaining pulmonary volume gain.
The IS enables the mobilization of large pulmonary volumes and it is also responsible for increasing the intra-alveolar pressure at the end of inspiration. This condition improves breathing capacity, and challenges the patient with the visual stimulus generated by the device.35, 36, 37, 38 The increase of the intra-alveolar pressure is proportional to the contractile force of the respiratory muscles, including the diaphragm and accessory muscles of the respiration, justifying the fact that to achieve the TLC, intense muscle activity should occur.39
It is worth noting that in order to perform breathing exercises with an IS, the subjects mobilize large tidal volume associated with a low respiratory rate, tending to increase muscle strength due to increased inhalation/exhalation ratio.27
Putting together our findings, the results of this investigation demonstrate the relevance of the Threshold IMT® in producing training effect on the inspiratory muscles, as the gain in the muscle strength is proportional to the applied load. According to Komi, changes in the muscular strength during short periods of training with incremental load appear to be due to the improvement of intra- and inter-muscular neural adjustment.40 These mechanisms allow better synchronization in the frequency of neuromuscular firing, resulting in greater activation of the motor units.41, 42
It is important to consider that the subjects of the CG did not significantly change the PImax with time. This fact demonstrates that the breathing exercise alone is not effective in increasing the IMS. A study of asthmatic children also found that a IMT program using the Threshold® IMT significantly increased PImax, which did not happen with the group that only followed a therapeutic exercise program and conventional education for children with asthma.43 This demonstrates that breathing exercises alone are not sufficient to produce significant gain in muscle strength and when applied in isolation do not impose a resistive load on the inspiratory muscles.
There are some limitations to our investigation that need to be considered. We used a volitional test of generation of pressure (PImax) instead of an electrically evoked potential test for the assessment of muscle strength, only healthy subjects were tested and it is not possible to correlate this experimental situation directly with clinical situations involving patients. Only healthy female subjects were available; there was no male representation. Care should also be taken in comparing the effectiveness of these devices, since the training protocols and intensities of training may differ. It is recognized that the physiological effects of the training are related to its intensity. The differences between the training groups are probably related to the intensity and protocols, and the difference seen at 30 days, with better outcomes in the threshold group could also reflect the growing intensity of the training in this group.
In conclusion, our results showed that the Voldyne® device, as well as promoting its known benefits in increasing lung volume, at the same time promotes a similar increased muscle strength to Threshold IMT® device, which is designed specifically for the purpose of TMI. However, after 30 days of training increased PImax caused by Threshold IMT® became more evident.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
☆ Study conducted at the Laboratory Methods and Evaluation Techniques of the Physiotherapy Course of the University of Santa Cruz do Sul – Rio Grande do Sul, Brazil.
Received 27 February 2014
Accepted 24 May 2014
Corresponding author.