Amyotrophic Lateral Sclerosis (ALS) is a fatal, progressive, neurodegenerative disease. When Respiratory failure is too severe to be corrected with Non Invasive Ventilation and/or when bronchial secretions cannot be managed with noninvasive techniques, tracheostomy and invasive mechanical ventilation (IV) are an option.1
Tracheostomy ventilation significantly prolongs survival in ALS patients without effect on the disease progression. For this reason, patients with IV experience a worsening of disability and an increment of the dependency with a severe impairment of their quality of life.2 One of the most important aspect of the multidisciplinary approach in ALS is to guarantee as long as possible the maintenance of the residual functions. In this context, the first and most widely used strategy to allow tracheostomized patients without severe bulbar involvement to speak is the simple cuff deflation, but, in a percentage of these patients, this technique fails with the consequent impossibility of verbal communication and a severe reactive mood depression.3
Intermittent Abdominal Pressure Ventilation consists of an elastic inflatable bladder incorporated within a corset surrounding the abdomen. With bladder inflation by a ventilator, the abdominal content and diaphragm move upward, assisting expiration. With bladder deflation, inspiration occurs passively. There have been only scattered reports on the use of IAPV4–7 and two publications concerning its use in large populations of patients, in a regimen of noninvasive8 and invasive9 ventilator support.
A 49 years old man with a diagnosis of definite ALS, according to El Escorial Criteria, was admitted for the first time to our Centre, having recently had tracheostomy and gastrostomy done because of worsening in respiratory function and swallowing, The patient complained of difficulty using home IV device and difficult management of the secretions. NIV was introduced in Spring 2014 after onset of wheezing during hospitalization in an intensive care ward of an other Centre. The patient reported intermittent use of non invasive ventilation due to poor tolerance until Autumn 2014. At that time there was a significant worsening of respiratory involvement due to a right lung pneumonia associated to weight loss and deterioration of swallowing and dysphagia.
During the hospitalization, we optimized both IV and secretion clearance by cough machine through the tracheostomy tube in association with tracheal aspirations. He could not sustain the spontaneous breathing, so, to permit speech, we introduced diurnal tracheal open ventilation (TOV) with cuff deflation and the concomitant usage of a speaking valve, but with poor patient tolerance due to discomfort with the unnatural experience of air coming in the upper airways and poor synchrony with the ventilation. The patient could not even manage secretions and saliva. Thus, to increase the feasibility and pleasure of speaking during mechanical ventilation and improve breathing comfort we introduced diurnal IAPV (Pneobelt™) associated with a tracheostomy speaking valve for spontaneous breathing. During tracheal ventilation, our patient was fitted while supine, with the corset's horizontal upper border approximately two finger breadths below the costophrenic junction. Once positioned, the patient was placed in a wheelchair, his cannula wad deflated and a speaking valve was placed. Pneobelt™ was connected to the same portable ventilator used for tracheal ventilation but set with parameters “ad hoc”for IAPV.
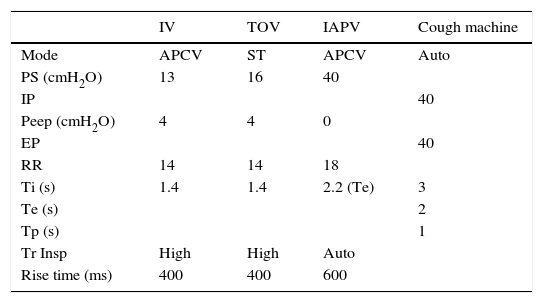
Table 1 shows IV, cough machine and IAPV settings (Fig. 1) shows Pneobelt™ with the corset and inner bladder.
Ventilation and cough machine settings (PS: pressure support; IP: inspiration pressure; EP: expiration pressure; RR: respiratory rate; Ti: inpiratory time; Te: expiratory time; Tp: pause time; Tr Insp: inspiratory trigger; IV: invasive ventilation; TOV: tracheal open ventilation; IAPV: intermittent abdominal pressure ventilation; APCV: assisted pressure-control ventilation; ST: spontaneous timed).
| IV | TOV | IAPV | Cough machine | |
|---|---|---|---|---|
| Mode | APCV | ST | APCV | Auto |
| PS (cmH2O) | 13 | 16 | 40 | |
| IP | 40 | |||
| Peep (cmH2O) | 4 | 4 | 0 | |
| EP | 40 | |||
| RR | 14 | 14 | 18 | |
| Ti (s) | 1.4 | 1.4 | 2.2 (Te) | 3 |
| Te (s) | 2 | |||
| Tp (s) | 1 | |||
| Tr Insp | High | High | Auto | |
| Rise time (ms) | 400 | 400 | 600 |
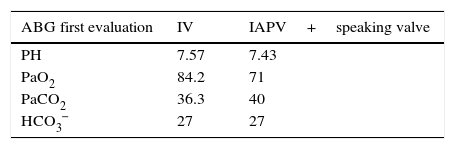
The use of IAPV permitted optimal speech, an efficient diurnal ventilatory pattern, good pulmonary gas exchange (Table 2), without dyspnoea and with a significant improvement of the salivary secretions’ management and a decrease in the tracheal aspiration need.
At time of discharge, our patient maintained IAPV for 3–4h/day, while he was in a wheelchair, with great compliance to treatment. He felt his breathing was “normal, like before tracheostomy”. To guarantee a safe discharge we trained the caregivers in the proper respiratory management and periodic supervision calls were made.
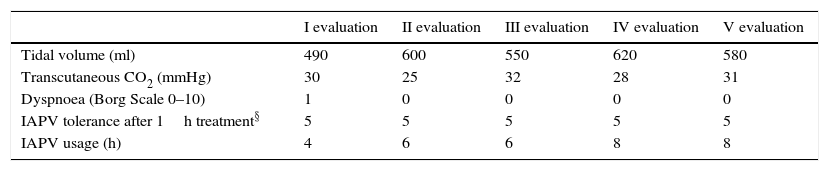
Table 3 shows the clinical follow-up of the patient performed every 3 months. Moreover, over time we checked the reappearance of a spontaneous respiratory activity without any need for ventilatory support. Nowaday our patient can maintain the spontaneous breathing for almost 2h, without dyspnoea or tachipnoea. No major technical problems or adverse effects due to IAPV use were reported.
Respiratory assessment during IAPV (intermittent abdominal pressure ventilation)(§: 5 point scale; 1 poor tolerance–5 optimal tolerance).
| I evaluation | II evaluation | III evaluation | IV evaluation | V evaluation | |
|---|---|---|---|---|---|
| Tidal volume (ml) | 490 | 600 | 550 | 620 | 580 |
| Transcutaneous CO2 (mmHg) | 30 | 25 | 32 | 28 | 31 |
| Dyspnoea (Borg Scale 0–10) | 1 | 0 | 0 | 0 | 0 |
| IAPV tolerance after 1h treatment§ | 5 | 5 | 5 | 5 | 5 |
| IAPV usage (h) | 4 | 6 | 6 | 8 | 8 |
To the best of our knowledge, this case describes for the first time the use of IAPV in a tracheostomized ALS patient, a noninvasive ventilation mode that functions primarily by exerting force on the abdomen and indirectly causing motion of the diaphragm. As reported in the Literature we confirm that IAPV is simple to use, portable and without particular side effects related to its daily use.
A respiratory rehabilitative treatment for ALS tracheostomized patients should consist in optimizing IV and secretion management with cough machine and in verifying spontaneous respiratory trials, TOV and speaking valve use both during ventilation and spontaneous breathing.3 In 1988, Miller et al., in a large, high quadriplegic patient series with tracheostomies, reported that the advantages if IAPV use included plugging of the tracheostomy tube. With IAPV speech was easier and louder.9 Our patient had a good speaking competence, but serious difficulties to manage secretions and saliva during TOV. So, to optimize speech, we introduced the diurnal use of IAPV.
In our centre tracheostomy is proposed only for patients with severe bulbar involvement, because the indication for tracheotomy should be dependent on glottic function rather than on inspiratory or expiratory muscle failure,1 but this patient arrived in our department having already had a tracheostomy. In our practice, ALS patients are not decannulated, to avoid the risk of near re-intubation due to disease progression and, or new episodes of acute respiratory distress syndrome; other authors,10 instead, propose the use of continuous volume-cycled NIV and cough machine with oximetry feedback in ambient air to permit safe extubation of unweanable ALS non bulbar patients. Our combined, ventilatory approach with tracheal invasive ventilation and IAPV has guaranteed optimal speech and a safe respiratory management with an optimal patient acceptance of treatment. Furthermore, there has been spontaneous breathing activity, which demonstrates an improvement in the patient's respiratory condition. IAPV facilitates diaphragmatic motion and may be particularly useful in patients with bilateral diaphragmatic weakness or paralysis and permits plugging of the tracheostomy tube with cuff deflation for several hours during the day, with prevention of tracheal damage.
Our case suggests that Pneumobelt can be a safe and effective method of daytime ventilation, and, by improving speech and secretion management, it permits a better quality of life even in a tracheostomized ALS patient.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors declare no financial support for the conduct of the study.