Diffuse alveolar haemorrhage (DAH) is a rare, life-threatening syndrome, characterized by progressive alveolar infiltrates, anaemia and haemoptysis. DAH is a medical emergency, requiring prompt identification and treatment, but this may be hindered by an absence of haemoptysis or non-acute presentation. A comprehensive search for the underlying cause is imperative, as this will guide any effective treatment. It is important to note that different aetiologies are associated with specific pathogenesis. We describe the case of a patient with malignant hypertension (MH) presenting with DAH, we review previous reports on this association and discuss the implications on the pathogenesis and clinical management of DAH.
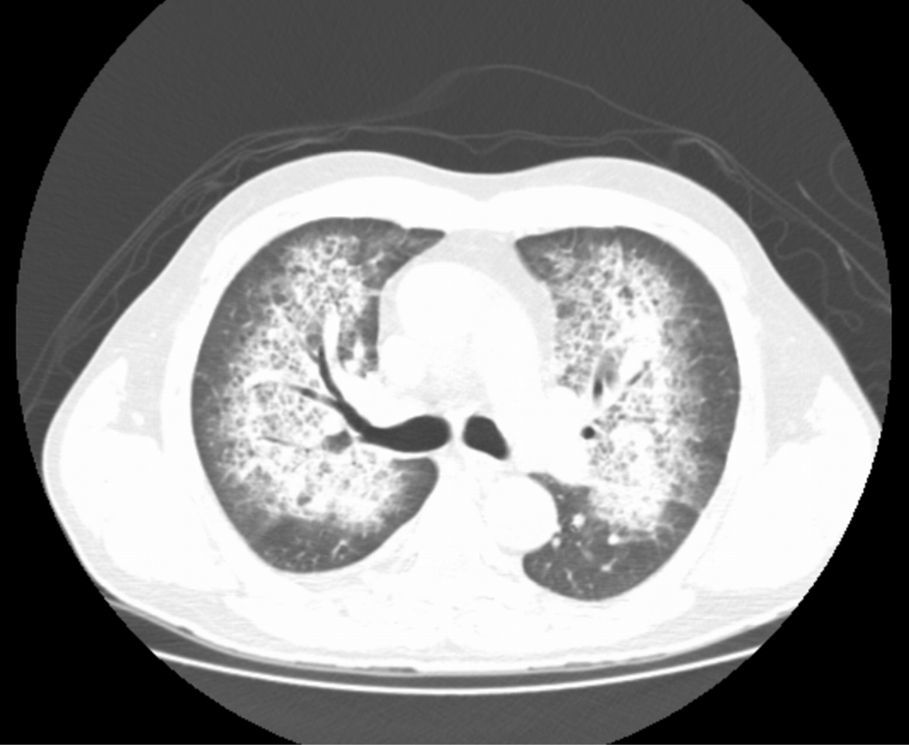
A 51-year-old male presented with a dry cough and mild dyspnoea which had lasted four days. He was a financial consultant, a heavy smoker and had a history of chronic sinusitis but without any prescribed medication. The physical examination revealed no signs of respiratory distress, a bilateral blood pressure (BP) of 220//130mmHg, and left basal crackles. An echocardiography revealed signs of mild aortic, mitral and tricuspid regurgitation and a chest X-ray showed bilateral perihilar “butterfly pattern” alveolar infiltrates. Blood tests showed severe renal failure, hypokalaemia and normocytic anaemia (creatinine: 8.02mg/dL (reference values (RV): 0.72–1.18), potassium: 2.0mmol/L (RV: 3.5–5.1), haemoglobin: 11.2g/dL (RV: 13.0–17.0)). Laboratory coagulation tests were normal (prothrombin time: 16.2s (RV: 12.0–17.4), prothrombin 77% (RV: 70–120)). An arterial blood gas analysis showed respiratory alkalosis with a PaO2 level of 63mmHg (RV 83–108). A non-contrast chest CT found bilateral central parenchymal infiltrates with a “crazy paving” pattern (Fig. 1) and a renal ultrasound found bilateral increased kidney echogenicity with preserved size. A bronchoscopy with bronchoalveolar lavage was performed, and progressively bloody fluid was retrieved. Urinalysis showed microscopic haematuria and proteinuria (+++) with a spot urine sample protein to creatinine ratio of 2380mg/g (RV: <200). Fundoscopic examination identified signs of hypertensive optic neuropathy, and the patient was admitted for malignant hypertension, under aggressive anti-hypertensive therapy. He remained stable and the pulmonary infiltrates improved, but poor renal function and difficult hypertension continued. Further study revealed cytoplasmic iron deposits in alveolar macrophages with a moderate alveolar haemorrhage but no signs of pulmonary infection. The auto-immune panel was negative, including anti-nuclear antibodies, proteinase-3-antineutrophil cytoplasmic antibodies, myeloperoxidase-antineutrophil cytoplasmic antibodies, anti-glomerular basement membrane antibodies, cryoglobulins and rheumatoid factors. Complement levels were normal and viral serologies were negative. The plasma renin was 1090μU/ml (RV: 7–76), aldosterone was 5660pg/ml (RV: 30–310), and aldosterone to renin activity ratio was 6.3ng/ng (RV: 14.5). An abdominal CT scan revealed a left adrenal nodule and a renal eco Doppler excluded renal artery stenosis. An ultrasound guided kidney biopsy was performed revealing hypertensive nephroangiosclerosis with chronic interstitial nephritis and arterio-sclerosis and arteriolo-sclerosis. There was no evidence of active necrotizing glomerulonephritis, crescent formation, immune deposits or vasculitis. The procedure was complicated by late bleeding and renal haematoma requiring embolization of the left renal artery. After the embolization, normalization of blood pressure and potassium levels were noted. A new evaluation of plasma renin and aldosterone levels showed normal results. The patient became asymptomatic; there was complete resolution of pulmonary infiltrates and hypoxaemia, but no recovery of renal function, requiring chronic haemodialysis. The final diagnosis was probable adrenal reninoma, leading to malignant hypertension, diffuse alveolar haemorrhage and chronic renal failure.
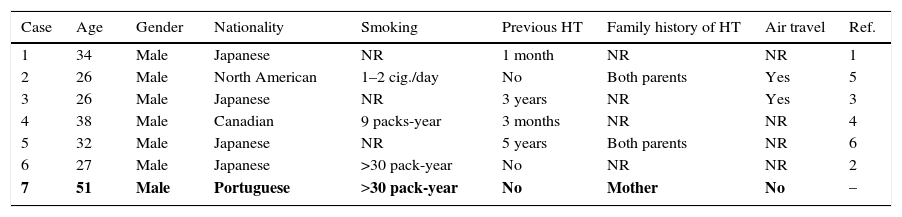
We report a patient with a probable reninoma leading to severe systemic hypertension and subsequent diffuse alveolar haemorrhage. Although we could not get histological confirmation of the reninoma, the left adrenal node, strikingly elevated levels of renin and prompt pressure response to the embolization procedure suggest that this was the cause of the hypertension. Malignant hypertension can be defined as extremely high blood pressure with associated papilledema. The pathogenesis of MH is poorly understood but disturbances in the renal release of vasoconstrictors and mechanical stress on vessels’ walls appear to be critical. This is the seventh report on malignant hypertension-associated DAH. The main characteristics of this one and of the previous reports are described in Table 1. This possible new syndrome displays some striking characteristics: all patients are, relatively young, males, with 4 out of 7 were smokers. There was also a predominance of Asians. Since the incidence of malignant hypertension is not increased in males, there may be some relevance to this gender predominance.
Clinical characteristics of all reports of malignant hypertension with diffuse alveolar haemorrhage.
| Case | Age | Gender | Nationality | Smoking | Previous HT | Family history of HT | Air travel | Ref. |
|---|---|---|---|---|---|---|---|---|
| 1 | 34 | Male | Japanese | NR | 1 month | NR | NR | 1 |
| 2 | 26 | Male | North American | 1–2 cig./day | No | Both parents | Yes | 5 |
| 3 | 26 | Male | Japanese | NR | 3 years | NR | Yes | 3 |
| 4 | 38 | Male | Canadian | 9 packs-year | 3 months | NR | NR | 4 |
| 5 | 32 | Male | Japanese | NR | 5 years | Both parents | NR | 6 |
| 6 | 27 | Male | Japanese | >30 pack-year | No | NR | NR | 2 |
| 7 | 51 | Male | Portuguese | >30 pack-year | No | Mother | No | – |
HT: systemic hypertension; cig.: cigarette; NR: no reference; Ref.: reference.
These reports suggest that extreme hypertension can lead to pulmonary haemorrhage, similar to pulmonary renal syndrome caused by an immune-mediated mechanism. The mechanism of how high blood pressure can cause alveolar haemorrhage remains unclear, but humoral factors1 might be involved in the alveolar capillaries. The damaged endothelium increases permeability and activates the coagulation cascade, including platelet activation and fibrin deposition. Red blood cells are destroyed within vessels,2 which may explain why up to one-third of patients do not present with haemoptysis. Hida et al.,1 argued that alveolar capillaries might be injured by malignant hypertension in the same way as systemic capillaries. However, Sato et al.3 and Aithal et al.4 concluded that left ventricular dysfunction resulting from systemic hypertension can cause pulmonary oedema, leading to haemorrhage. On the other hand, Dalal et al.5 showed that smoking, platelet dysfunction due to underling uraemia and thrombocytopenia may also predispose to development of pulmonary haemorrhage. Sato et al.3 and Dalal et al.5 suggest that previous air travel may have contributed to the development of DAH, with an underlying mechanism similar to high altitude pulmonary oedema. However, it is worth noting that no other findings have supported this hypothesis, and this may be just a non-significant association. In conclusion, our and previous reports of malignant hypertension associated DAH suggest that high blood pressure may be a significant cause of alveolar haemorrhage. Clinicians caring for DAH patients should be aware of this association. We also propose large-scale studies on the association between systemic blood pressure and the risk of alveolar haemorrhage which could open the way to new treatment of DAH with BP lowering agent.
DisclosureThe authors report no financial support, off-label or investigational drug use.
Conflicts of interestThe authors have no conflicts of interest to declare.