Continuous positive airway pressure (CPAP) is frequently used to treat patients with acute respiratory failure in out-of-hospital settings. Compared to a facemask, the helmet has many advantages for the patient but requires a minimum gas flow of 60 L/min to avoid CO2 rebreathing. The aim of the present bench study was to evaluate the performance of four Venturi devices, connected to a single oxygen cylinder, in delivering helmet-CPAP with clinically relevant gas flow, fraction of inspired oxygen (FiO2), and positive end-expiratory pressure (PEEP) values.
MethodsThree double-inlet Venturi systems (EasyVent, Ventuplus, Compact-HAR) were connected to full 5-L oxygen cylinders using a double flowmeter, and their oxygen requirements to reach different setups (flow 60-80 L/min; FiO2 0.4-0.5-0.6, PEEP 7.5-10-12.5 cmH2O) were tested. The fourth Venturi system (O2-MAX) was directly attached to the tank, and the flow and FiO2 delivered at preset FiO2 0.3 and 0.6 were recorded. The runtime of the cylinder was assessed.
ResultsEasyVent, Ventuplus, and O2-MAX were able to deliver helmet-CPAP with clinically useful setups when connected to a single oxygen cylinder, while Compact-HAR did not. The runtime of the cylinders ranged between 28 and 60 minutes according to the preset flow and FiO2. The delivered gas flow decreased slowly and linearly with the drop in cylinder pressure until its exhaustion.
ConclusionsHelmet-CPAP might be provided using portable Venturi systems connected to an oxygen cylinder, but not all of them are able to deliver it. The use of a double flowmeter allows delivery of both high flow and high FiO2 when double-inlet Venturi systems are used. Due to the flow drop observed during the cylinder consumption, a flow >60 L/min should be set when helmet-CPAP is started. Considering the flow drop phenomenon, the estimated duration of the tank runtime can be used with a margin of safety when planning patient transport.
Continuous positive airway pressure (CPAP) is used to treat acute respiratory failure (ARF) and can be administered via facemask or helmet.1,2 Due to its simple use and the availability of compact devices connectable to an oxygen cylinder, facemask-CPAP is frequently employed in ARF patients both in the pre-hospital setting and during patient transport.3–8
Helmet-CPAP (H-CPAP) reduces air leaks and skin damage and is better tolerated by patients,9 however, its out-of-hospital use is limited by its high gas flow requirements. Indeed, ≥60 L/min of gas flow are necessary to safely deliver H-CPAP, both to prevent carbon dioxide rebreathing and to exceed the patient's peak inspiratory flow, thus maintaining a stable positive airway pressure.10–12
Several flow generators, exploiting the Venturi effect, to deliver pre-hospital H-CPAP should be able to generate an adequate gas flow, together with an FiO2 and positive end-expiratory pressure (PEEP) appropriate for ARF patients.2,11,12 These Venturi systems, connectable to an oxygen cylinder, are user friendly, and cost-effective, however, their performance in terms of gas flow, FiO2, and PEEP remains unclear.
A previous bench study compared two H-CPAP portable Venturi devices.12 They were connected to a single oxygen tank able to deliver a maximum of 15 L/min of O2 through the primary oxygen inlet of the device. According to the Venturi effect, as the O2 flow from the tank increased, the delivered gas flow in the circuit increased, but the resulting FiO2 decreased to values often inadequate for ARF patients. To overcome this limitation, double-inlet Venturi systems equipped with a second O2 inlet have been developed. This allows to increase FiO2 of the gas mixture but requires an additional oxygen cylinder. To avoid the use of two oxygen tanks, which are impractical for out-of-hospital settings, a novel and easy solution could be connecting a double flowmeter to a single oxygen cylinder. Moreover, in addition to double-inlet Venturi systems, new cylinder-attachable Venturi devices with predefined FiO2 settings are nowadays available on the market.
This bench study aims to assess the feasibility of H-CPAP using either double-inlet portable Venturi systems connected to a single oxygen cylinder via a double flow meter, or a cylinder-attachable Venturi device. The primary endpoint was to evaluate the effectiveness of different portable Venturi systems in delivering H-CPAP with clinically adequate gas flows, FiO2, and PEEP values. The secondary endpoint was to evaluate their efficiency, defined as duration of the oxygen cylinder.
MethodsFour commercially available, portable Venturi flow generators designed for the delivery of H-CPAP in the out-of-hospital setting were studied (Fig. 1).
1: DEVICE-1, EasyVent [Dimar. Medolla. Modena. Italy]; 2: DEVICE-2, Ventuplus [StarMed. Mirandola. Modena. Italy]; 3: DEVICE-3, Compact-HAR [Harol S.r.l. San Donato Milanese. Milan. Italy]; 4: DEVICE-4, O2-Max (Pulmodyne. Indianapolis. USA). Photographs taken by the authors with permission of the manufacturers.
DEVICE-1 (EasyVent, Dimar, Medolla, Italy), DEVICE-2 (Ventuplus, StarMed, Mirandola, Italy) and DEVICE-3 (Compact-HAR, Harol S.r.l., San Donato, Italy) are Venturi flow generators equipped with two oxygen lines: Line-A, connected to a primary oxygen source constitutes the main flow; Line-B, located downstream from the air entrainment valve, linked to a supplementary oxygen source, provides an oxygen enrichment flow, increasing the FiO2 of the delivered gas mixture. DEVICE-4 (O2-Max, Pulmodyne, Indianapolis, USA) has a single inlet port directly connectable to a single oxygen source. It offers three preset FiO2 values (0.3-0.6-0.9), whereas the flow cannot be adjusted. The gas flow declared by the manufacturer is 140 L/min when using an FiO2 of 0.3.13 Gas flows of other settings and the effect of PEEP on gas flow are unknown.
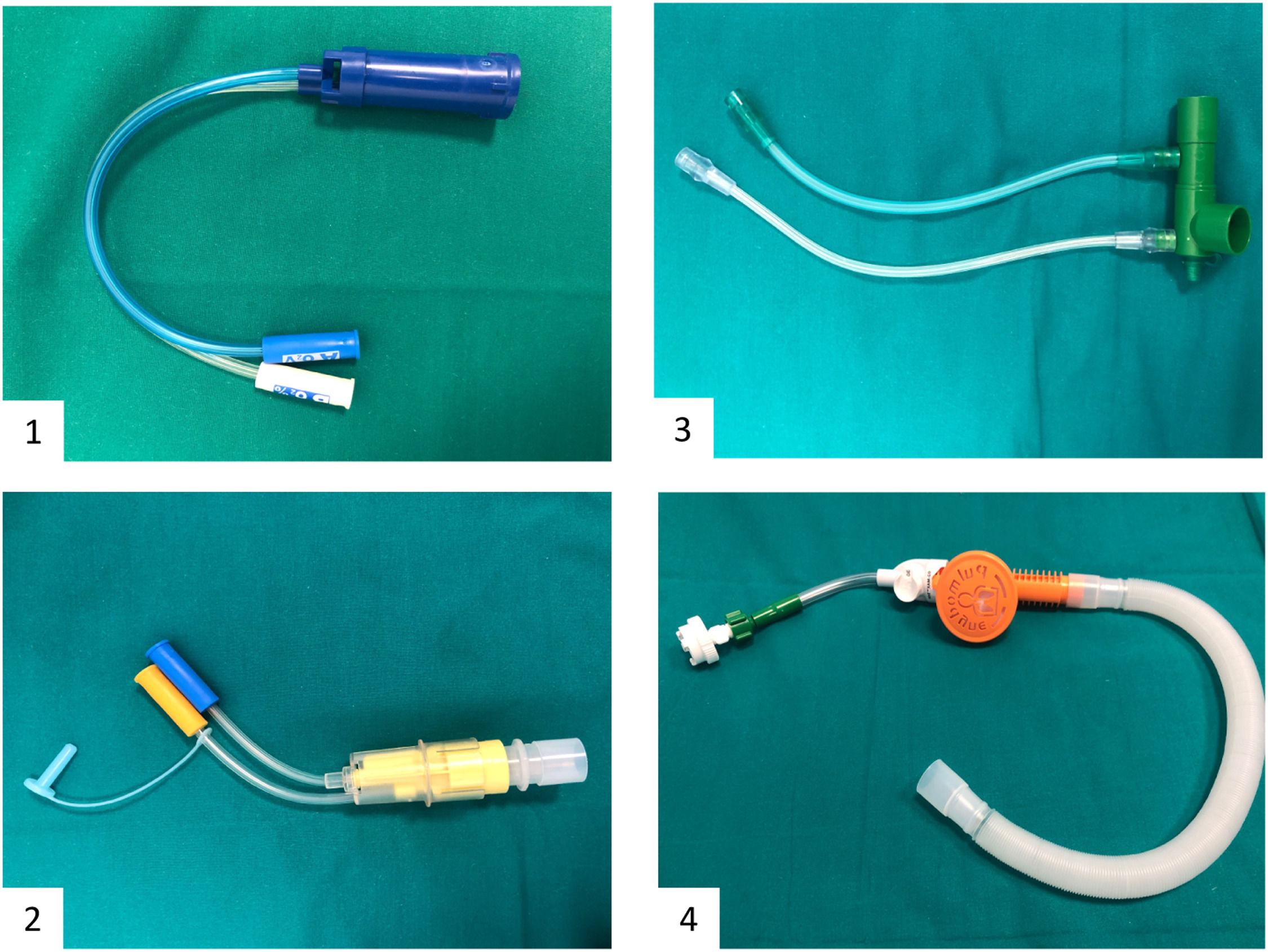
Full 5-L, 200 bar oxygen cylinders for a total of 1,000 L of oxygen were used. A double flow meter (Rs®, Flowmeter SpA, Bergamo, Italia) was connected to the standard AFNOR cylinder joint. This system has two columns capable of delivering a maximum of 15 L/min and 30 L/min of oxygen to Line-A and B, respectively (Fig. 2B). DEVICE-4 was connected directly to the tank via the AFNOR joint (Fig. 1.4). A full description of the experimental setup is provided in Fig. 2 and in the Supplementary Appendix (A-1).
As the first step, we evaluated the effectiveness of the four Venturi systems in delivering H-CPAP connected to an oxygen cylinder. For each double-inlet Venturi flow generator, the ability to generate pre-established clinically useful flow/FiO2 setups in the presence of three different PEEPs was tested. The oxygen source of Lines A and B was gradually opened to achieve a gas flow of either 60 or 80 L/min (SETUP 1 and 2, respectively), with FiO2 of 0.4-0.5-0.6, and PEEP of 7.5-10-12.5 cmH2O.
After achieving stable flows and FiO2 values, the amount of oxygen delivered to Lines A and B of each setup was recorded, generating a reference table. All measurements were performed with and without a heat and moisture exchanger (HME) filter interposed in the circuit. Indeed, while HME filters are widely used to muffle the noise inside the helmet improving patients’ comfort, they might reduce the flow, change the delivered FiO2 and PEEP.14–17
The flow delivered to Lines A, and B was set using the floating balls of the flowmeter columns. Due to their relatively low accuracy, to evaluate the bedside applicability of the reference table, three independent healthcare professionals working in the Emergency department were asked to reproduce each setting three times, following the rounded oxygen flow values of the reference table, blinded to the flow and the FiO2 delivered. The generated flow and FiO2 values were recorded and compared to the predetermined settings.
For DEVICE-4, the gas flow and FiO2 delivered of two of the three preset adjustable FiO2 levels (0.3 and 0.6) were tested, with a fixed PEEP of 10 cmH2O.
In the second step, the flow, FiO2, PEEP and tank pressure were evaluated during the progressive oxygen consumption of the cylinder. Only an initial flow rate of 80 L/min and a fixed PEEP of 10 cmH2O, combined with the lowest and highest FiO2 levels (0.4 and 0.6, respectively), were tested for DEVICE-1, 2 and 3. Similarly, for DEVICE-4, only two preset FiO2 (0.3 and 0.6) were analyzed. Flow, FiO2, PEEP, and tank pressure were recorded every minute until the exhaustion of the cylinder. PEEP and tank pressure were measured from the helmet-integrated and cylinder-integrated barometers, respectively. In all experiments, an HME filter was interposed in the circuit. The time during which a gas flow of at least 60 L/min could be maintained (i.e., the minimum flow required to safely deliver H-CPAP) was considered the clinically relevant duration of the cylinder. For each Venturi system and setup, the runtime of the cylinder with data on flow, FiO2, PEEP, and tank pressure was tested twice. Finally, the expected tank duration was calculated as: [tank pressure (Bar) x tank Volume (L)]/total amount of oxygen delivered from Line A and Line B measured at the beginning of the experiments. Of note, oxygen flow was considered, for the sake of the calculation, as constant.18
Statistical analysisData are presented as mean±standard deviation or median [interquartile range]. The normality of each distribution was assessed using the Shapiro-Wilk test. Continuous variables were compared using a t-test or paired t-test, or Mann-Whitney Test and Signed rank test, as appropriate. To test the ability of three operators to set the CPAP in the different prespecified settings, we pooled the flows and the related FiO2 measured within the helmet of the different operators together, regardless of the setting, and compared them to the preset ones. A p-value <0.05 was considered statistically significant. Analyses were performed with Stata statistical software (Stata Statistical Software, Release 16; StataCorp, College Station, TX, USA), and graphs were drawn using SigmaPlot v.12.0 (Systat Software, San Jose, CA).
ResultsEffectiveness of H-CPAPAmong the double-inlet Venturi flow generators, only DEVICE-1 and 2 connected to a single oxygen cylinder, were able to deliver H-CPAP with the preset gas flows, FiO2 and PEEP values. DEVICE-3 generated a maximum gas flow of 45 L/min and was thus excluded.
Without the interposition of an HME filter the oxygen flows were 0.4 [0.0, 1.1] L/min lower to ensure the same gas flow. Considering its proven benefit for the patient and the low O2 consumption it required, all subsequent analyses were conducted applying an HME filter.
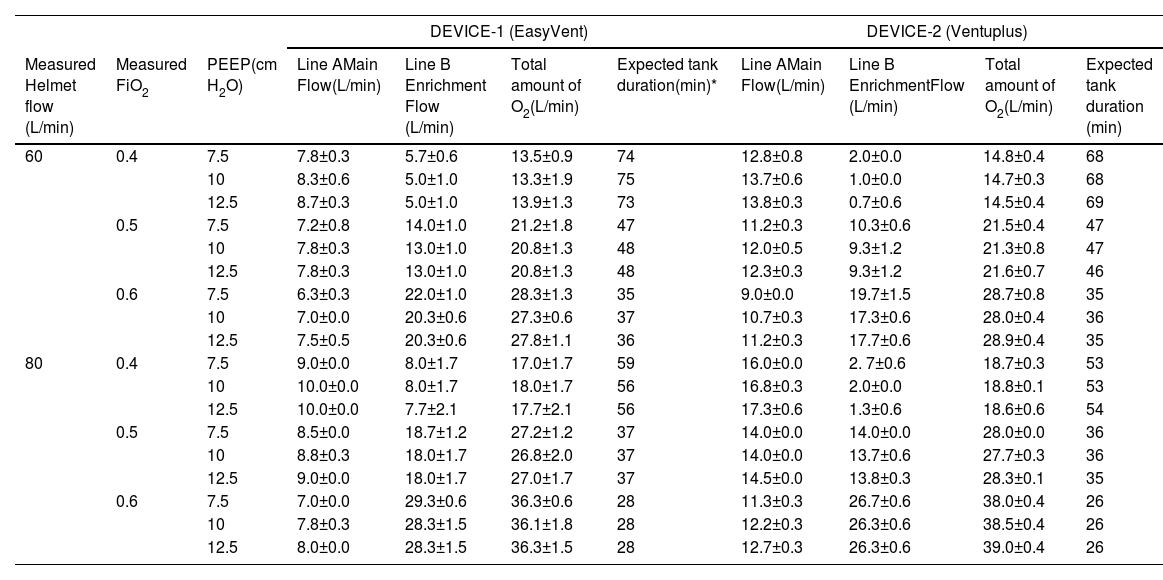
Table 1 summarizes the oxygen flows to Lines A and B required by DEVICE-1 and 2 in different setups to deliver H-CPAP. In addition, the expected tank duration is reported.
Effectiveness test. Oxygen flows with double-inlet DEVICE-1 and 2 at different setups with HME filter applied at the inlet port of the helmet.
Little differences were observed between the preset values and the flows delivered by the three different investigators, both with DEVICE-1 and 2. Of note, with the first the flows delivered were 2.0±1.9 L/min (p<0.001) and 0.8±1.9 L/min (p=0.03) higher, whereas with the second, they were 5.5±2.8 L/min (p<0.001) and 6.2±2.6 L/min (p<0.001) higher than the preset 60 and 80 L/min, respectively. Slight absolute differences were also observed for the FiO2 delivered: with DEVICE-1 −0.3±0.6% (p<0.001), −0.7±0.9% (p=0.006), and +1.5±0.9% (p<0.001), while for DEVICE-2: −0.7±0.6% (p<0.001), −1.8± 0.9% (p<0.001), −2.3±1.2% (p<0.001) as compared to basal FiO2 0.4, 0.5 and 0.6, respectively.
When DEVICE-4 was used, the interposition of an HME filter at the inlet port of the helmet reduced the delivered flow of 15.8±4.5 L/min (p<0.01), whereas FiO2 increased significantly (9±6%, p<0.01). For instance, with the 0.3 preset, the resulting delivered flow was 98.5±2.1 L/min with a measured FiO2 of 0.4±0.0, while with the 0.6 preset it was 90.5±0.7 L/min with a measured FiO2 of 0.85±0.7.
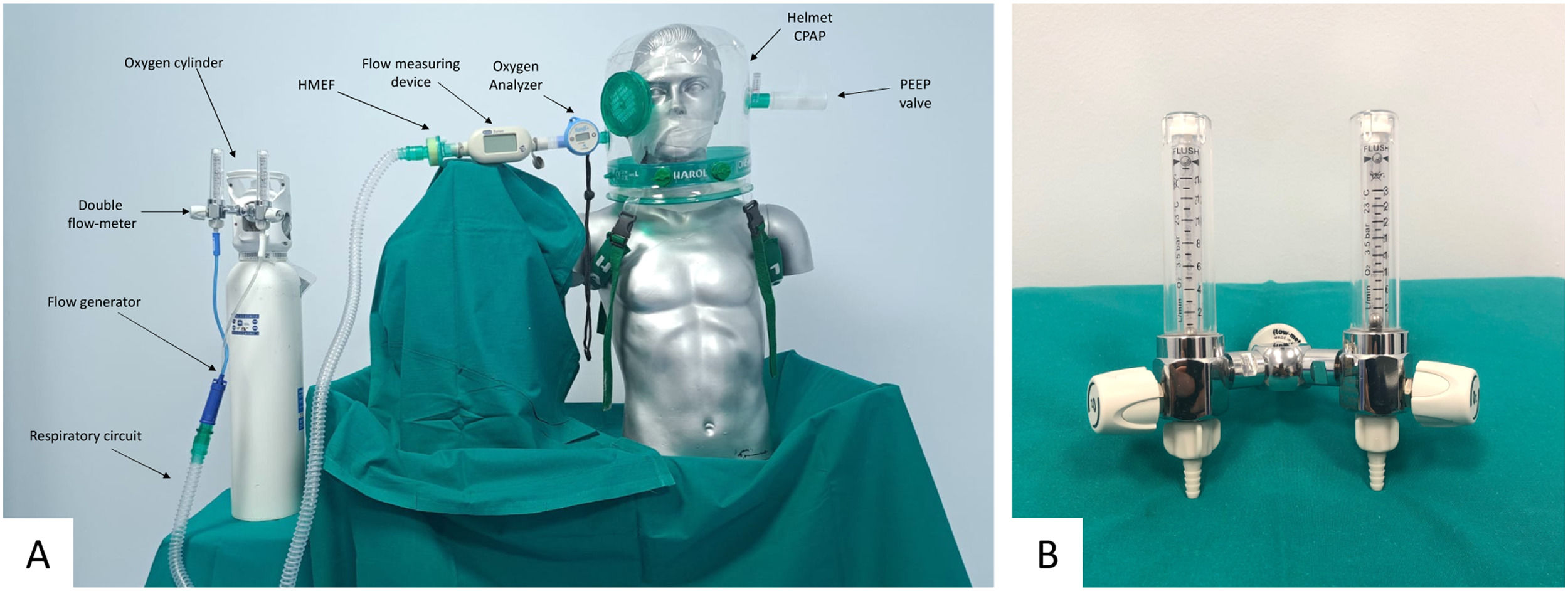
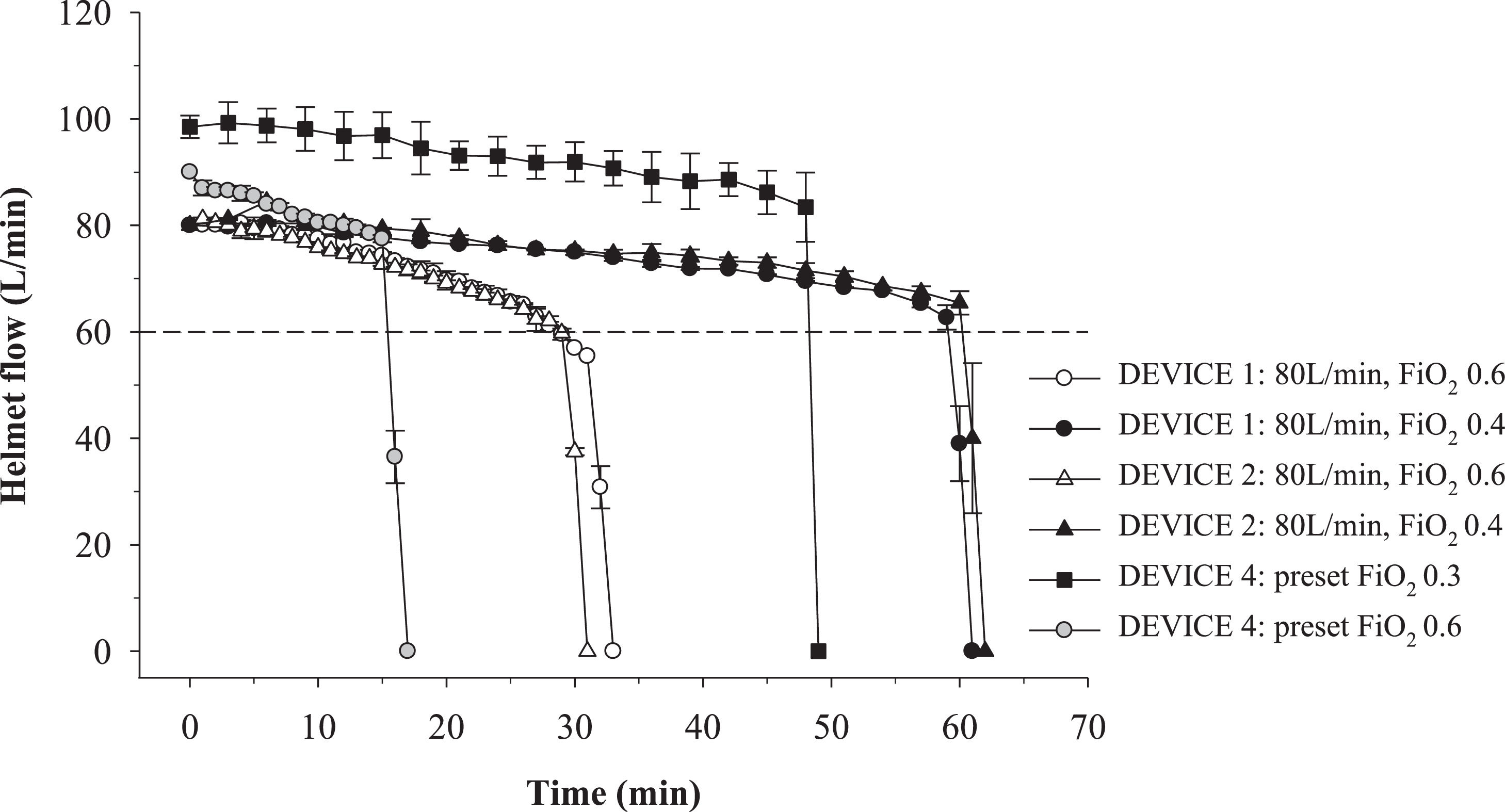
Efficiency in delivering H-CPAP: oxygen use and duration of the oxygen cylinderThe overall efficiency of Devices 1, 2 and 4 in terms of oxygen flow and minutes of H-CPAP delivered is reported in Fig. 3. Considering 60 L/min as the minimum threshold of flow required to deliver H-CPAP safely, the duration of H-CPAP with DEVICE-1 and DEVICE-2 with a preset flow of 80 L/min and FiO2 of 0.4 was 59 and 60 min, respectively. When FiO2 was increased to 0.6 (with the same flow), the duration was reduced to 28 min for both devices. When DEVICE-4 was tested with FiO2 of 0.3 and 0.6, the duration was 48 and 15 minutes, respectively.
Efficiency test: oxygen consumption and duration of the oxygen cylinder for different DEVICES and setups. DEVICE-4 generated a flow of 98.5±2.1 L/min and 90.5±0.7 L/min with a preset FiO2 of 0.4 and 0.6 respectively. DEVICE-1: EasyVent DEVICE-2: Ventuplus; DEVICE-3: Compact-HAR; DEVICE-4: O2-Max.
During the runtime of H-CPAP, together with a progressive fall of the pressure inside the oxygen cylinder, a progressive reduction in delivered flow was observed (Fig. 3 and Supplementary appendix, A-2). With both DEVICE-1 and 2, the drop was equal to 0.3 and 0.7 L/min for the FiO2 0.4 and 0.6 preset, respectively. For DEVICE-4, flow dropped 0.3 L/min with FiO2 0.3. The concomitant FiO2 variation was negligible. With both DEVICE-1 and 2, throughout the entire runtime of H-CPAP, the FiO2 ranged between 0.39 and 0.41 when FiO2 was set at 0.40, and between 0.58 and 0.62 when it was set at 0.6. With DEVICE-4, it ranged between 0.39 and 0.40 with the 0.3 FiO2 preset, and between 0.74 and 0.84 with 0.6 preset. PEEP remained stable until tank exhaustion.
DiscussionThe study's key findings are: first, H-CPAP can be delivered using portable Venturi devices connected to an oxygen cylinder reaching adequate gas flows, FiO2, and PEEP values. However, not all Venturi devices achieve these parameters. Indeed, DEVICE-3 was unable to deliver 60 L/min of gas flow. Compared to the other employed Venturi systems, in this device the gas flow and the O2 entrainment systems are perpendicular and not parallel to each other, thus probably decreasing the Venturi effect due to the generation of turbulence.
Second, when double-inlet Venturi devices are used, a double flowmeter allows the simultaneous delivery of high gas flows and FiO2 using a single oxygen tank, which is practical in out-of-hospital settings. Third, during the exhaustion of the cylinder the delivered gas flow decreases slightly, thus an initial flow >60 L/min should be set to ensure a safe flow until the cylinder is empty. Lastly, when a 5-L (or larger) full oxygen cylinder is used, the runtime of H-CPAP can be estimated and could be sufficient for out-of-hospital transport.
To the best of our knowledge, the use of a double flowmeter connected to a single oxygen tank represents a novel approach, allowing simple delivery of adequate gas flows and FiO2 when double-inlet Venturi devices are used. Setting the two oxygen flows using the floating balls of the double flow meter is straightforward, but could lead to variations among different operators due to its low accuracy.19 While no significant FiO2 differences were observed, the flows set by the three different investigators were slightly higher than the preset ones. There are two potential reasons for this: first, rounded values from Table 1 were used, as decimal flow could not be set. Additionally, the floating balls could be intentionally set at the upper limit of the notch, because the investigators were aware of the Venturi system and the importance of ensuring a higher rather than lower gas flow.
With a preset flow of 80 L/min, FiO2 0.4-0.6, and PEEP 10 cmH2O, the duration of H-CPAP using DEVICE-1 and DEVICE-2 were similar and varied according to the chosen FiO2. Although our study observed a shorter tank duration than a previous one,12 higher FiO2 values, suitable also for severe ARF, were delivered. During the progressive emptying of the tank, a slight and gradual flow drop was observed, followed by a sharp drop when it ran out. The gas flow drop was associated with the drop in cylinder pressure thanks to the pressure-reducing regulator connected to the cylinder.20 This information is new and has two implications in clinical practice. First, an initial preset flow >60 L/min should be used when delivering H-CPAP with an oxygen cylinder, to guarantee at least 60 L/min until the cylinder is empty. Second, given that the calculated expected tank duration does not consider the flow drop, it underestimates the cylinder duration, thus guaranteeing an additional safety margin.
Compared to the double-inlet devices, DEVICE-4 is directly connected to the oxygen tank and does not require a double flowmeter, thus being more practical. On the other hand, neither does it allow for adjustments of gas flow and FiO2, nor an accurate estimate of the O2 consumption. The 0.30 FiO2 preset generated a gas flow (98.5±2.1 L/min) for 48 minutes (with the 5-L oxygen tank), i.e., a clinically useful runtime. On the other hand, the 0.6 FiO2 preset, requiring more oxygen, lasted only 15 minutes.
The main limitations of our study are its bench design and the static conditions under which the tests were conducted. Experiments were conducted with a high pre-set gas flow (80L/min) able, in theory, to prevent carbon dioxide rebreathing and to maintain a stable positive airway pressure during the whole respiratory cycle. However, future studies are needed to assess the stability of CPAP in patients with high inspiratory efforts, a factor that was not considered in our experiments.21 Furthermore, in the last two years, new Venturi devices, with an adjustable venturi valve and a digital screen for flow and FiO2 settings, and new high-performance Turbine systems have been evaluated to deliver H-CAP, showing promising results.16,21 They are more expensive, bigger, and heavier than those evaluated in our study. Nevertheless, they might be applicable in out-of-hospital settings, and evaluating their performance when connected to an oxygen cylinder might be considered a topic of future research.
The strength and novelty of our study are the evaluation of the performance of four Venturi systems connected to a single oxygen cylinder in terms of gas flow, FiO2, and PEEP values. Despite the bench evaluation, the tests were performed to obtain clinically useful results, which will hopefully provide valuable insights for healthcare professionals.
ConclusionsH-CPAP can be delivered using portable Venturi devices connected to an oxygen cylinder. However, not all devices are suitable for delivering it effectively. A double flow meter connected to the oxygen cylinder allows to deliver high gas flow and FiO2 using a single tank. Considering the gradual flow decrease during the cylinder consumption, an initial flow rate higher >60 L/min should be set. The estimated duration of the tank runtime can be used with a margin of safety to plan patient transport.
Ethical disclosuresConsidering the bench design of the study, ethics committee approval was not necessary.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.



![1: DEVICE-1, EasyVent [Dimar. Medolla. Modena. Italy]; 2: DEVICE-2, Ventuplus [StarMed. Mirandola. Modena. Italy]; 3: DEVICE-3, Compact-HAR [Harol S.r.l. San Donato Milanese. Milan. Italy]; 4: DEVICE-4, O2-Max (Pulmodyne. Indianapolis. USA). Photographs taken by the authors with permission of the manufacturers. 1: DEVICE-1, EasyVent [Dimar. Medolla. Modena. Italy]; 2: DEVICE-2, Ventuplus [StarMed. Mirandola. Modena. Italy]; 3: DEVICE-3, Compact-HAR [Harol S.r.l. San Donato Milanese. Milan. Italy]; 4: DEVICE-4, O2-Max (Pulmodyne. Indianapolis. USA). Photographs taken by the authors with permission of the manufacturers.](https://static.elsevier.es/multimedia/25310437/unassign/S253104372300171X/v1_202310300432/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9znTMwFdb/TnkS0koegILxs=)
![A: Experimental setup. B: double flow meter [Rs®, Flow-meter SpA. Bergamo. Italia]. A: Experimental setup. B: double flow meter [Rs®, Flow-meter SpA. Bergamo. Italia].](https://static.elsevier.es/multimedia/25310437/unassign/S253104372300171X/v1_202310300432/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9znTMwFdb/TnkS0koegILxs=)