A 54-year-old caucasian male presented with cough and progressive asthenia.
Chest computed tomography showed discrete areas of subpleural reticulation, bronchiectasis, micronodules and mediastinal lymphadenopathies scattered in all stations suggesting sarcoidosis with fibrosis. Pulmonary function testing demonstrated a mild obstructive ventilatory defect and a moderate diffusion impairment.
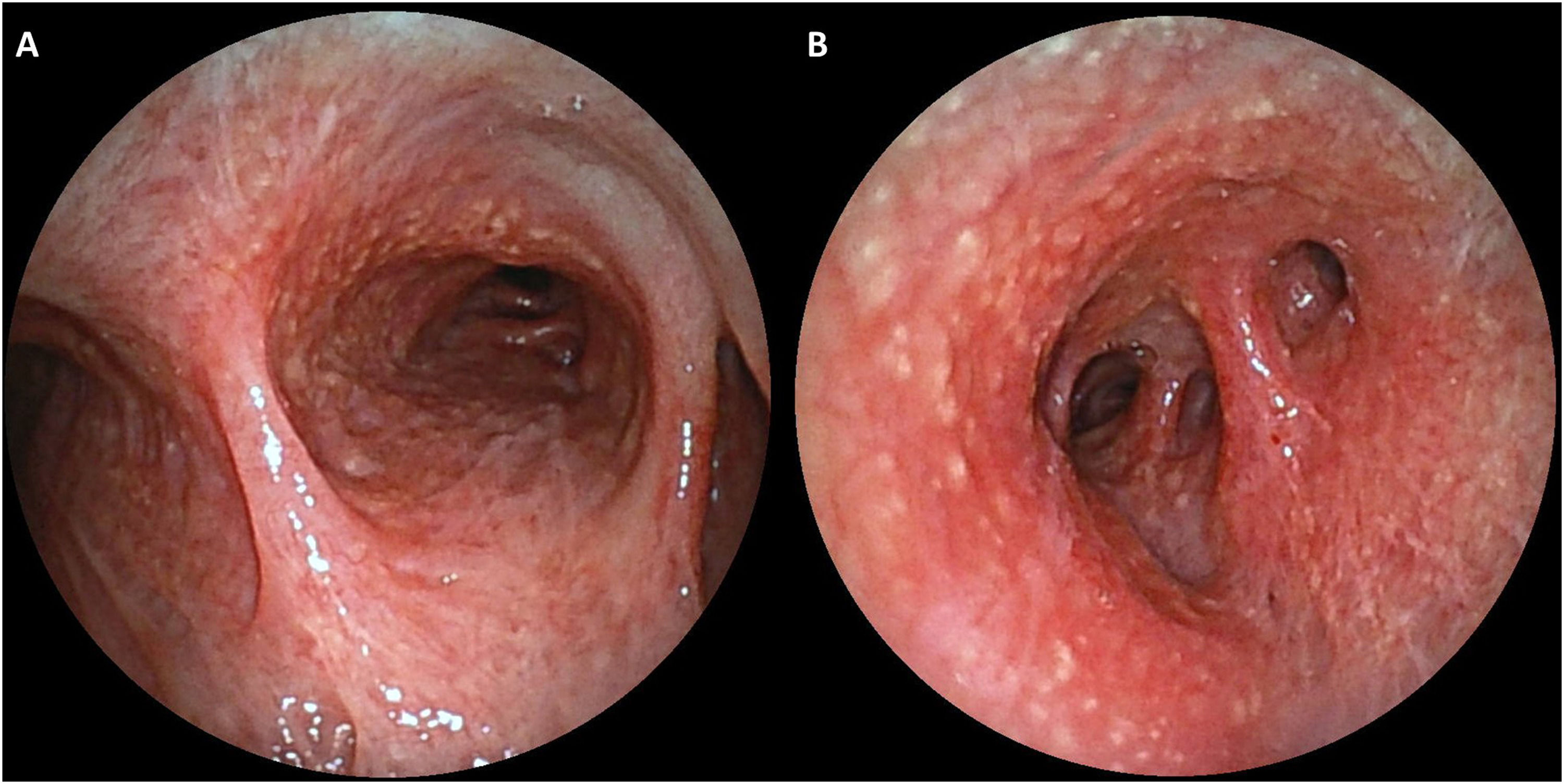
The patient underwent flexible bronchoscopy evidencing a diffuse hyperaemic mucosa with multiple white-yellow millimetric nodules distributed throughout the tracheobronchial tree, manifesting an exuberant cobblestone pattern (Fig. 1). The bronchoalveolar lavage showed a lymphocytic cellular pattern and CD4-to-CD8 ratio of 2.17.
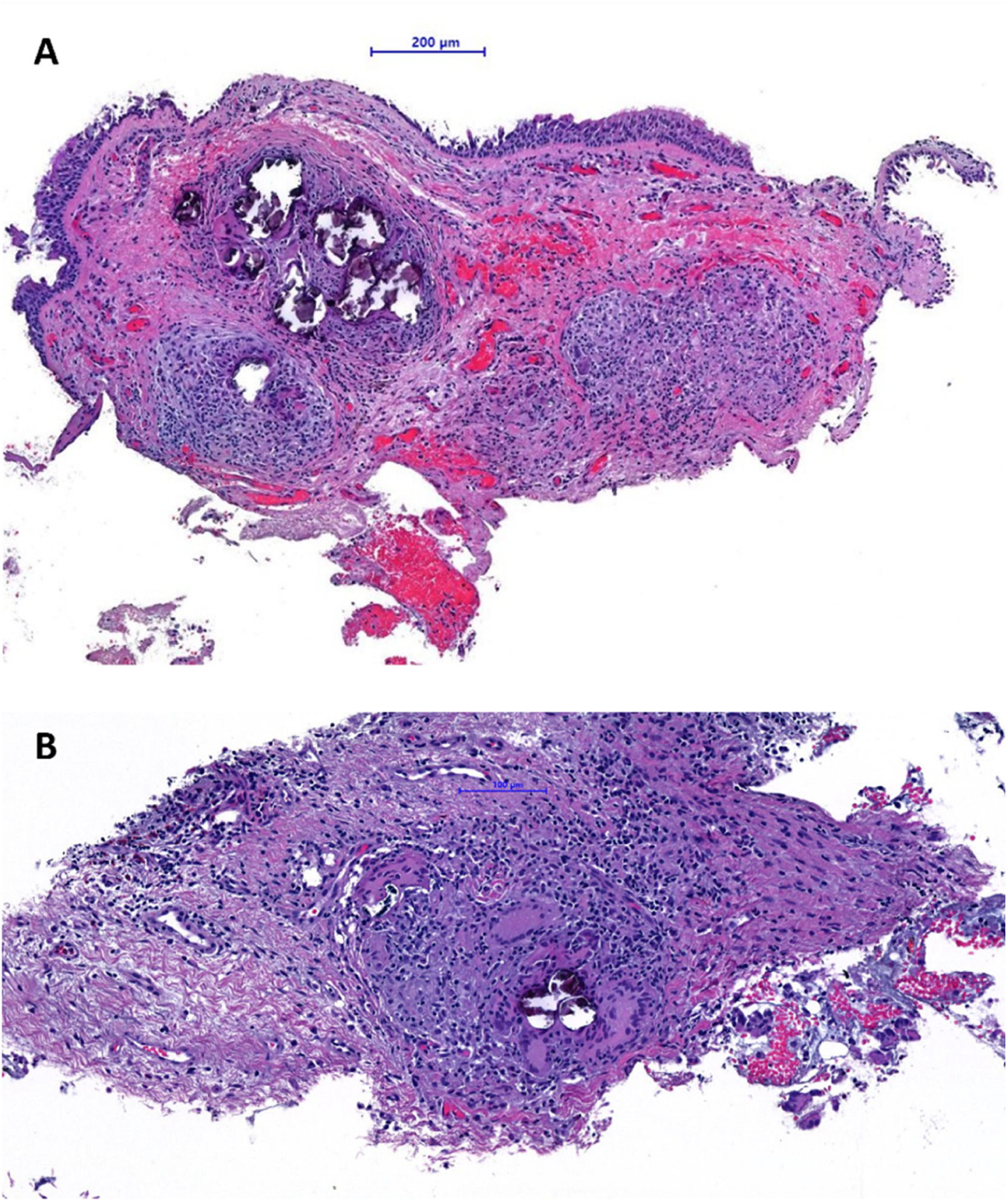
Histological examination of bronchial biopsies of the nodules demonstrated respiratory-type mucosa with chronic inflammatory process with non-necrotizing granulomas. Numerous multinucleated giant cells and abundant calcifications were identified, with no signs of malignancy (Fig. 2). An immunohistochemical study was conducted (amplification method by polymers - OptiView Dab IHC detection kit; automated technique – equipment: BencMark™XT Ventana Medical System) to look for: AE1AE3, p53, RE, thyroglobulin and TTF1. No expression of AE1AE3, p53, RE, thyroglobulin and TTF1 was observed.
Based on the clinical and radiographic findings, histologic pattern and exclusion of other causes, the diagnosis of sarcoidosis was established.1
The patient started treatment with 40 mg of prednisolone and has since shown symptom relief and cough resolution.
Although endobronchial sarcoidosis is described, its exact incidence in central airway is not known. In our patient, the unusual cobblestoning pattern was observed, which is considered a sentinel finding of advanced disease.2 In these situations, a biopsy should be performed to exclude other aetiologies (e.g. malignant and infectious).1
It's important to be aware of this form of presentation, given an early diagnosis, considering it implies increased respiratory symptoms and morbimortality.2
Unidade Local de Saúde da Guarda (Guarda, Portugal)
There were no external sources of funding.
The study was duly authorized by the Ethics Committee for Health of the institution where it took place, and the procedures were followed according to the regulations established by the Helsinki Declaration of the World Medical Association updated in 2013.