Chronic obstructive pulmonary disease (COPD) is a complex and heterogeneous disease, and there is a clinical need for validated markers and biomarkers that can contribute to the assessment of patients, risk prediction, treatment guidance, and assessment of response. Although according to the 2018 GOLD guidelines clinically useful biomarkers for COPD patients in stable condition have yet to be identified, several clinical markers and biomarkers have been proposed for COPD. These include isolated clinical markers, such as symptoms and Health Status assessment, exercise tests, function tests and imaging, and also composite scores and molecular markers.
However, and despite strong efforts to identify useful markers in an attempt to improve prognostic and therapeutic approaches, results have not been consistent and expectations of relying on these markers in near future are faint.
Current approaches to COPD have shifted from treating the disease to treating the individual patient. There is a clear need to identify treatable traits, focusing more on the patient and not on the disease, in order to implement an increasingly personalized treatment of COPD in the clinic, leading to true precision medicine. There is a need to identify combinations of clinical markers and biomarkers, genetic markers, and phenotypes that can guide the personalized therapy of COPD patients.
This critical review will therefore focus not only on currently established markers and biomarkers in COPD but also on possible future approaches toward precision medicine.
Over the last few years, numerous clinical and molecular markers of chronic obstructive pulmonary disease (COPD) have been identified, as well as phenotypes, in an attempt to improve prognostic and therapeutic approaches. However, results have not been consistent and expectations of relying on these markers in near future are faint.
There is a need to identify treatable traits,1,2 i.e., treatable characteristics of each individual patient, and to define which markers are most important. COPD is an unstable disease and markers may vary over time for the same patient. Moreover, given the complexity of COPD, it is unlikely that one isolated marker may guide therapeutic approaches or predict prognosis, but perhaps a combination of markers will be able to do so. It is also important to note, comorbidities occur frequently in COPD patients, including cardiovascular disease, skeletal muscle dysfunction, metabolic syndrome, osteoporosis, depression, and lung cancer.3 Given that they can influence mortality and hospitalizations independently, comorbidities should be actively looked for, and treated appropriately if present.3 A systematic review identified an association between the presence of co-morbid anxiety, obesity and osteoporosis, and possibly metabolic disease or depression, with reduced physical activity in COPD patients, highlighting the need to identify all co-morbid conditions present in these patients, in order to optimize treatment.4
This critical review will therefore focus not only on currently established markers and biomarkers in COPD but also on possible future approaches toward precision medicine.
Definition of marker and biomarkerThe concepts of marker and biomarker are different. A marker is defined as “a measurement that is associated with, and believed to be related pathophysiologically to a relevant clinical outcome”, whereas a biomarker has a more restrictive definition: “a measurement of any molecule or material (e.g., cells, tissue) that reflects the disease process”. Markers can be diagnostic, of disease severity or progression, and of treatment effect.5,6 A clinical outcome is defined as a consequence of the disease experienced by the patient, such as death, symptoms, exacerbations, weight loss, exercise limitation, and use of healthcare resources among others.5
Adequately validated biomarkers can contribute to improve patient care by (1) facilitating early detection of subclinical disease, (2) improving the diagnosis of acute or chronic syndromes, (3) stratifying patients’ risk, (4) selecting the most appropriate therapy for a given patient, and/or (5) monitoring disease progression and response to therapy.6,7
Since COPD is a complex and heterogeneous disease, there is a clinical need for validated biomarkers that can contribute to the assessment of patients, risk prediction, treatment guidance, and assessment of treatment response.6 Although according to the 2018 GOLD guidelines clinically useful biomarkers for COPD patients in stable condition have yet to be identified, several clinical markers and biomarkers have been proposed for COPD.
Clinical markersIsolatedClinical markers in COPD can be divided in four categories: (1) symptoms and Health Status assessment, (2) physical activity and exercise capacity, (3) function tests, and (4) imaging.
Symptoms and health status assessmentSeveral questionnaires exist for symptom and health status assessment of COPD, and the 2018 GOLD guidelines recommend the modified Medical Research Council (mMRC),3 the COPD assessment test (CAT),8 the Clinical COPD Questionnaire (CCQ),9 which allow for assessment of response to interventions, the Chronic Respiratory Disease Questionnaire (CRQ)10 and St. George's Respiratory Questionnaire (SGRQ).11 The mMRC only assesses the impact of dyspnea, but it is simple to use in clinical practice, relates well with other measures of health status, predicts future mortality risk,12 and is more discriminating with respect to 5-year survival than staging of disease severity using the ATS guideline.13 The importance of dyspnea as a predictor of poor survival is well substantiated.14 CAT or CCQ are short, practical, and easy to use in clinical practice, but patients prefer the CCQ since it reflects their status better than CAT.15 Of note, the classification of COPD according to the GOLD groups produced by the mMRC or CAT score is not identical.16 CAT may be used as a complementary tool in a patient's clinical assessment to predict COPD exacerbations, health status deterioration, depression, and mortality.17
CRQ and SGRQ are both lengthy and have scoring algorithms that are too complex to use in routine clinical practice.18 When used in isolation, these clinical markers may not be sufficient to accurately assess COPD. However, mMRC, CAT and CCQ are generally more useful in daily clinical practice while CRQ and SGRQ use is mainly restricted to clinical investigation. Nonetheless, these two latter questionnaires may be used once with every patient since they are very informative.
Physical activity and exercise capacityCOPD is clinically characterized by a pathological rate of decline in lung function with age, and, as a result, patients with COPD often complain of dyspnea and exercise intolerance, both of which not only interfere with the ability to perform the activities of daily life but also significantly impair quality of life (QoL). Specialists recommend that a minimum of 30min of moderate intensity daily physical activity, such as walking, are necessary to maintain fitness, and COPD patients not meeting this standard are considered insufficiently active.19,20
In COPD patients, exercise and physical activity influence exercise tolerance and muscle strength, QoL, dyspnea, number of days hospitalized and number of exacerbations.21,22 Studies have shown that physical activity and exercise in daily life is an important predictor of risk of hospital readmission and mortality in COPD patients.
Exercise capacity is the strongest element of disease severity and mortality and has shown a consistently stable association with lung function or dyspnea. For COPD patients the BODE index (body mass index [BMI], FEV1, dyspnea and 6-min walk distance) includes exercise capacity to predict and characterize severity of illnesses and mortality.23,24 Also, indexes of outcomes such as exercise capacity help to measure the risk of future outcomes and the absolute effects of treatment and, thereby, the benefits and damages of treatment. Unfortunately, exercise capacity and life style have probably been rarely tested and evaluated in the vast majority of COPD patients.
In a study that followed patients for 5 years, Vo2max was shown to be the best predictor of mortality, independently of FEV1 and patient age.25 In another study26 the 6min walk distance test (6MWT) was determined in patients with severe COPD. Over a 2-year period, survival increased progressively with increases in the 6MWD. Patients unable to walk 100m had a mortality rate approaching 90% at 1-year. Patients with similarly impaired airflow (as measured by FEV1) who were able to walk more than 400m had significantly higher survival. The study demonstrated that exercise capacity was a better predictor of mortality than both FEV1 and BMI. In clinical practice, a quick exercise capacity test will help physicians to assess patient status and adopt appropriate interventions.
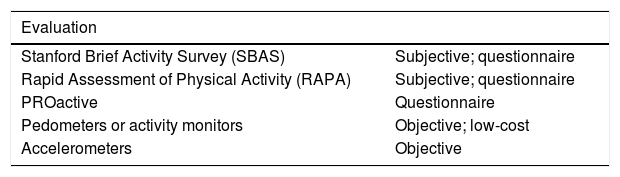
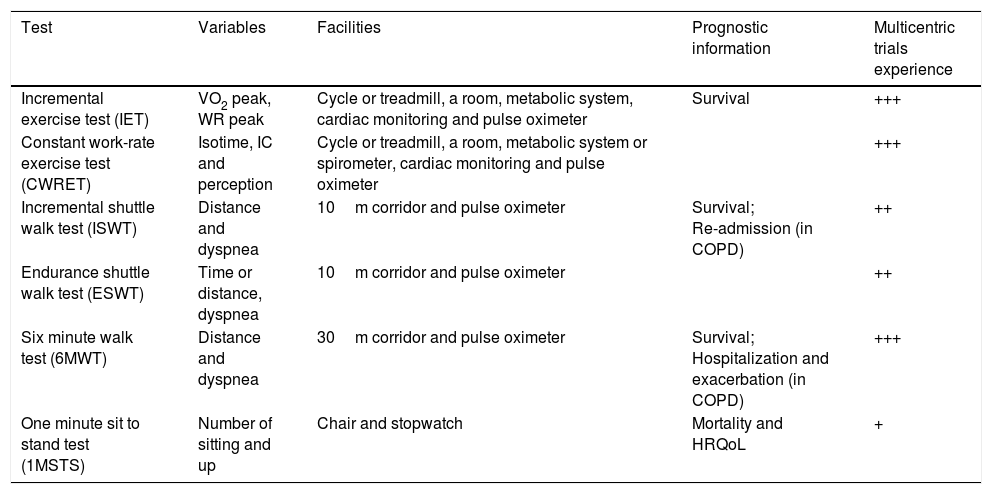
There are several methods to evaluate physical activity27,28 – Table 1. Exercise tests29 – Table 2 – are more objective to characterize COPD patients and predict prognosis, but are often not available outside rehabilitation or research settings. The severity and cause of exercise intolerance are best assessed by conducting standardized laboratory exercise testing in which detailed physiological measurements are taken while patients perform cycle ergometry or treadmill walking. Protocols can be either constant (“endurance”) or incremental. Simpler tests are also used, although the physiological information gathered is more limited: the 6MWT is relatively simple and has been used extensively; the incremental shuttle walk test (ISWT) and the endurance shuttle walk test (ESWT) are better standardized and have also been used in clinical trials. Endurance tests such as the constant work-rate exercise test (CWRET) and the ESWT are more responsive to interventions, both pharmacological and nonpharmacological, than incremental tests such as the incremental exercise test (IET), the ISWT, or the 6MWT. Although several tests exist to measure both the physical activity and the exercise capacity of COPD patients, there is a need for a reliable, simple test that all COPD patients are able to perform, and that is easy to apply in any office and by any doctor.
Characteristics of some physical activity assessment tests.
| Evaluation | |
|---|---|
| Stanford Brief Activity Survey (SBAS) | Subjective; questionnaire |
| Rapid Assessment of Physical Activity (RAPA) | Subjective; questionnaire |
| PROactive | Questionnaire |
| Pedometers or activity monitors | Objective; low-cost |
| Accelerometers | Objective |
Characteristics of selected exercise tests.
| Test | Variables | Facilities | Prognostic information | Multicentric trials experience |
|---|---|---|---|---|
| Incremental exercise test (IET) | VO2 peak, WR peak | Cycle or treadmill, a room, metabolic system, cardiac monitoring and pulse oximeter | Survival | +++ |
| Constant work-rate exercise test (CWRET) | Isotime, IC and perception | Cycle or treadmill, a room, metabolic system or spirometer, cardiac monitoring and pulse oximeter | +++ | |
| Incremental shuttle walk test (ISWT) | Distance and dyspnea | 10m corridor and pulse oximeter | Survival; Re-admission (in COPD) | ++ |
| Endurance shuttle walk test (ESWT) | Time or distance, dyspnea | 10m corridor and pulse oximeter | ++ | |
| Six minute walk test (6MWT) | Distance and dyspnea | 30m corridor and pulse oximeter | Survival; Hospitalization and exacerbation (in COPD) | +++ |
| One minute sit to stand test (1MSTS) | Number of sitting and up | Chair and stopwatch | Mortality and HRQoL | + |
In a study published by Puhan et al.30 the authors found that upper limb strength measured by the handgrip test and, in particular, by the one minute sit to stand test (1MSTS) as a measure of exercise capacity were strongly and independently associated with mortality and Health-Related (HR)-QoL over 24 months of observation. However, no significant associations with exacerbations have been found.
Although direct comparisons of the predictive ability of exercise tests are scarce, the current body of evidence suggests that the simpler 1MSTS, the 6MWT or the IET can be used to predict outcomes in COPD. In most practice settings, exercise tests are rarely performed with COPD patients because these tests require equipment, space and trained staff. It is this panel's opinion that the 1MSTS offers an attractive alternative. The 1MSTS seems to measure similar aspects of exercise capacity to the 6MWT31,32 and may be an attractive option with which to assess exercise capacity in COPD patients in both clinical practice and research.
Function testsA post-bronchodilator Forced Expiratory Volume in 1 second/forced vital capacity (FEV1/FVC)<0.70 confirms the presence of persistent airflow limitation and thus of COPD. FEV1 is an extremely important parameter in the prognosis evaluation, non-pharmacological therapeutic intervention, and for detecting COPD with rapid decline in lung function. An individual FEV1 patient level poorly expresses the disease status and is an unreliable marker of breathlessness severity, exercise limitation, and health status impairment.3 In COPD patients, FEV1 and symptoms/QoL are poorly correlated.33 Monitoring FEV1 trajectory, as a marker of disease activity, is more accurate than a single FEV1 measurement,34 and it may be a marker of uncontrolled disease.33 Frequent exacerbators show a faster decline of FEV1 when compared to infrequent exacerbators.35 Nevertheless, the FEV1 change rate is highly variable among COPD patients, with increased rates of decline among current smokers, patients with bronchodilator reversibility, and patients with emphysema,36 but an accelerated FEV1 decline is not inevitable in COPD.37
An inspiratory capacity-to total lung capacity (IC/TLC) ratio ≤25% seems to be a risk factor for COPD exacerbations38 and is a marker of mortality in COPD patients.39 IC/TLC is associated with reduced maximal strength and peak power output of patients’ lower extremities, suggesting that it may also be a marker of peripheral muscle dysfunction.40 IC/TLC as a continuum, predicts mortality in emphysematous COPD patients.41 In clinically stable COPD patients, IC/TLC and dyspnea can predict a decline of exercise capacity and may guide early therapeutic interventions.42
Hypercapnia is a marker of poor prognosis in COPD patients.43
Measurement of diffusing capacity for carbon monoxide (DLCO) provides information on the functional impact of emphysema in COPD and is often helpful in patients with breathlessness that may seem out of proportion with the degree of airflow limitation.3 DLCO is indicated for differential diagnosis in restrictive and obstructive diseases, disability assessment, evaluation of medication-associated toxicity, and prediction of exertional hypoxemia.44 Using the DLCO instead of a CT-determined emphysema, as has been done in the COPD-Lung Cancer Screening Score (COPD-LUCSS), has proven to be useful in identifying COPD patients at risk of death by lung cancer.45 DLCO may be more descriptive of systemic deconditioning than gas exchange in COPD patients.46 As for the assessment and follow-up of heavy smokers, the transfer coefficient of the lung for carbon monoxide (K[CO]) may be a useful tool because a lower baseline K(CO) is independently associated with a more rapid progression of emphysema and airflow limitation in this particular COPD population.47
Although not validated, hyperinflation increases as airway obstruction worsens,48 and can be present even in milder COPD during everyday activities.49 Hyperinflation increases acutely under conditions such as exercise or exacerbations, accompanied by a sharp increase in dyspnea intensity, leading to a vicious spiral of activity avoidance, physical deconditioning, reduced QoL, and early development of comorbidities such as cardiovascular disease.49 As hyperinflation provides more useful information pertaining to dyspnea and exercise tolerance than FEV1, it can be measured at any disease degree, aiding therapeutic decisions, particularly when there are discrepancies between clinical features and impairment of airflow obstruction.48
ImagingChest computed tomography (CT) is an important method for assessing lung conditions.48 CT supports the differential diagnosis and promptly identifies bronchiectasis.3 Thoracic high-resolution CT scan (HRCT) can be used to discriminate non-emphysematous and emphysematous COPD phenotypes.50 CT may help in early diagnosis of COPD, particularly by detecting air trapping from the analysis of inspiratory and expiratory images.48 Additionally, in case of a chest surgical procedure, such as lung volume reduction, a CT scan is necessary3 to determine emphysema distribution and surgical suitability.3 Moreover, emphysema distribution is a marker of COPD severity.51 CT and Magnetic Resonance Imaging (MRI) correlate pulmonary artery enlargement with right ventricular dysfunction.52 Additionally, in COPD patients, an elevated pulmonary artery to aortic ratio, as assessed by CT, is correlated with increased exacerbation risk, with this parameter outperforming other well established predictors of these events.53 Pulmonary hypertension is an independent risk factor of exacerbations and mortality in COPD patients, and CT seems to be useful in the assessment of these patients.54 CT can also be used to measure Epicardial Adipose Tissue (EAT) volume, which has been shown to be increased in COPD patients and is independently associated with smoking history, BMI and exercise capacity, all modifiable risk factors of future cardiovascular events. EAT volume could be a non-invasive marker of COPD patients at high risk for future cardiovascular events.55 Finally, CT is also required for patients being evaluated for lung transplantation. But a question remains: should a CT scan be performed on all COPD patients?
Composite scoresMulticomponent indexes incorporate several dimensions of COPD, and may provide physicians with a powerful tool to assess and monitor disease severity in order to guide decision making and improve patient outcomes. Other needs such as predicting healthcare utilization and risk stratification can also be studied with those tools in a COPD patient population.
The perfect index is yet to be established, but the most commonly used multicomponent indexes are BODE and its variations such as mBODE (BMI, FEV1, dyspnea and maximal oxygen uptake expressed as mL/min/kg) and BODEx (BMI, FEV1, dyspnea and exacerbations). In recent years, ADO (age, dyspnea and FEV1), DOSE (dyspnea, obstruction, smoking, exacerbation) and CID (Clinically Important Deteriorations) have also been used in COPD different scenarios. As expected, they are all better predictors of mortality than FEV1 alone. The BODE is considered to be the reference index: less complex than mBODE, better validated, with wider use18 and an excellent predictor of survival in patients with COPD.23,56 In patients with more severe disease, the use of BODE index is recommended57,58 as it seems to reflect COPD severity better than other multidimensional grading indexes.59
The need to perform the 6MWT renders BODE impractical in primary care and in less severe patients; in this setting it can be replaced by the BODEx index,60 as both indices show a high degree of correlation and a similar prognostic capacity for predicting mortality.58 When 6MWT data are not available, other validated options are the ADO or DOSE56 indexes. The ADO index is a better predictor of mortality compared to DOSE, but the DOSE index is better correlated with current symptoms and future risk for exacerbations and hospitalizations,56 a very important dimension in COPD. Whether prediction of mortality rates in patients using such indexes truly indicates patient-perceived severity and can guide appropriate treatment has been questioned, however, on the other hand, by measuring disease severity, they are useful in establishing prognosis and guiding therapy.18
Other indexes such as the COPD Prognostic index, that predicts mortality, hospitalization, and exacerbation frequency, and the SAFE (SGRQ, Air-Flow limitation and Exercise tolerance) index, which also predicts exacerbations, may also be useful.61 Very recently, a new composite measure has been proposed for COPD: CID. CID is defined as (1) a decrease of ≥100mL from baseline in trough FEV1, (2) a deterioration in HR-QoL defined as ≥4-unit increase from baseline in SGRQ total score, or (3) the occurrence of an on-treatment moderate-to-severe COPD exacerbation. CID has been used in clinical trials to evaluate therapeutic outcomes with excellent results.62,63
Some generic tools are available, such as the Charlson comorbidity index, which considers 17 comorbidities, and is an established predictor of mortality.4 Although it is the most common multimorbidity measure employed in medical populations,64 it does not include some important conditions in COPD, such as depression, anxiety and obesity, and does not evaluate other important health outcomes including QoL or health-care utilization,4 thus being a complex tool beyond the field of COPD.
In this area of growing evidence, this panel concludes that in a complex and heterogeneous disease such as COPD, the use of validated multicomponent indexes as BODE, BODEx, ADO, DOSE or CID, can contribute to the assessment of patients, risk prediction and treatment guidance, but all indexes need more evidence for a generic implementation.
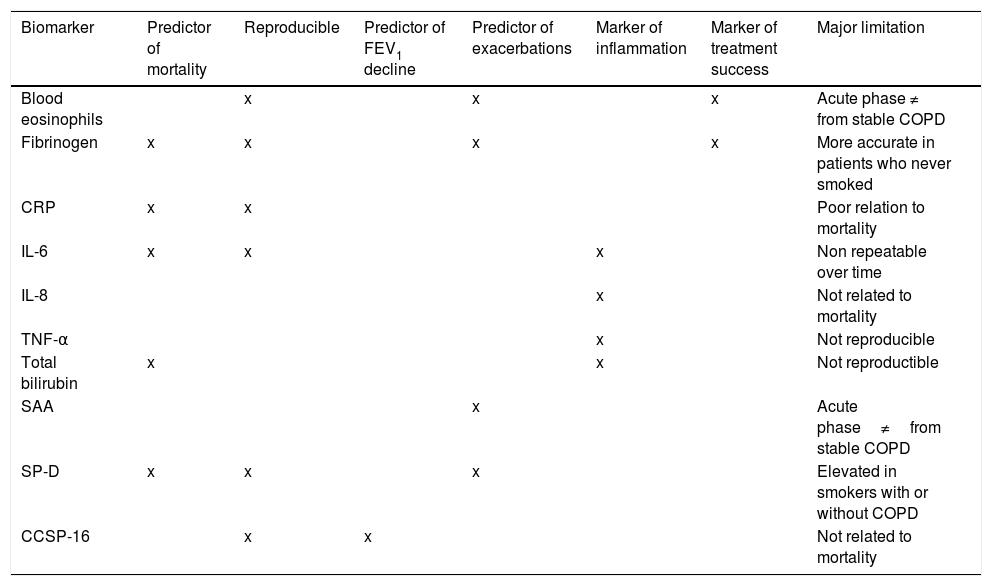
Molecular markersBiomarkers are extremely important in any disease provided they have diagnostic, prognostic or therapeutic value. In recent years, many analytical biomarkers have been explored in COPD, namely plasma fibrinogen,6,36,65 CRP,6,36,65–68 Interleukins IL-66,36,65,67,69 and IL-8,6,36,65,70 total bilirubin (important due to its antioxidant capacity),6 serum amyloid protein (SAA),6 surfactant protein D (SP-D),6,36,65 club cell secretory protein 16 (CCSP-16)6,36,65,71, and Matrix Metalloproteinases MMP-8 and MMP-9.65 In this review, we will only address those which either have been assessed in more studies for validation purposes or appear to be more relevant for COPD – Table 3.
Biomarkers which either have been assessed in more studies for validation purposes or appear to be more relevant for COPD.
| Biomarker | Predictor of mortality | Reproducible | Predictor of FEV1 decline | Predictor of exacerbations | Marker of inflammation | Marker of treatment success | Major limitation |
|---|---|---|---|---|---|---|---|
| Blood eosinophils | x | x | x | Acute phase ≠ from stable COPD | |||
| Fibrinogen | x | x | x | x | More accurate in patients who never smoked | ||
| CRP | x | x | Poor relation to mortality | ||||
| IL-6 | x | x | x | Non repeatable over time | |||
| IL-8 | x | Not related to mortality | |||||
| TNF-α | x | Not reproducible | |||||
| Total bilirubin | x | x | Not reproductible | ||||
| SAA | x | Acute phase≠from stable COPD | |||||
| SP-D | x | x | x | Elevated in smokers with or without COPD | |||
| CCSP-16 | x | x | Not related to mortality |
CRP, C-Reactive Protein; IL-6, Interleukin 6; IL-8, Interleukin 8; TNF-α, tumor necrosis factor α; SAA, serum amyloid protein; SP-D, surfactant protein D; CCSP-16, club cell secretory protein 16.
The most promising systemic/inflammatory biomarkers for predicting mortality in COPD are fibrinogen,3,43,67 IL-6,6,36,65,67,69 CRP,3,43,67–70 and total bilirubin.6
Plasma fibrinogen is the first biomarker drug development tool qualified for use in COPD under the FDA's drug development tool qualification program.72 High sensitive-CRP was the first biomarker to be investigated in COPD.
A recent genome-wide gene expression analysis from 229 ex-smokers from the ECLIPSE Study, identified novel, clinically relevant molecular subtypes of COPD. These network-informed clusters were more stable and more strongly associated with measures of lung structure and function than clusters derived from a network-naïve approach, and they were associated with subtype-specific enrichment for inflammatory and protein catabolic pathways. These clusters were successfully reproduced in an independent sample of 135 smokers from the COPDGene Study.73
Since oxidative stress may be an important amplifying mechanism in COPD,3 oxidative stress markers in sputum, namely malondialdehyde (MDA), hexanal, nonanal, acrolein, 8-isoprostane, nitrosothiols, 3-nitrotyrosine, and 8-hydroxy-2′-deoxyguanosine (8-OHdG)74 may be of interest in a nearby future. Hydrogen peroxide and 8-isoprostane are increased in the exhaled breath condensate, sputum, and systemic circulation of COPD patients, and oxidative stress further increases during exacerbations. There may also be a reduction in endogenous antioxidants in COPD patients as a result of reduction in the transcription factor Nrf2 that regulates many antioxidant genes.3 However, there is a clear disparity regarding oxidant-induced DNA damage and somatic mutations in COPD, which may reflect a difference in the oxidative stress per se or a deficient antioxidant and/or repair capacity in the lungs of patients.75
As for exhaled compounds being used as diagnostic markers, a very recent review concluded that reliable exhaled markers in COPD are still missing.76 The major challenges behind this are the heterogeneity in breath sampling technologies, the selection of appropriate control groups, and lack of sophisticated (and standardized) statistical data analysis methods.76 This was confirmed by a small study that showed that the biological meaning of exhaled and non-exhaled markers of respiratory inflammation in patients with COPD depends on the type of marker and the biological matrix in which it is measured.77
Given the above, the following question can be raised: should specific tests that include WBC, fibrinogen, PCR and, eventually, TNF-α, IL-8 and IL-6 be done in COPD patients? This panel agrees that the most important biomarkers to use in clinical practice are WBC, fibrinogen, IL-6 and PCR, with the remaining ones being restricted to use in a research setting. Therefore, the panel also agrees that the usefulness of the above mentioned biomarkers in routine assessments remains a matter of discussion and that currently available evidence does not allow for a conclusive proposal.
Peripheral eosinophilia has been proposed as a possible biomarker both for response to systemic corticosteroids during exacerbations and for predicting patients that will benefit from inhaled corticosteroids (ICS) in the stable state of COPD.
COPD patients with eosinophilia seem to benefit from systemic corticosteroids when exacerbating.78,79 Also, blood eosinophil levels of ≥200cells/μL and/or ≥2% of the total WBC count has been suggested as a biomarker in severe COPD exacerbations for predicting higher readmission rates.80 A cut-off of 3% in blood eosinophil counts as a proportion of the total WCB showed a sensitivity and specificity of 90% and 60%, respectively, for identifying an eosinophilic exacerbation. This was equivalent to an absolute count of approximately 230cells/μL. These authors have suggested considering using % in exacerbations and absolute counts in stable state.81
For patients in the stable phase of COPD, other studies have proposed different cut-off values. For example, two post hoc analyses of the WISDOM study suggested that patients with screening eosinophil blood levels ≥4% or ≥300cells/μL had lower exacerbation rates with continued ICS82 and that these same cut-off values might identify patients who will experience a deleterious effect from ICS withdrawal.83 In a post hoc analysis of two replicate RCTs comparing the efficacy in preventing exacerbations of once-daily inhaled fluticasone furoate plus vilanterol versus vilanterol alone,84 the following eosinophil cut-offs were evaluated: 0–2%, 2–4%, 4–6% and >6%. This post hoc analysis concluded that the benefits of ICS are observed for eosinophil counts greater than 2% and in a dose dependent manner, i.e., the higher the eosinophil count, the greater the reduction in exacerbation frequency with the ICS/LABA combination.85 However, all these studies are retrospective analysis, and many investigators have called for prospective randomized trials to confirm the predictive utility of blood eosinophils and to define a threshold.86
The FLAME study was the first prospective study evaluating eosinophilia as a biomarker of response to ICS-containing maintenance therapy. This study showed that indacaterol/glycopyrronium demonstrated a significant improvement in lung function compared with salmeterol/fluticasone for all eosinophil cut-offs tested (<2%, ≥2%, <300cells/μL and ≥300cells/μL).87 A subsequent post hoc analysis confirmed these results with more blood eosinophils cut-offs, namely <3%, <5% and <150cells/μL.88 A recent post hoc analysis of the WISDOM study further identified a subgroup of patients – patients with ≥2 exacerbations and ≥400cells/μL – that seem to be at increased risk of exacerbation when discontinued from ICS.89
The inflammatory response is extremely complex and involves the participation of numerous cell types and a myriad of inflammatory signals.6 Therefore, it is unlikely that a single biomarker can describe such complexity accurately.6,65,77
In conclusion, clinically useful biomarkers for stable COPD patients have yet to be identified,3 concerning diagnosis, disease activity or severity,33 disease progression,90 prognosis33,91 and response to therapy.34,90,92
Treatable traitsFEV1 is a marker of COPD severity and has historically been used to guide therapeutic choices. However, we now understand that the trajectory of FEV1 change, as an indicator of disease activity, is more important than a single FEV1 measurement.34 More importantly, we have moved from an airflow limitation FEV1-centric view of the disease to the understanding that COPD is such a complex and heterogeneous condition that it cannot be accurately captured by a single parameter. The complexity of this disease stems from its intrapulmonary and extrapulmonary components, whose dynamic interactions along time are not linear (for instance, exacerbations, symptoms comorbidities, etc.) and its heterogeneity from the fact that not all of these components are present in all individuals at any given point in time. This understanding inevitably leads to the need for personalized assessment and treatment of patients with COPD. There is a clear need to identify treatable traits, focusing more on the patient and not on the disease, in order to implement an increasingly individualized treatment of COPD in the clinic, leading to a true precision medicine.1 Precision medicine is defined as “treatments targeted to the needs of individual patients on the basis of genetic, biomarker, phenotypic, or psychosocial characteristics that distinguish a given patient from other patients with similar clinical presentations”.2 Indeed, there is a need to identify combinations of clinical markers and biomarkers, genetic markers, and phenotypes that can guide a personalized approach of COPD patients. The correlation genotype-phenotype-environment, or exposome, needs to be recognized.1 Guiding treatment solely based on clinical phenotyping is difficult, since a patient may display characteristics of more than one phenotype at the same time. Precision medicine integrates information based on the underlying pathobiological mechanisms of disease (defined as endotypes) and the clinical expression of such endotypes (defined as phenotypes)93 for a more patient-centered way to make therapeutic decisions and so maximize the benefit versus risk ratio. Endotypes can be identified via specific biomarkers but before being implemented in clinical practice, endotypes need to be better understood and their specific biomarkers fully validated.34,93 The final objective of precision medicine is to “improve clinical outcomes for individual patients while minimizing unnecessary side effects for those less likely to respond to a given treatment”.2
Conflict of interestIG declares to have received speaking fees from Novartis, AstraZeneca, Menarini and GSK. MJG declares to have received speaking fees from Genzyme, GSK, Novartis, A. Menarini, Philips, Vitalaire, Praxair and Linde, and to be an Advisory Board member of the Resmed iCARE group. MvZ declares to have received speaking fees from Novartis, Boeringher Ingelheim, AstraZeneca, Teva Pharma, Tecnifar, Praxair and Vitalaire. FM declares to have received speaking fees from Novartis, AstraZeneca, Menarini, Mundipharma, TEVA and Boehringer Ingelheim. JM declares to have received speaking fees from GSK, Novartis, AstraZeneca, Menarini, Mundipharma and Boehringer Ingelheim, and to be an Advisory Board member of GSK. PS declares to have received speaking fees from Novartis Farma, Boehringer Ingelheim, Munfipharma, AstraZeneca and Linde Saúde.
Role of Funding SourceFunding for this paper was provided by Novartis Portugal. Funding was used to access all necessary scientific bibliography and cover meeting expenses. Novartis Portugal had no role in the collection, analysis and interpretation of data, in the writing of the paper and in the decision to submit the paper for publication.